Constipation is exhausting, but lunch can actually help. These high-fiber sandwiches are built the way your gut prefers: sturdy whole-grain bread for gentle bulk, creamy legume spreads for steady fiber, seed “gel boosters” for softness, and juicy produce for moisture. Moreover, they’re practical—quick to assemble, easy to repeat, and sized to deliver meaningful fiber without feeling heavy.
Now, how much fiber do most adults need? A realistic daily target sits around 25–38 g. However, jumping there overnight can backfire. Instead, increase gradually—about 5 g extra per day each week—and pair each meal with fluids so fiber can actually hold water and move comfortably (see this concise intake overview and NIDDK hydration guidance). Meanwhile, short habits matter: drink a glass of water with your sandwich, then take a 10–15-minute walk. Little by little, those simple moves add up to relief.
Because details determine outcomes, every recipe below was designed with fiber grams, moisture, and texture in mind. In other words, the builds aren’t random—they’re engineered for comfort, regularity, and flavor you’ll actually crave tomorrow.
Also Read: Hemorrhoids High Fiber Diet: Best Foods, What to Avoid, and a 7-Day Plan
How much fiber these sandwiches deliver & of what kinds?
First, how much: each sandwich aims to contribute roughly 12–20 g of fiber toward your day. Which means, two thoughtfully built high-fiber sandwiches can cover most of what you need, leaving breakfast and snacks to top you up gently.
Second, which kinds: not all fibers behave the same, so the layers do different jobs.
- Viscous, soluble fibers make a soft gel that holds water in the stool, which often makes passing easier. You’ll get these from oats and barley (thanks to β-glucans), plus chia and ground flax (rich in mucilage). we have used oat/barley-leaning breads, avocado-chia mixes, and flax-boosted hummus throughout. If you’re curious about the mechanics, here’s a clear look at β-glucans and stool-softening and a friendly explainer on chia’s mucilage-rich fiber.
- Insoluble fibers—from bran, leafy greens, and vegetable skins—add gentle bulk and help speed transit. As a result, grated carrots, greens, and crunchy slaws live inside the sandwich, not just on the side, so every bite pulls its weight.
- Moisture is the multiplier. Because fiber needs water to work, spreads are creamy, fillings are juicy, and sauces are built in rather than left out. Additionally, we suggest sipping water with the meal, since fluids help fiber function.
Finally, how the recipes are structured: each sandwich states its intent (relief or maintenance), lists realistic portions, and includes make-ahead notes, smart swaps, and small finishing touches. Therefore, you can choose what fits today—and repeat it tomorrow—without turning lunch into a project.
Also Read: Prune Juice & Prunes for Constipation: What Works, How Much, and When to Seek Help
Why High-Fiber Sandwiches help (and how to build them)
Put simply, sandwiches make fiber doable. They bundle the right textures (soft + crisp), the right moisture (creamy + juicy), and the right amounts (measured slices and scoops) into a meal you can repeat tomorrow. Moreover, the format nudges consistency—arguably the most important factor for regularity.
They’re effortless to measure—and easy to stick with
Whole-grain slices are pre-portioned, spreads are spoonable, and veg layers are visible. Making it easy for you to assemble, eat, and actually hit useful daily fiber targets with minimal guesswork. If you like to prep once and assemble fast, this MasalaMonk idea for lentil meal-prep (as a sandwich filling) shows how a single batch can anchor multiple sandwiches during the week.
Moisture is built in by design
Dry, dense meals can backfire. We have ensured, each of these high-fiber sandwiches are built in a way that anchors moisture inside the bread: creamy hummus or yogurt-tahini underlayers, avocado folded with seeds, and juicy produce (carrot, greens, citrus segments) on top. That layering keeps bites slick rather than pasty, which, in turn, supports comfortable stool texture. If you like dairy or dairy-free yogurt as a base, a quick example is this hung curd spinach sandwich—the same idea powers our “Green Goddess” stack.
Layer order actually helps transit
Then start with a creamy spread to “seal” the crumb; next, add your fiber engine (chickpeas, lentils, or black beans) so it clings; in the end, finish with watery produce for slip. Additionally, a squeeze of lemon or a spoon of salsa adds acidity and fluid without heaviness. Small choices like these often determine whether a sandwich just sits—or genuinely supports movement.
Seeds add gentle gel—without bulky portions
A teaspoon of chia or finely ground flax disappears into spreads yet changes texture meaningfully after a glass of water. In brief, chia’s soluble, mucilage-rich fiber is well-documented (concise overview, open-access review; see also a broader nutrient profile in this MDPI review of chia’s composition: open access). For flax specifics you can use in everyday cooking, here’s a MasalaMonk primer: flax seeds for strong digestion.
The hand-held format supports satiety and travel
Because each of these high-fiber sandwiches pairs intact grains with legumes and produce, you get slower digestion and steadier fullness; which means, you’re less likely to graze later. For a clear big-picture explainer on fiber’s roles (beyond “roughage”), Harvard’s Nutrition Source summarizes the two fiber types and their effects.
