Summer in India (and much of the world) means intense heat, rising humidity, and a constant search for something cool, satisfying, and hydrating. Yet most commercial processed drinks—think sodas, bottled iced teas, energy drinks, and “fruit” beverages—are loaded with refined sugar, artificial flavors, and preservatives that often leave you feeling sluggish, not refreshed.
This year, we challenge you to #ReimagineRefreshment. Skip the processed, and turn to natural, wholesome, and on-trend alternatives—each carefully chosen for taste, nutrition, and practicality in your everyday routine. Let’s discover the top 5, why they work, how you can make them at home, and how each fits with a modern wellness lifestyle.
1. Cortisol Cocktail: Social Media’s Favorite Stress‑Busting Summer Sipper

What is it?
A “cortisol cocktail” is a hydrating, mineral-rich, non-alcoholic drink trending everywhere from TikTok to wellness podcasts. Despite the name, it contains no hormones—just a combination of natural ingredients that support hydration, electrolytes, and calm.
Key Ingredients:
- Coconut water (natural electrolytes & potassium)
- Citrus juice (vitamin C boost)
- Magnesium powder (supports calm, sleep, and nerve function)
- Sea salt (mineral replenishment)
- Sparkling water (just for fizz!)
How to Make It (1 glass):
- Pour 200ml coconut water into a tall glass.
- Squeeze in the juice of half an orange or lime.
- Stir in 1/4 tsp magnesium powder (or as per supplement label).
- Add a small pinch of sea salt.
- Top with sparkling water and a few ice cubes. Garnish with mint or orange wedge.
Why you’ll love it:
It’s lightly sweet, super hydrating, has no added sugar, and the minerals help with both energy and relaxation—a perfect afternoon pick-me-up or post-workout cooler.
Pro Tip: If you take medication or have kidney issues, check with your doctor before using magnesium supplements.
2. Prebiotic Soda: Gut-Friendly, Fizzy, and Fun

What’s new in 2025?
Big beverage brands and indie startups are rolling out “prebiotic sodas”—fiber-infused, naturally sweetened fizzy drinks made for gut health and a lighter summer vibe.
What makes it different?
- Contains plant-based prebiotic fiber (like inulin) for digestion.
- Lower in sugar than regular sodas.
- Naturally flavored with real fruit.
- Some use stevia or monk fruit for sweetness.
How to Make Your Own:
- Add a few fresh orange and strawberry slices to a glass.
- Pour chilled sparkling water over.
- Stir in 1 tsp inulin powder (available online/health stores).
- Add a tiny pinch of sea salt and a dash of stevia or honey if desired.
Why it’s great:
You get the satisfaction of bubbles without the sugar crash. Prebiotics feed the good bacteria in your gut, supporting overall digestion and wellness.
Pro Tip: Start with a small amount of inulin to let your system adjust.
3. Matcha Cooler: Energize with Antioxidants

Why matcha?
Matcha is a finely ground green tea powder rich in antioxidants, L-theanine (for calm focus), and a mild caffeine lift—ideal for summer afternoons or a healthy “mocktail hour.”
Trendy variations:
- Classic Iced Matcha: Whisk 1 tsp matcha powder with a splash of cold water until frothy. Pour over ice, top with more cold water, and add honey or maple syrup if needed.
- Pineapple Matcha Fizz: Whisk matcha, add pineapple juice, sparkling water, and ice for a tropical green twist.
- Matcha Lemonade: Mix matcha with lemon juice, a touch of agave, and plenty of ice.
Why you’ll love it:
Matcha is naturally energizing but gentle on the system—no jitters. It looks beautiful in the glass and tastes bright and grassy.
Pro Tip: Use ceremonial-grade matcha for best color and flavor.
4. Chaas / Buttermilk: India’s Traditional Summer Hero
Why is chaas a classic?
