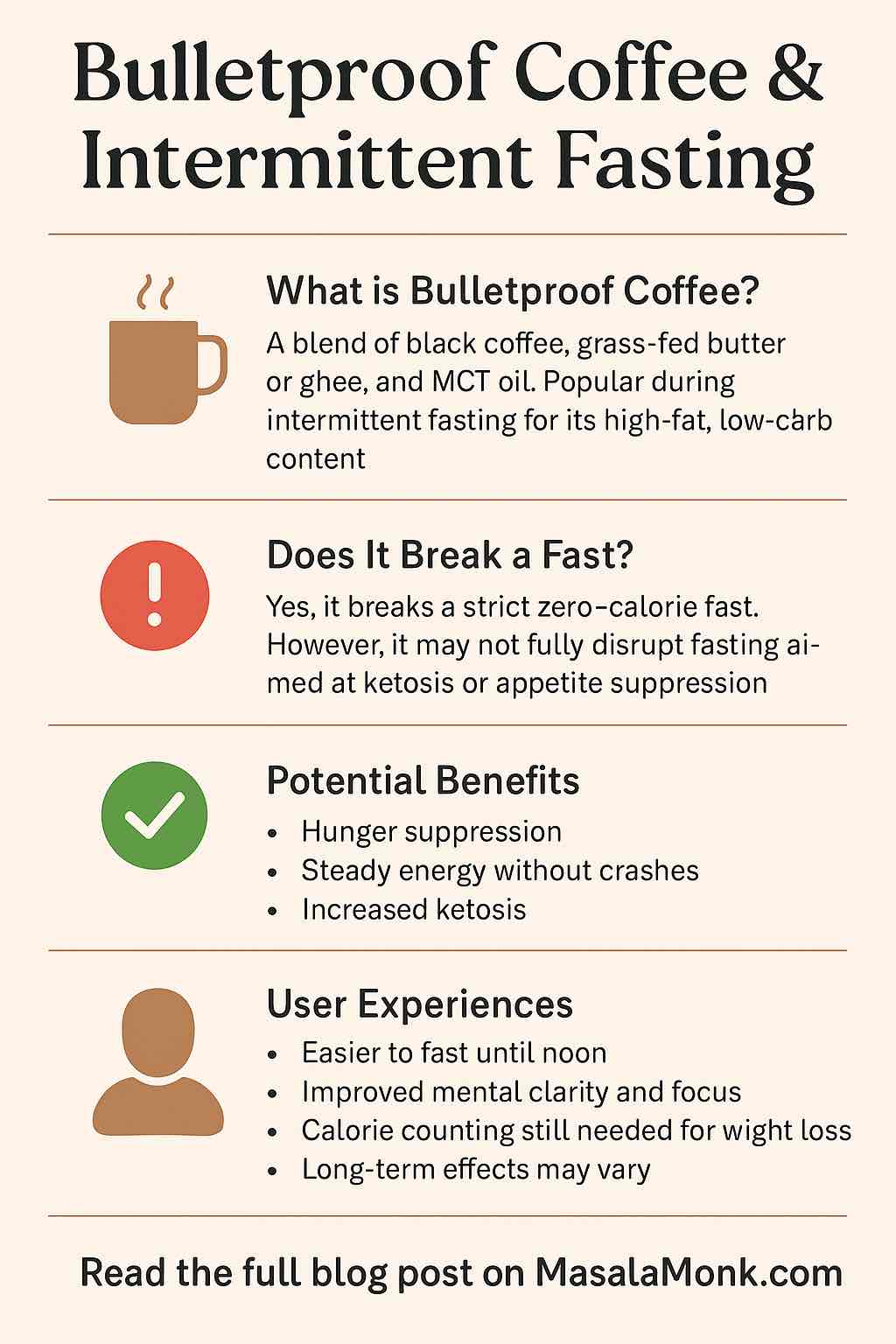
If you hang out in wellness forums, listen to biohacker podcasts, or simply love exploring new ways to optimize your mornings, you’ve probably heard of Bulletproof Coffee—that creamy, frothy blend of coffee, grass-fed butter, and MCT oil.
Pair that with intermittent fasting (IF)—the global health and weight-loss trend—and you get a routine that promises boundless energy, weight management, and laser-sharp focus. But does this combo actually deliver? Is it right for you? And what do real users say when the hype fades and habits settle in?
Let’s cut through the noise. Here’s your practical, up-to-date guide to Bulletproof Coffee and fasting, packed with research, honest feedback, and actionable tips.