Gentle routines amplify the effect
Right after eating, your body’s gastrocolic reflex naturally increases colon motility—so a brief 10–15-minute walk can nudge momentum in the right direction. For a plain-language primer, see Cleveland Clinic’s overview of the gastrocolic reflex. Moreover, even light movement supports regularity; their constipation guide underscores that exercise can stimulate the intestines. If symptoms persist despite these habits, the NIDDK’s constipation page outlines when to speak with a clinician.
Build template (at a glance)
- Bread (2 slices): 100% whole-grain or sprouted; look for ≥3–4 g fiber per slice.
- Spread (2–4 tbsp): hummus, white-bean mash, or yogurt-tahini; optionally stir in 1 tsp chia or ground flax.
- Engine (⅓–½ cup): chickpeas, lentils, or black beans; lightly mash so it anchors.
- Produce (heaped): grated carrot + leafy greens + a juicy element (cucumber, tomato, or citrus).
- Finish: lemon or vinegar splash; herbs; pepper. Additionally, sip water and, if possible, take a short walk afterward.
For background reading that ties food choices to gut comfort more broadly (in case you want to deepen the “why”), this MasalaMonk primer on gut inflammation and digestive health connects everyday plant foods with a calmer baseline—useful context for readers who like understanding the bigger picture.
Also Read: Teas for Digestion, Bloating, and Gut Health.
How to Use These High-Fiber Sandwiches
When constipation drags on, lunch is often the easiest place to add high fiber foods for constipation relief—without cooking an entire pot of anything. In practice, plant based foods high in fiber (beans, chickpeas, lentils, leafy greens) plus high fiber fruits and vegetables for constipation (kiwi, pear, apple, carrots) work together; as a result, you get both moisture and bulk. Along the way, foods rich in soluble fiber—like oats, barley, chia, and ground flax—form a gentle gel that supports softer stools and calmer bellies. Because you asked for a high fiber plant based diet approach, every sandwich below is fully plant-forward, practical for weekdays, and aligned with high fiber foods for gut health, colon health, and everyday digestive health. For hydration cues that make this even easier, see NIDDK’s diet & constipation guidance; for grain choices that add viscous fiber, here’s a friendly β-glucan overview.
Format you’ll see below: brief “why,” a clear ingredient list, step-by-step method, fiber-forward upgrades, and make-ahead tips—so these fiber rich foods for bowel movement become an easy habit, not homework.
1) Hummus–Kiwi–Greens “Softener” — flagship of High-Fiber Sandwiches (Relief)
Estimated fiber: ~17 g • Taste & texture: cool, fresh, silky
When to choose it: stools feel dry; you want gentle moisture without heaviness
Why it works (quickly yet gently)
This is a purpose-built combo of foods that are rich in soluble fiber and high fiber fruits for constipation. Specifically, creamy hummus (legumes = plant based foods high in fiber) and a teaspoon of ground flax (mucilage) create a moist base; then, thin-sliced kiwi and a mound of grated carrot supply juicy volume. Resulting in every bite that stays soft, which supports easier bowel movements and overall gut health. If you’d like a plain-English primer on adding flax safely, skim flax seeds for strong digestion; if you prefer the science on chia/flax-style gels, here’s a concise chia fiber review for later.

Ingredients (serves 1)
- 2 slices 100% whole-grain bread (≥3–4 g fiber/slice; oats or barley in the mix add foods rich in soluble fiber)
- Hummus, 4 tbsp (legume base = high fiber foods for digestive health)
- Ground flaxseed, 1 tsp (stirred into the spread)
- Kiwi, 1 medium, thin-sliced (one of the most convenient high fiber fruits for constipation)
- Baby spinach, big handful (leafy greens = fiber rich foods for gut health)
- Carrot, finely grated, ½ cup (insoluble lift for bowel movement comfort)
- Lemon juice, black pepper, tiny pinch of salt
Method
- In a small bowl, whisk lemon into the hummus; then stir in ground flax until creamy.
- Spread the mixture edge-to-edge on both slices; afterwards, pile on spinach, layer kiwi, and shower with grated carrot.
- Season with pepper and a pinch of salt; and then, close gently and press once with your palm.
Fiber-forward upgrades (choose 1–2, not all)
- Add 2–3 tbsp chickpeas into the hummus; which will make you push the legume count higher for a plant based high fiber diet day.
- Scatter 1 tsp chia over the carrot before closing; helping you nudge the soluble fiber profile without adding bulk.
- Swap bread for a dense oat-bran or barley loaf to increase β-glucans (i.e., foods rich in soluble fiber)—see β-glucan basics.
Make-ahead & serving
- Grate carrot the night before; store sealed so it stays juicy.
- Assemble within 10 minutes of eating (kiwi looks and tastes brightest right away).
- Serve with a full glass of water; thus, the high fiber foods to ease constipation you just ate can actually hold fluid as intended.