This yogurt-based drink, known as chaas, is the ultimate Indian cooler—full of probiotics, protein, minerals, and natural cooling properties. It’s the perfect digestif after a heavy meal or a sweltering day.
Simple recipe:
- Blend 1 cup plain dahi (curd/yogurt) with 1.5 cups cold water.
- Add 1/2 tsp roasted cumin powder, a pinch of black salt, and a handful of fresh mint or coriander.
- Pour over ice and serve immediately.
Why you’ll love it:
Chaas hydrates, replenishes lost electrolytes, and is ultra-satisfying after spicy food or long hours outside.
Pro Tip:
Add grated ginger, chopped cucumber, or even a dash of chaat masala for variety.
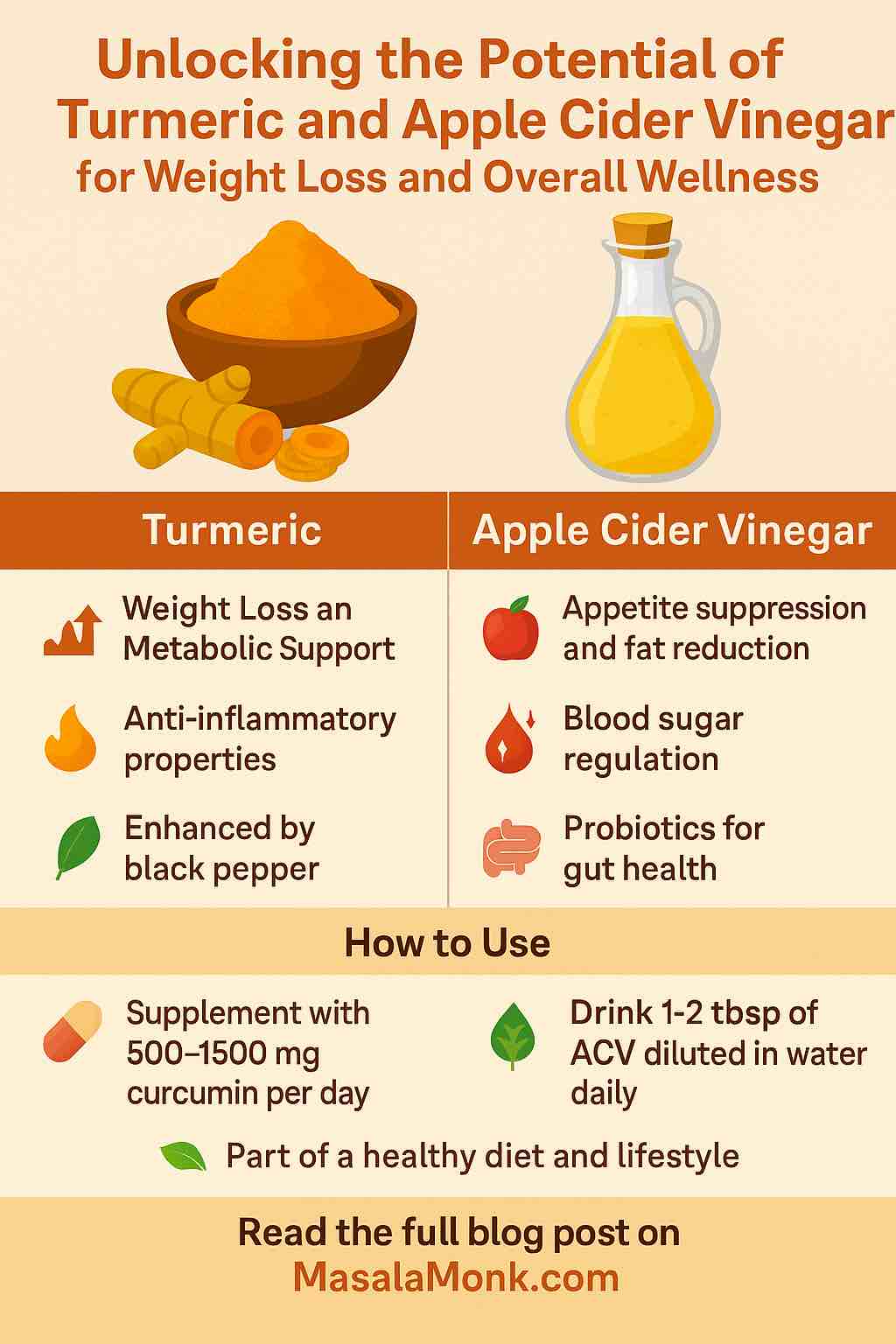
5. Turmeric & Ginger Tonic: Anti-Inflammatory and Zesty

Why this tonic?