What Exactly Is Bulletproof Coffee?
- Ingredients: Freshly brewed black coffee, grass-fed butter (or ghee), and MCT (medium-chain triglyceride) oil.
- How it’s made: Blend all ingredients for 15-30 seconds until frothy—like a rich, creamy latte.
- Why it’s popular: The fat slows caffeine absorption for “stable energy,” and MCTs convert rapidly to ketones, the brain’s preferred fuel during low-carb or fasted states.
Quick Recipe:
- 1 cup hot brewed coffee
- 1-2 tablespoons unsalted grass-fed butter/ghee
- 1 tablespoon MCT oil (start small if you’re new)
Blend & enjoy!
Intermittent Fasting Basics: Why Pair with Bulletproof Coffee?
Intermittent fasting is a way of scheduling your meals to create extended periods (often 12–20 hours) where you don’t eat, allowing insulin levels to drop and your body to switch to burning fat.
Popular patterns:
- 16:8 (fast 16 hours, eat within an 8-hour window)
- OMAD (one meal a day)
- Alternate-day or 5:2 fasting
Bulletproof Coffee’s appeal during fasting?
It can blunt morning hunger, supply “clean” energy, and—because it contains only fat—doesn’t spike insulin or blood sugar much, keeping you closer to a fasted state (even if it technically adds calories).
Does Bulletproof Coffee Break a Fast? (Practical Perspective)
Short answer:
- Yes, it breaks a strict zero-calorie fast (autophagy, full metabolic rest).
- No, if your goal is to maintain ketosis, control appetite, or make fasting tolerable (and you accept a few calories from pure fat).
Key Points:
- Calories: 150–350 per cup, all from fat.
- Insulin response: Minimal—no significant spike if pure fat is used (but individual variations exist).
- Autophagy: Likely reduced compared to water-only fasting.
- Appetite control: Most users report improved satiety and reduced hunger.
Real User Experiences: What Do People Actually Feel?
What’s Good:
- “I can fast until noon effortlessly, with zero cravings.”
- “Mental clarity is real—no jitters, no crash.”
- “Perfect for early meetings or a hectic commute. I don’t miss breakfast anymore.”
What’s Mixed or Cautionary:
- “It’s delicious, but if I’m not careful, I overeat at lunch.”
- “After six months, my cholesterol crept up—my doctor asked me to dial it back.”
- “Great for starting keto/IF, but eventually I just switched to black coffee.”
The Common Themes:
- Initial hunger suppression: Huge benefit, especially for fasting beginners or anyone making the keto switch.
- Sustained, steady energy: Less crash compared to sugary breakfasts.
- Mixed on weight loss: Some lose, some plateau—usually linked to total calorie intake.
- Taste is polarizing: You’ll love or hate the buttered texture—no in between.
- Long-term use: Watch your blood markers and overall calorie balance.
The Science: What’s Proven (and What Isn’t)?
- Satiety: Studies suggest MCT oil + caffeine can curb appetite, making fasting more tolerable.
- Metabolic effects: No big insulin rise from pure fats; can support ketosis. Not a magic bullet for metabolism.
- Weight loss: Driven mainly by reduced calories over time, not by adding fat to your coffee.
- Cholesterol: Saturated fats in butter/ghee can raise LDL in some people—monitor if you have heart risks.
References:
- Dr. Berg, 2025: Bulletproof Coffee and Fasting
- Healthline: 3 Reasons Why Bulletproof Coffee Is a Bad Idea
- MDPI review, 2023: Coffee, Fats, and Cognitive Benefits
Practical Tips: How to Use Bulletproof Coffee in Your Fasting Routine
1. Clarify Your Goal
- Zero-calorie fasting/autophagy: Stick to black coffee or plain tea.
- Appetite suppression or easier fasting: Try Bulletproof Coffee—but only if it truly helps you stick with your eating window.
2. Mind the Calories
- One cup is fine for most—don’t “stack” multiple servings.
- Track your intake if weight loss is your primary goal.
3. Choose Ingredients Wisely
- Grass-fed butter (more nutrients, better fats).
- Pure MCT oil—not coconut oil (MCTs are more ketogenic).
- High-quality, mold-free coffee beans.
4. Watch for Side Effects
- New to MCT oil? Start small—½ tsp and build up. Too much can cause stomach upset.
- Monitor cholesterol if you have risk factors.
5. Don’t Rely Solely on Bulletproof Coffee
- Use it as a tool, not a crutch.