- On very sensitive days, replace raw spinach with tender arugula for similar benefits and gentler texture.
Why it fits the brief
This sandwich champions high fiber foods for constipation relief without heaviness—because moisture, viscosity, and volume are layered on purpose. In turn, you’ll notice comfort during the afternoon rather than bloat
Also Read: Peppermint Tea for IBS and Bloating: Natural Relief Backed by Tradition
2) Lentil “Sloppy-Joe” Toastie — cozy High-Fiber Sandwich (Relief with staying power)
Estimated fiber: ~19–20 g • Taste & texture: warm, savory, cohesive
When to choose it: you need relief and long-lasting satiety
Why it works (comfort + momentum)
Here you combine two plant based foods high in fiber—a white-bean mash and saucy lentils—with a crunchy layer of broccoli slaw. Which helps you get soluble-leaning moisture from tomato-braised lentils and insoluble lift from brassica shreds. Because the filling is warm and glossy, this tastes indulgent; nevertheless, it is textbook high fiber foods for bowel movements, colon health, and all-day digestive health. Prefer batch cooking? This lentil meal-prep filling anchors several sandwiches across the week—convenient for a high fiber plant based diet.

Ingredients (serves 1)
- 2 slices sprouted-grain bread (≥3–4 g fiber/slice; excellent high fiber foods for gut health)
- White-bean mash, 3 tbsp (blend white beans + lemon + olive oil + pinch salt)
- Cooked lentils, ½ cup (core legume in any plant based high fiber diet)
- Broccoli slaw, ½ cup (insoluble crunch from stems + a little prebiotic fiber)
- Tomato paste, onion, garlic, smoked paprika, olive oil, splash vinegar (for sauce)
Method
- Warm a small pan; sauté onion and garlic until tender; then add tomato paste and smoked paprika.
- Stir in lentils with 2–3 tbsp water and a splash of vinegar; simmer 3–4 minutes until thick, glossy, and spoonable.
- Spread white-bean mash on both bread slices; afterwards, pile on the lentils; then crown with broccoli slaw.
- Press in a grill pan or sandwich press 2–3 minutes per side until toasty outside and steamy inside.
Fiber-forward upgrades (pick what fits your day)
- Fold 1 tsp ground flax into the bean mash; in practice, you add foods that are rich in soluble fiber without changing flavor.
- Replace one slice with an oat-bran slice for extra β-glucans (again, high fiber foods for colon health).
- Add 2 tbsp grated carrot to the slaw for more insoluble volume (i.e., fiber rich fruits and vegetables for constipation in practice).
Make-ahead & serving
- Simmer a bigger batch of lentils on Sunday; cool quickly and refrigerate up to 4 days (or freeze flat in bags).
- Keep slaw dry until assembly so it stays crisp; alternatively, dress slaw lightly with lemon just before toasting.
- Serve with a sliced apple or pear (skin on): those are easy fiber rich fruits for constipation that travel well.
- Hydrate alongside; that helps the sandwich’s foods rich in soluble fiber can do their gel-forming job.
Why it fits the brief
Because it layers legumes two ways, this toastie moves from “filling” to truly high fiber foods to ease constipation. Moreover, it stays moist, which many readers find is the missing piece in at-home “healthy” & high-fiber sandwiches.
Also read: The Ultimate Guide to Lentils: Types, Benefits, and Recipes
3) Barley–Chickpea “Salad” Sandwich — herby High-Fiber Sandwich (Maintenance)
Estimated fiber: ~17 g • Taste & texture: cool, herby, packable
When to choose it: you want balance, not “power relief,” especially on workdays
On days you want reliability rather than “power relief,” this build blends foods rich in soluble fiber (barley’s β-glucans) with legume bulk from chickpeas. Consequently, you get a gentle gel plus comfortable volume—exactly what high fiber foods for digestive health should deliver. If you’re curious about the science behind β-glucans and softness, here’s a clear overview.
