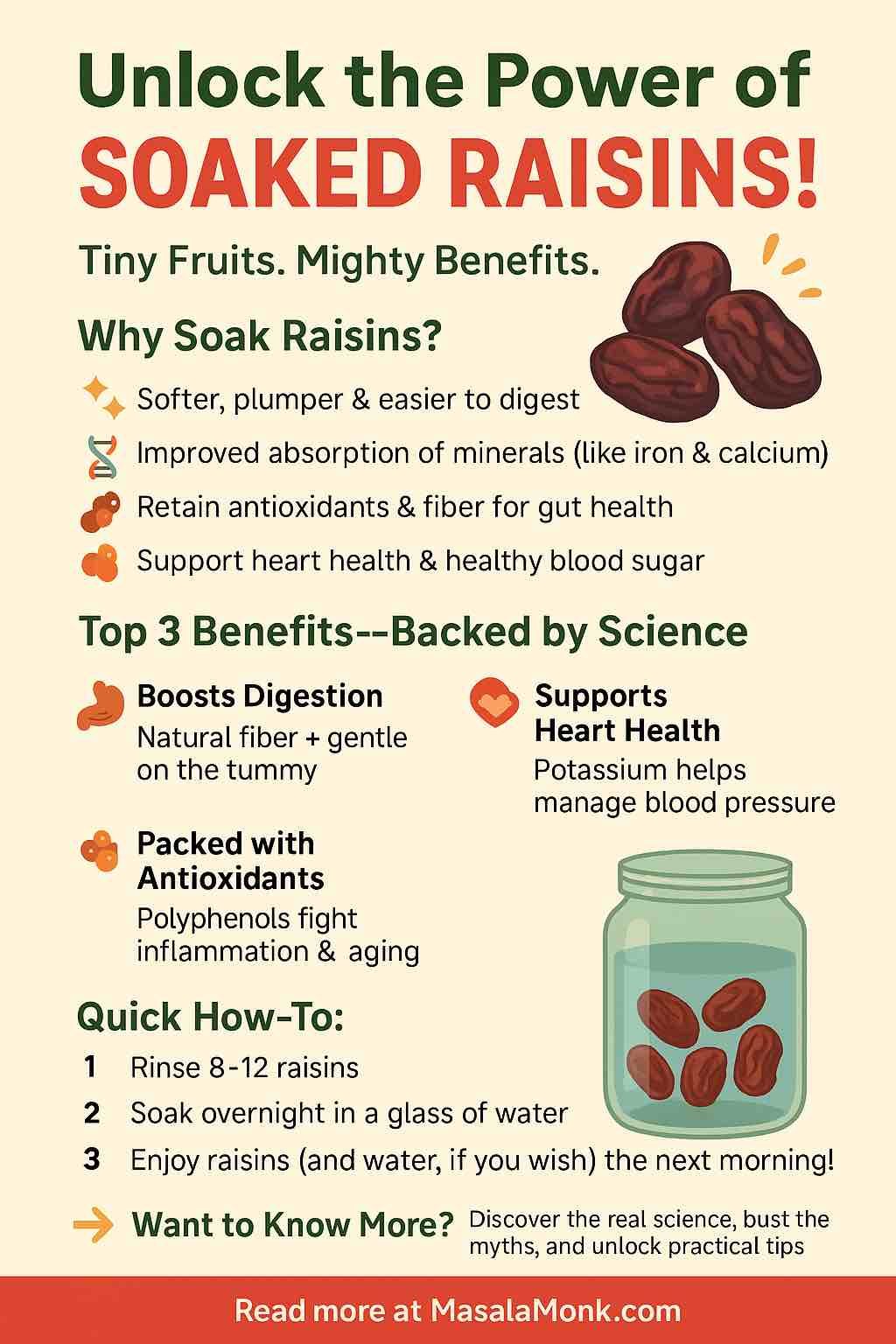
Imagine starting your day with a handful of sweet, plump raisins—transformed overnight by nothing more than a soak in water. While raisins are a staple in pantries across the globe, soaking them has become a popular morning ritual, especially in wellness circles and traditional Ayurveda. But what’s the real story? Are soaked raisins truly a nutritional powerhouse, or just another health trend? Let’s dive deep, separate myth from fact, and discover how you can unlock the full potential of this humble dried fruit.
Section 1: Why Soaked Raisins? A Historical and Scientific View
Raisins, or dried grapes, have a history as rich as their flavor. Used in ancient Persia, Greece, and India, they’ve long been celebrated for their concentrated energy and sweetness. But soaking them? That tradition stems from Ayurveda and folk wisdom, promising better digestion, “detoxification,” and even glowing skin.
But science has started to catch up, looking beyond old wives’ tales to understand what actually happens when you soak raisins overnight.
Section 2: The Science – What Really Changes When You Soak Raisins?
1. Softer, More Digestible
Soaked raisins are simply easier on the teeth and stomach. The soaking process rehydrates their tough skins, making them soft, plump, and easier to chew and digest. For anyone with sensitive teeth or digestive issues, this alone is a big win.
2. Reduced Anti-Nutrients, Enhanced Absorption
Like many plant foods, raisins contain “anti-nutrients” (phytates and tannins) that can bind to minerals like iron, zinc, and calcium, slightly reducing their absorption. Soaking, even for just 8-12 hours, can lower these compounds by 10–20%, theoretically making it easier for your body to access these minerals. While the effect is modest, it’s real—especially if your diet is mostly plant-based.