- Still prioritize nutrient-dense meals with protein, fiber, and micronutrients.
Common Pitfalls & How to Avoid Them
| Pitfall | Solution |
|---|---|
| Overeating at lunch | Drink slowly; don’t use as an excuse for junk at meals |
| Cholesterol creeping up | Use less butter/ghee, more MCT, or alternate days |
| Digestive upset | Start with low MCT oil and increase slowly |
| Plateauing weight loss | Track total calories, skip BPC some days, switch to black coffee |
Sample Morning Fasting Routine (16:8 IF Example)
6:30 am – Wake up, hydrate (water, herbal tea)
7:30 am – Brew coffee, blend with 1 tbsp butter, 1 tbsp MCT oil
8:00 am – Sip slowly; check in with hunger
12:00 pm – Break fast with balanced, protein-rich meal
Throughout: Hydrate, listen to your body, adjust routine as needed
The Bottom Line: Should YOU Try Bulletproof Coffee with Fasting?
- If you’re struggling with morning hunger, need a “fasting hack” to get started, or love the taste—give it a try.
- If you have cholesterol issues or strict fasting goals, proceed with caution or stick to black coffee.
- For everyone: use it as a tool, not a magic bullet. Sustainable results come from balanced habits, not just a fancy coffee blend.
Pro tip: Periodically take breaks from Bulletproof Coffee to reassess your hunger, habits, and health markers.
Real-World Quotes
“I started BPC to help with fasting. Now, after a year, I just enjoy the taste. But I only have it on days when I really need the extra appetite suppression.” — Reddit user, 2025
“It’s not a diet miracle, but it made skipping breakfast less miserable. My weight loss? That came from what I ate after, not the coffee itself.” — Keto forum user
Further Reading & Resources
- Is Intermittent Fasting Good or Bad for You? (Time, 2025)
- Bulletproof Coffee Reviews & Recipes
- Latest on Bulletproof Coffee’s Health Effects (Cleveland Clinic)
Final Thoughts
Bulletproof Coffee can be a useful hack for making intermittent fasting easier and more enjoyable. But it’s not for everyone, and it’s not a shortcut to health. Use it thoughtfully, stay curious about how your body responds, and always keep the big picture—your overall nutrition and well-being—front and center.
Have you tried Bulletproof Coffee while fasting? Share your experience or questions below!
Frequently Asked Questions (FAQs)
1. Does Bulletproof Coffee break a fast?
Yes, it breaks a strict zero-calorie fast since it contains calories from fat. However, for those fasting to stay in ketosis or suppress appetite, it may not significantly disrupt your fasting goals.
2. Will Bulletproof Coffee kick me out of ketosis?
Unlikely, as it’s almost pure fat (butter/ghee and MCT oil) and contains virtually no carbs or protein, so it can actually help maintain or boost ketone production.
3. Can I lose weight if I drink Bulletproof Coffee during my fasting window?
Yes, but only if your total daily calories stay below your needs. Bulletproof Coffee is high in calories, so adjust your other meals to avoid overeating.
4. Is Bulletproof Coffee safe for people with high cholesterol?
It contains a lot of saturated fat, which may raise LDL cholesterol in some people. If you have cholesterol or heart health concerns, consult your doctor and monitor your blood work regularly.
5. Can I use coconut oil instead of MCT oil?
You can, but MCT oil is more efficiently converted into ketones, while coconut oil contains other fats that may not have the same effect.
6. What if Bulletproof Coffee upsets my stomach?
Start with a very small amount of MCT oil (½ teaspoon), increase slowly, and blend well. Too much MCT oil at once can cause digestive issues, especially if you’re new to it.
7. Can I add sweeteners, protein powder, or other ingredients?
Adding anything with carbs or protein (including sweeteners or protein powder) will increase insulin response and may break your fast more fully. For best fasting results, stick to the classic recipe.
8. Is Bulletproof Coffee a good meal replacement?
It suppresses hunger but lacks protein, fiber, and most vitamins/minerals. Use it occasionally, not as your sole breakfast or regular meal substitute.
9. How many times per day can I drink Bulletproof Coffee?
Most people do best with one cup per day during their fasting window. More than that can quickly add too many calories and saturated fat.
10. What’s the difference between Bulletproof Coffee and regular coffee with cream?
Bulletproof Coffee is made with grass-fed butter and MCT oil for higher fat, zero carbs, and a focus on ketosis, while regular coffee with cream typically contains less fat, more carbs, and lacks MCTs.