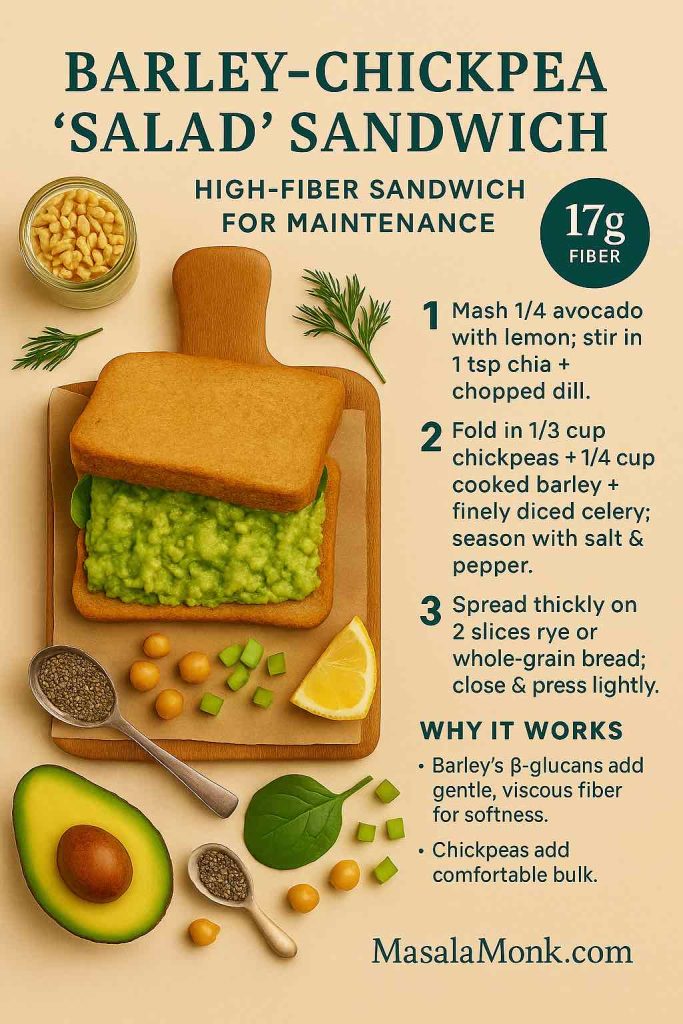
Ingredients (serves 1)
- 2 slices rye or 100% whole-grain bread (≥3–4 g fiber/slice; supports high fiber foods for gut health)
- Avocado, ¼ fruit, mashed (creamy base for moisture)
- Chia seeds, 1 tsp (disappears into the mash; classic foods rich in soluble fiber) — background: chia’s mucilage review
- Cooked chickpeas, ⅓ cup (plant based foods high in fiber)
- Cooked barley, ¼ cup (β-glucans for stool comfort)
- Celery (finely diced), dill, lemon, pepper, small pinch salt
Method
- Mash avocado with lemon; then stir in chia and chopped dill until glossy.
- Fold in chickpeas, barley, and celery; afterwards, season to taste.
- Spread thickly; after that, close and press lightly for a tidy, travel-worthy sandwich.
Fiber-forward upgrades
- Add 2 tbsp grated carrot for extra insoluble lift—useful among high fiber fruits and vegetables for constipation.
- Swap one slice for an oat-bran slice to nudge β-glucans (again, foods rich in soluble fiber).
- For herb lovers, a handful of parsley adds polyphenols without changing fiber math.
Make-ahead & serving
- Mix the filling up to 48 hours ahead; which means, weekday assembly takes 2 minutes.
- Serve with apple slices (skin on) for simple fiber rich fruits for constipation and satisfying crunch.
- Sip water alongside; therefore, the sandwich’s soluble fibers can actually do their job.
Why it fits the brief
This is a dependable high fiber plant based diet lunch: creamy, not dry; hearty, not heavy; and quietly supportive for bowel movements, colon health, and long-term gut health.
Also Read: Chickpeas’ Instead of ‘Sardines’: 5 High Protein Plant-Based Meal Prep Ideas
4) Pear–Walnut “Green Goddess” Stack — bright High-Fiber Sandwich (Gentle maintenance)
Estimated fiber: ~12–13 g • Taste & texture: juicy, herb-bright, light
When to choose it: you want support without heaviness
Why it works (light yet helpful)
Some days you want a lift without intensity. Here, juicy pear (skin on) brings pectin, leafy greens add volume, and a yogurt-tahini herb sauce keeps everything moist. Ultimately you get high fiber foods for constipation relief that feel bright rather than dense—ideal for easy digestive health.

Ingredients (serves 1)
- 2 slices oat-bran or whole-grain bread (≥3–4 g fiber/slice)
- Yogurt-tahini-herb sauce (yogurt + tahini + lemon + herbs)
- ½ pear, thin-sliced, skin on (simple high fiber fruits for constipation)
- Arugula or spinach, big handful (fiber rich foods for gut health)
- Walnuts, 1 tbsp (pleasant crunch)
- Lemon zest, black pepper
Method
- Whisk yogurt, tahini, herbs, and lemon until creamy; then spread generously.
- Layer pear, greens, and walnuts; afterwards, finish with zest and pepper.
- Close gently; press once to set the layers.
Fiber-forward upgrades
- Add thin cucumber or tomato slices for extra juiciness (i.e., high fiber fruits and vegetables for constipation that also boost moisture).
- Stir 1 tsp ground flax into the sauce to tilt toward foods rich in soluble fiber—basic primer: flax for digestion.
- Prefer curd? The texture tactic mirrors this hung curd spinach sandwich.
Make-ahead & serving
- The sauce keeps 3–4 days; making weekday builds stay fast.
- Serve with a small bowl of berries for additional fiber rich fruits for constipation that don’t weigh you down.
- Drink water; subsequently, the pectin and seed gels work more comfortably.