Both turmeric and ginger are scientifically proven to fight inflammation, boost immunity, and aid digestion—plus, they make a beautifully golden, Instagram-ready drink.
How to Make:
- Boil a 2-inch piece of ginger in 2 cups water for 5 minutes.
- Stir in 1 tsp turmeric powder, juice of half a lemon, and 1 tbsp honey or jaggery.
- Add a pinch of black pepper (boosts turmeric’s benefits), strain, and chill.
- Serve over ice with lemon slices.
Why you’ll love it:
This drink delivers a vibrant flavor punch, supports your health, and looks gorgeous. Perfect as a midday refreshment or post-dinner “digestive.”
Pro Tip:
Make a batch ahead and store in the fridge—it’s even better cold!
Conclusion: Hydrate Smarter, Live Better
This summer, skip the commercial drinks aisle and embrace these natural, practical, and deeply satisfying alternatives. Whether you’re after hydration, gut health, energy, tradition, or an immune boost, there’s a perfect glass waiting for you.
Try them at home, share with family and friends, and tag your creations with #MasalaMonkDrinks for a chance to get featured!
Share Your Favorite
Which drink will you try first? Have your own healthy summer sipper?
Drop your recipes, questions, and reviews in the comments below.
Stay cool, stay hydrated, and enjoy every sip—naturally.
MasalaMonk.com
10 FAQs for Natural Summer Drinks
1. Are these drinks suitable for kids and seniors?
Yes, all drinks can be enjoyed by kids and seniors, but adjust the amount of added salt, spices, or supplements (like magnesium) for age and dietary needs. Always consult a doctor for any chronic health issues.
2. Can I prepare these drinks ahead of time?
Absolutely! Drinks like chaas, turmeric & ginger tonic, and infused prebiotic soda can be refrigerated for up to 24–48 hours. Just stir before serving and add fresh herbs/ice at the end.
3. Are these drinks vegan?
Most are vegan by default. For chaas, use plant-based yogurt. For sweeteners, replace honey with agave or maple syrup.
4. Do I need special equipment to make these drinks?
No special equipment needed! A blender or whisk is helpful for chaas and matcha, but all drinks can be made with basic kitchen tools like a pitcher, knife, and glass.
5. Where can I find inulin powder or magnesium powder?
These are available at health food stores, large supermarkets, or online. Choose a reputable brand and start with small quantities.
6. Can I use bottled coconut water or does it have to be fresh?
Bottled coconut water is fine—just choose unsweetened and no-added-flavor versions for the healthiest option.
7. How much sugar do these drinks contain?
Most drinks are naturally low in sugar. You control sweetness—add fruits, stevia, or minimal natural sweeteners if desired.
8. Are these drinks safe for people with diabetes?
Most are safe in moderation, but always check with your doctor. Use unsweetened versions and low-GI sweeteners if needed.
9. Can I make a big batch for a party or picnic?
Definitely! All recipes can be multiplied, made in pitchers, and served chilled. Add ice and herbs just before serving for freshness.
10. How do I store leftovers?
Store in a covered container or bottle in the fridge for 24–48 hours. Shake or stir well before pouring.