3. Nutrient Powerhouse Stays Intact
Importantly, soaking doesn’t “wash out” the good stuff! Raisins are naturally rich in:
- Potassium: Helps control blood pressure and heart function
- Iron: Vital for energy and fighting fatigue
- Antioxidants (polyphenols, resveratrol): Combat inflammation and oxidative stress
- Natural prebiotics: Promote gut health
- Fiber: Supports smooth digestion and healthy cholesterol
Section 3: Health Benefits—Backed by Research
A. Heart Health & Blood Pressure
Studies have shown that regular raisin consumption can lower blood pressure and LDL cholesterol, thanks largely to their potassium and fiber content. Some research even suggests a 6–10 mmHg drop in systolic BP when swapping raisins for processed snacks.
B. Blood Sugar Balance
Raisins, despite being sweet, have a moderate glycemic index. Multiple trials indicate that they cause a smaller spike in blood sugar than many refined carb snacks—good news for those with diabetes or prediabetes.
C. Gut Health & Regularity
The combo of soluble fiber and natural tartaric acid acts as a gentle laxative and prebiotic, feeding your good gut bacteria and supporting smooth, regular bowel movements.
D. Antioxidant & Anti-Inflammatory Power
Raisins retain powerful polyphenols after soaking. These compounds have been linked to reduced inflammation, healthier aging, and even improved brain function (in animal studies).
Section 4: Busted—Myths About Soaked Raisins
1. “Soaked raisins detox your body.”
There’s no scientific evidence that any food directly “detoxifies” your liver or cleanses your blood. The antioxidants and fiber in raisins can support your body’s natural detox pathways, but don’t expect miracle cures.
2. “Raisin water is a vitamin drink.”
Most vitamins and minerals remain in the fruit, not the soaking water. While raisin water can be a hydrating, slightly sweet beverage, it’s not a substitute for eating the whole raisin.
3. “You must eat them only in the morning.”
While morning routines can help you remember, there’s no magic time—soaked raisins are good any time of day!
Section 5: How To Soak & Enjoy Raisins—Your Daily Ritual
Step-by-Step Guide
- Measure out 8-12 raisins (about a tablespoon), preferably organic and unsweetened.
- Rinse them to remove any residue.
- Soak in a glass of clean, room-temperature water overnight (6–12 hours).
- In the morning, eat the raisins and, if you like, drink the water.
Pro Tip: Add a few strands of saffron or a pinch of cinnamon to your soak for an extra wellness boost and unique flavor!
Creative Ways To Use Soaked Raisins
- Add to breakfast oatmeal, porridge, or yogurt bowls
- Mix into salads for a sweet-tart pop
- Blend into smoothies for natural sweetness
- Top on toast with nut butter
- Incorporate into homemade trail mix or granola
Section 6: Practical Precautions
- Portion Control: Raisins are energy-dense. 8–12 per day is a good starting point.
- Sugar Content: Still high in natural sugars—suitable for most, but diabetics should monitor blood sugar.
- Dental Hygiene: Always rinse or brush after—raisins can stick to teeth.
- Allergies/Sensitivities: Rare, but possible—especially to sulfites if used as a preservative.
Section 7: The Bottom Line—Should You Soak Raisins?
Soaked raisins are a simple, practical way to make a healthy food even gentler and more enjoyable. The science supports modest improvements in mineral absorption and digestive comfort, but the real value comes from the core nutrients and antioxidants raisins already provide. If you love the taste and routine, there’s no downside—just pure, plant-based goodness in every bite.
Ready to Try?
Tomorrow morning, swap your usual snack for a handful of soaked raisins—and see how you feel! Sometimes, the simplest rituals offer the sweetest rewards.
FAQs About Soaked Raisins
1. What are the main benefits of eating soaked raisins?
Soaked raisins are softer, easier to digest, and may have slightly reduced anti-nutrients, making minerals like iron and calcium more available for absorption. They still provide antioxidants, fiber, potassium, and natural prebiotics—supporting heart, gut, and metabolic health.
2. How long should I soak raisins for best results?
Soak raisins for 8–12 hours (overnight is ideal) in clean, room-temperature water. This ensures they are fully rehydrated and easier to eat and digest.
3. Should I drink the water in which raisins were soaked?
Drinking raisin water is optional. Most nutrients and fiber stay in the fruit, but the water may contain some sugars and trace minerals. It’s safe and can be a hydrating, slightly sweet beverage, but eating the raisins is more beneficial.
4. Are soaked raisins better than unsoaked raisins?
Soaked raisins are easier on the teeth and stomach and may allow for slightly better mineral absorption. However, most of the core health benefits are present in both soaked and unsoaked raisins.
5. Can diabetics eat soaked raisins?
Raisins have a moderate glycemic index and contain natural sugars. In small amounts (8–12 per day), they can be part of a diabetic diet, but portion control and blood sugar monitoring are important. Consult your healthcare provider for personal guidance.
6. Can I soak other dried fruits with raisins?
Yes! You can soak raisins with other dried fruits like figs, apricots, or dates. Just be mindful that the combined sugar content will increase, so keep portions moderate.
7. Do soaked raisins help with constipation?
Yes, soaked raisins are a gentle, natural laxative due to their soluble fiber and tartaric acid content. Regular consumption may help improve bowel regularity.
8. Are there any side effects of eating soaked raisins?
Most people tolerate soaked raisins well. Overeating can cause digestive upset due to fiber and sugar. Rarely, some may be sensitive or allergic to grapes or preservatives like sulfites.
9. Do I need to rinse raisins before soaking?
Yes, it’s best to rinse raisins before soaking to remove any dust, residues, or preservatives on the surface.
10. Can kids and elderly people eat soaked raisins?
Absolutely! Soaked raisins are softer and less of a choking hazard, making them a safe, nutritious snack for children and older adults—provided there are no allergies or medical restrictions.