Why it fits the brief
Although gentle, the stack still qualifies as high fiber foods for bowel movements, and, importantly, it supports colon health without the heaviness that sometimes derails weekday lunches.
Also Read: Bananas for Constipation: Ripe vs Green, Timing & What Works
5) Black Bean–Avocado Salsa Melt — cozy High-Fiber Sandwich (Relief + comfort)
Estimated fiber: ~18.5–19 g • Taste & texture: warm, saucy, satisfying
When to choose it: you need soothing relief and an easy win at dinner
Why it works (warm, saucy, effective)
This is comfort food with a purpose. Black beans (core to any plant based high fiber diet) supply both soluble and insoluble fiber; avocado keeps things lush; and fresh salsa provides juicy acidity so the sandwich never feels dry. Meaning, you get high fiber foods to ease constipation that also satisfy.
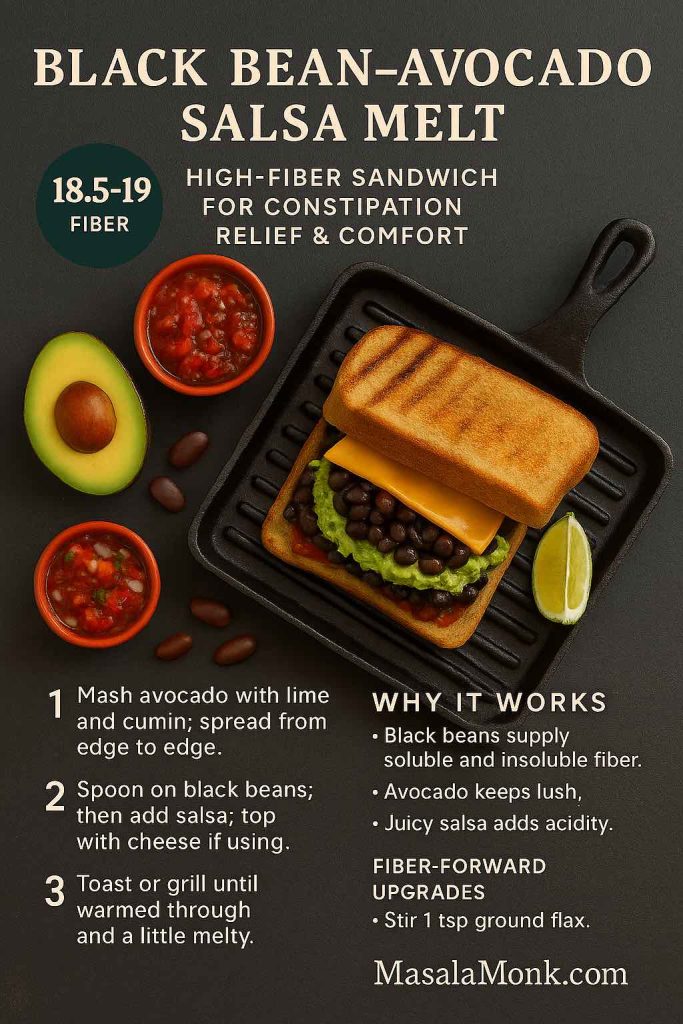
Ingredients (serves 1)
- 2 slices sprouted-grain bread (≥3–4 g fiber/slice; great for high fiber foods for gut health)
- Avocado, ¼ fruit, mashed
- Black beans, ½ cup (lightly mashed so they cling)
- Fresh tomato-onion salsa, ¼ cup (or tomato-lime if onion-sensitive)
- Optional: thin slice cheddar or plant cheese
- Lime, cumin, pinch salt
Method
- Mash avocado with lime and a pinch of cumin; spread from edge to edge.
- Spoon on black beans; then add salsa; top with cheese if using.
- Toast or grill until warmed through and a little melty.
Fiber-forward upgrades
- Stir 1 tsp ground flax into the avocado to lean toward foods rich in soluble fiber.
- Add 2 tbsp grated carrot for extra insoluble support (a staple among high fiber fruits and vegetables for constipation).
- Swap one slice for oat-bran bread to increase β-glucans.
Make-ahead & serving
- Beans keep 3–4 days; meanwhile, mash just before assembly for best texture.
- Serve with orange segments or cucumber spears; which makes you add fluid and crunch that amplify results.
- Hydrate; in turn, these fiber rich foods for bowel movement do their job more comfortably.
Why it fits the brief
It’s a weeknight win: cozy, fast, and firmly in the lane of high fiber foods for colon health and everyday digestive health.
Also Read: 10 Creative Chia Pudding Recipes for Every Taste
6) Tempeh–Kimchi Gut-Health Reuben — tangy High-Fiber Sandwich (Maintenance + microbiome)
Estimated fiber: ~14 g • Taste & texture: savory-tangy, deli-style
When to choose it: things are moving, and you want to keep the gut ecosystem happy
Why it works (tangy and sustaining)
Once things are moving, pairing plant based foods high in fiber with fermented vegetables is a smart way to maintain momentum. Tempeh offers satisfying protein and fiber; kimchi or sauerkraut adds acidity, moisture, and live cultures; as a result, you get high fiber foods for gut health in a deli-style package. For more combinations, browse Probiotic-Rich Sandwiches.

Ingredients (serves 1)
- 2 slices whole-grain rye (≥3–4 g fiber/slice)
- Tempeh, ~100 g, sliced and sautéed
- Kimchi or sauerkraut, ¼ cup
- Spinach, big handful
- Yogurt-mustard (or a dairy-free version)
Method
- Sear tempeh in a thin film of oil until browned; then set aside.
- Spread yogurt-mustard on bread; afterwards, layer tempeh → kimchi → spinach.
- Grill lightly to warm and meld the layers.
Fiber-forward upgrades
- Add thin tomato slices for juicy slip (handy within high fiber fruits and vegetables for constipation).
- Stir 1 tsp chia into the yogurt-mustard for a small soluble nudge (again, foods that are rich in soluble fiber).
- Prefer milder ferments? Use kraut and a dab of pickle brine for acidity without heat.
Make-ahead & serving
- Cook tempeh 2–3 days ahead; consequently, weekday assembly is trivial.
- Serve with carrot sticks and apple wedges (skin on) for easy fiber rich fruits for constipation and crunch.
- Water alongside, then a brief walk; helping the meal support predictable bowel movements.
Why it fits the brief
This one keeps the momentum you’ve built—supporting colon health and digestive health while staying firmly in the high fiber plant based diet lane.
Also Read: Optimize Digestion with These 5 Fruit Juice Recipes
Sidekicks that make High-Fiber Sandwiches even more effective
Kiwifruit (1–2/day)—slice one into Sandwich #1 and enjoy the second on the side. Trials show kiwi improves bowel movements and overall comfort (kiwi RCT overview; gold-kiwi RCT).
Prunes or prune juice—start with 4–6 prunes or ½–1 cup prune juice alongside lunch or dinner. Practical “how much/when” is covered here: prune juice & prunes for constipation. For clinical context, review the trial where prunes beat psyllium in mild–moderate cases.
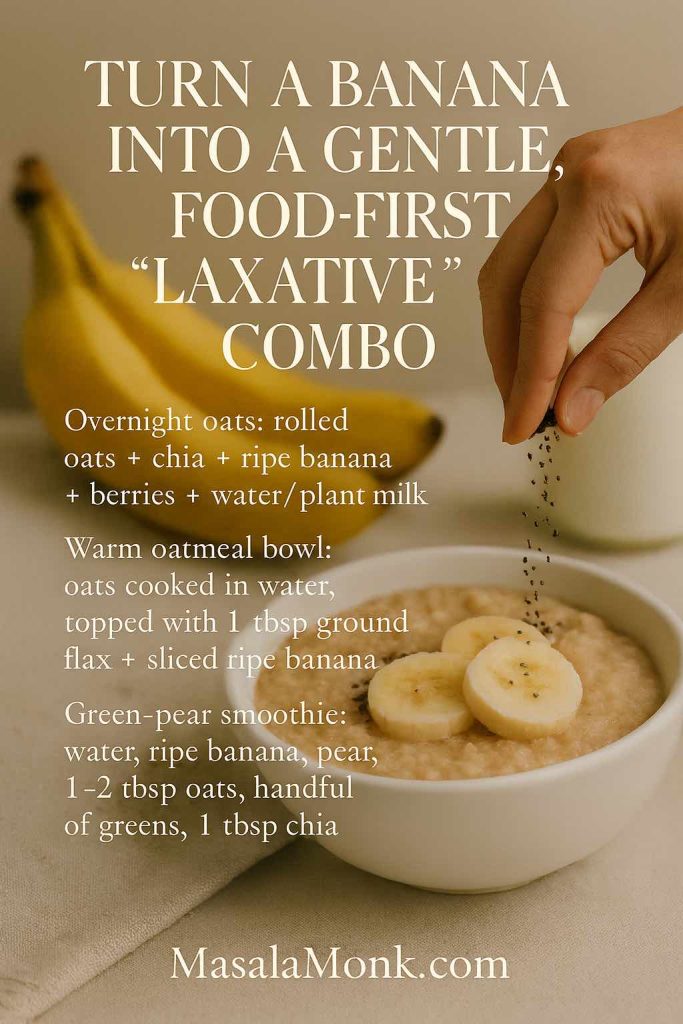
Chia or ground flax add-ins—a teaspoon whisked into spreads boosts softness without heaviness. Chia’s mucilage is well documented (chia fiber review), and flax blends easily into hummus or avocado (see flax seeds for strong digestion).
Hydration reminder—fluids help fiber function; thus, pair every High-Fiber Sandwich with water or herbal tea (NIDDK guidance).
Also Read: Psyllium Husk (Isabgol/Ispaghula) Side Effects: Risks, Benefits & How to Take It Safely
A day that shows how High-Fiber Sandwiches fit together
Breakfast
Oat-bran toast with avocado + ground flax; sliced kiwi on the side. (Fluids help fiber work—keep a glass of water nearby: NIDDK guidance.)
Lunch
Hummus–Kiwi–Greens “Softener.”
Snack
Whole-grain pita with hummus and grated carrot; sip water.
Dinner
Black Bean–Avocado Salsa Melt.
After meals
A 10–15-minute walk—especially helpful after dinner.
Weekly rotation
- Power relief days: Lentil Toastie (#2) + Hummus–Kiwi (#1).
- Steady maintenance days: Barley–Chickpea (#3) + Pear–Walnut (#4).
- Microbiome-minded days: Tempeh–Kimchi (#6) with a side of berries.
Because the builds repeat cleanly, you’ll hit helpful fiber totals consistently without chasing supplements.
Also Read: Hummus Veggie Sandwich: A Nutritious and Delicious Delight
Shopping once, eating well all week (repeatable High-Fiber Sandwiches)
These staples keep a high fiber plant-based diet effortless across the week.
Breads & grains
- 100% whole-grain or sprouted sandwich bread (≥3–4 g fiber/slice)
- Rye; oat-bran loaves
- Barley (pearled or hulled)
Legumes & spreads
- Hummus; canned or cooked chickpeas, lentils, black beans; white beans for mash
Seeds & flavor
- Chia; ground flaxseed; tahini; plain yogurt (dairy or plant-based)
- Lemons, dill, cumin, smoked paprika, black pepper, olive oil, vinegar
Produce
- Kiwifruit, pears, apples, oranges, berries, prunes
- Spinach/greens, carrots, broccoli slaw, cucumbers, tomatoes, onions
- Kimchi or sauerkraut
Batch tips
- Cook barley on Sunday; chill and portion for quick fold-ins.
- Freeze cooked beans flat in bags; they thaw in minutes.
- Keep a tiny “fiber station” (chia, ground flax) in reach so you never forget the add-ins.
- Pre-shred carrots and wash greens to make assembly truly five minutes.
Also Read: The Best Greens for Gut Health and Digestive Wellness
Gentle ramp-up (comfort matters with High-Fiber Sandwiches)
If you’re coming from a low-fiber baseline, jumping to 30+ grams immediately can feel rough. Therefore, increase gradually—about 5 g per day each week—and keep fluids steady. On a day that feels gassy, reduce raw brassicas, emphasize oats, barley, chia/flax, and use ripe pears or kiwi for a softer profile; subsequently, bring the extra crunch back as comfort improves. For a neutral reference on intake ranges, most adults do well around 25–38 g/day (scale up gradually: concise intake overview).
Also Read: Top 10 Foods for Gut Health
Put it all together (and keep repeating)
Ultimately, relief comes from meals that are moist, fibrous, and easy to repeat. These six High-Fiber Sandwiches were engineered for exactly that: whole-grain bread for steady bulk, legume spreads for satisfying depth, chia or ground flax for gentle gel, and fruit-veg add-ins—kiwi, pear, apple, carrots, greens—for softness and volume. Add water, take a short walk, and give it a few consistent days. Consequently, your gut will notice; meanwhile, your schedule won’t suffer; and, importantly, your lunches will finally pull their weight.
For quick reference when you need an extra nudge, bookmark prune juice & prunes for constipation; for fermented add-ins that pair well with High-Fiber Sandwiches, explore probiotic-rich sandwiches.
FAQs
1) What makes these High-Fiber Sandwiches good for constipation relief?
Because they combine foods rich in soluble fiber (oats, barley, chia, ground flax) with insoluble sources (bran, leafy greens, vegetable skins), they add moisture and gentle bulk together. Consequently, stools hold water, bowel movements become easier, and overall digestive health feels steadier. Meanwhile, the format is practical—so you actually repeat it.
2) How many grams of fiber should I aim for with a high fiber plant based diet?
Most adults do well around 25–38 g per day. That said, increase gradually. For example, add about 5 g per day each week and space it across meals. In practice, two High-Fiber Sandwiches can provide a big share, while breakfast and snacks top up the rest.
3) Which ingredients are the best high fiber foods for constipation relief inside a sandwich?
Start with plant based foods high in fiber: chickpeas, lentils, and black beans. Then, add foods that are rich in soluble fiber—chia, ground flax, oats, and barley—for gel-forming softness. Finally, tuck in high fiber fruits and vegetables for constipation like kiwi, pear, apple (skin on), carrots, and leafy greens for comfortable volume.
4) Are there specific fiber rich fruits for constipation that work especially well between bread?
Yes—pears and apples (with the skin), berries, and kiwi slot neatly into layers. Moreover, citrus segments and grated carrot add juiciness without heaviness. In turn, those choices support bowel movements while keeping sandwiches fresh and bright.
5) What bread should I pick for high fiber foods for gut health?
Choose 100% whole-grain or sprouted loaves that list whole grain first and give at least 3–4 g fiber per slice. Better yet, rotate rye, oat-bran, and barley-forward breads to keep textures interesting and to boost foods rich in soluble fiber via β-glucans.
6) I feel gassy when I jump into a plant based high fiber diet. What should I tweak?
First, slow the ramp—add fiber gradually. Next, emphasize moist builds with foods that are rich in soluble fiber (chia, ground flax, oats, barley) and slightly reduce raw brassicas for a few days. Subsequently, bring crunch back as comfort improves. Hydration and a brief walk after meals often help.
7) How can I hydrate wisely so high fiber foods to ease constipation actually work?
Pair each sandwich with a full glass of water. Additionally, use juicy layers—tomato, cucumber, citrus segments—to keep bites moist. Consequently, soluble fibers can form the soft gel that supports smoother bowel movements.
8) What are smart add-ins for high fiber foods for colon health?
Sprinkle 1 teaspoon of chia or finely ground flax into spreads; fold beans into hummus; or add a spoon of barley or oat-bran to legume salads. Therefore, you raise soluble fiber without making the sandwich bulky or dry.
9) Can I keep these High-Fiber Sandwiches fully vegan?
Absolutely. In fact, a high fiber plant based diet is the default here. Use hummus, white-bean mash, avocado-chia spreads, and yogurt-style dairy-free sauces. Meanwhile, tempeh, kimchi, and sauerkraut bring plant-forward protein and tang that support gut health.
10) What are easy meal-prep moves so my high fiber foods for digestive health stick all week?
Batch-cook lentils and chickpeas; chill barley; pre-grate carrots; wash greens; and keep ground flax and chia within arm’s reach. Consequently, assembly takes five minutes, and you’ll actually repeat the habit.
11) How do I balance high fiber foods for bowel movements with a sensitive stomach?
Begin with softer, moist builds: creamy spreads, thin-sliced fruit, and tender greens. Moreover, keep portions moderate, chew thoroughly, and add a short post-meal walk. On balance, that trio supports comfort while still moving fiber intake upward.
12) Are raw veggies mandatory, or can I still get high fiber foods for constipation relief with gentler textures?
You can. Lightly sautéed onions/peppers, roasted carrots, or softened greens still count. In practice, you’ll retain fiber while improving tolerance. Therefore, choose textures your gut likes and keep moisture high.
13) Which spreads quietly raise foods rich in soluble fiber without changing flavor?
Hummus mixed with 1 tsp ground flax, avocado blended with 1 tsp chia, or yogurt-tahini whisked with oat-bran. Subsequently, you’ll notice creamier bites and better stool softness—without extra weight.
14) Do I need fruit at every meal to hit high fiber foods for gut health targets?
Not necessarily, but it helps. For instance, one high fiber fruits for constipation choice (pear, apple, berries, or kiwi) inside or beside a sandwich boosts totals and adds moisture. Meanwhile, legumes and whole-grain bread carry the rest.
15) What’s the simplest “starter” High-Fiber Sandwich if I’m brand-new to this?
Begin with whole-grain bread, hummus + 1 tsp ground flax, thin-sliced pear or apple, and a handful of spinach. Therefore, you’ll get foods rich in soluble fiber plus gentle bulk in a mild, friendly package.
16) How do I keep high fiber foods for colon health from feeling dry or dense?
Layer moisture at every step: creamy spread, juicy produce, and a quick acidity hit (lemon, vinegar, salsa). Consequently, the sandwich eats soft, not stodgy—and your bowel movements tend to follow suit.
17) Are there kid-friendly options that still count as plant based foods high in fiber?
Yes: mashed black beans with mild salsa and avocado on soft whole-grain bread; chickpea “salad” with finely diced cucumber; or thin pear slices with yogurt-tahini. Moreover, cutting sandwiches into small squares improves traction with picky eaters.
18) How can I vary flavors yet stay within high fiber foods for digestive health?
Rotate breads (rye, oat-bran, sprouted), spreads (hummus, white-bean, avocado-chia), and high fiber fruits and vegetables for constipation (pear, apple, kiwi, carrot, greens). In turn, you’ll keep taste buds happy while the fiber keeps working.
19) Do these ideas help if I’m focused on high fiber foods for gut health beyond constipation?
Generally, yes. While everyone’s different, a steady mix of soluble and insoluble fiber plus plant diversity often supports gut health and overall comfort. Nevertheless, adjust portions and textures to your tolerance.
20) What’s a quick checklist before I make any High-Fiber Sandwiches?
Whole-grain bread (3–4 g fiber/slice) ✅
Legume base (⅓–½ cup) ✅
Seed booster (1 tsp chia or ground flax) ✅
Juicy produce (heaped) ✅
Water alongside + brief walk ✅
Therefore, you’ve covered high fiber foods for constipation relief and set up a predictable, comfortable day.