Do you ever feel a burning sensation in your chest after a meal, or wake up at night with acid in your throat? You’re not alone. Acid reflux and heartburn affect millions worldwide, but with a little know-how, you can take control—starting with what’s on your plate.
Why Does Acid Reflux Happen?
Acid reflux occurs when stomach acid flows backward into the esophagus, irritating its lining. The most common culprit? The lower esophageal sphincter (LES)—a muscular “gate” that should keep acid in the stomach, but sometimes relaxes or weakens. What you eat (and when you eat it) plays a major role.
The Usual Suspects: Foods That Commonly Trigger Reflux
Let’s get straight to it. The following foods and beverages have been consistently linked—by recent research and digestive health experts—to increased heartburn and reflux:
1. High-Fat & Fried Foods
- Examples: Fried chicken, pizza, creamy sauces, cheeseburgers, pastries, chips.
- Why They’re a Problem: High-fat meals slow down your stomach’s emptying and relax the LES, making it easier for acid to escape upward.
- Pro Tip: Choose baked or grilled options, and go easy on added oils and dressings.
2. Spicy Foods
- Examples: Hot sauce, chili peppers, curries, wasabi, salsas.
- Why They’re a Problem: Spicy ingredients—like capsaicin—can irritate the esophagus and further relax the LES.
- Pro Tip: If you crave heat, experiment with herbs or milder spices that don’t bother your stomach.
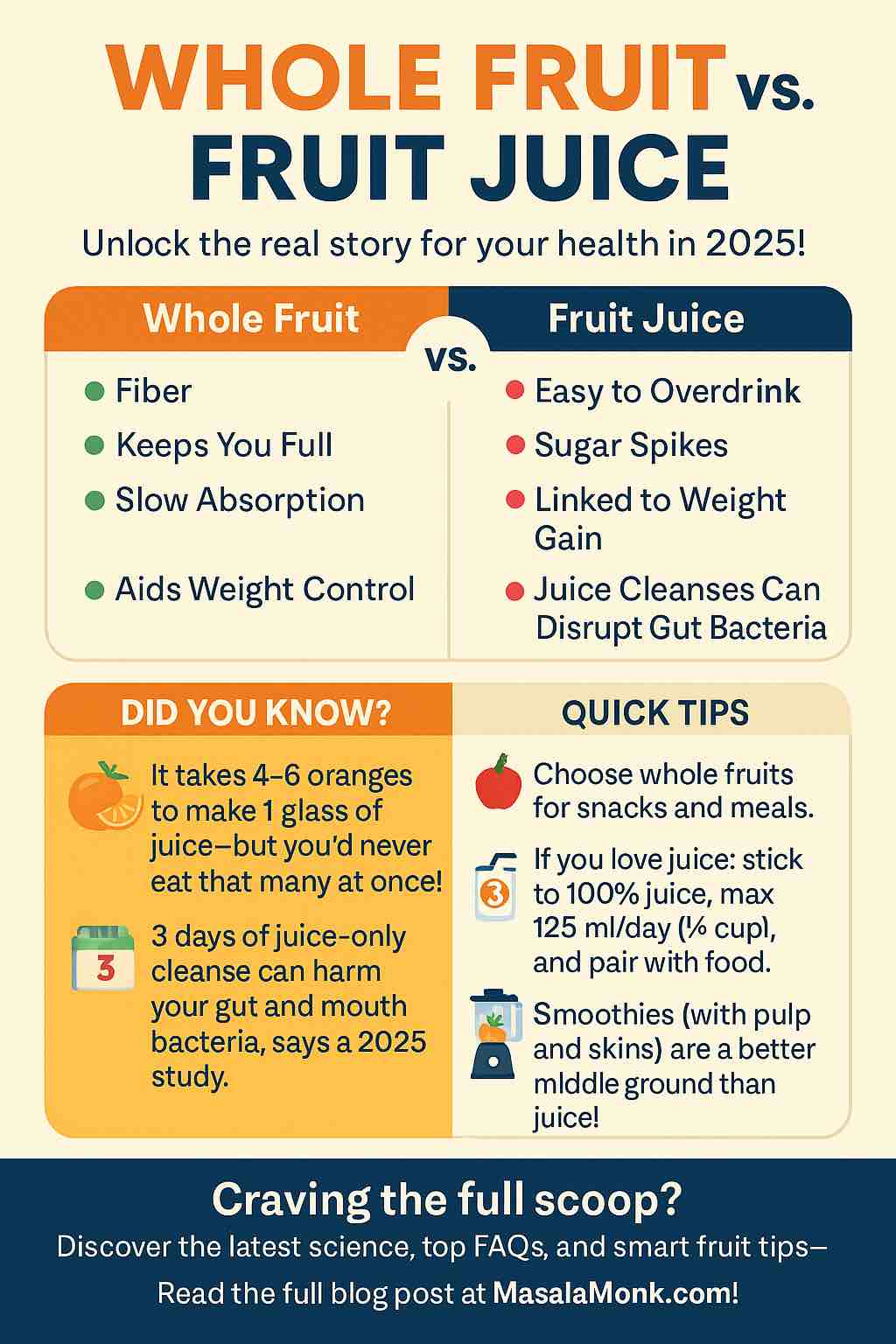
3. Citrus Fruits & Juices
- Examples: Oranges, lemons, limes, grapefruits, tomato-based sauces, orange juice.
- Why They’re a Problem: These are highly acidic, directly irritating your esophagus.
- Pro Tip: Opt for lower-acid fruits like bananas, apples (not green apples), and melons.
4. Chocolate
- Why It’s a Problem: Contains methylxanthine, which can relax the LES. Even small amounts may trigger reflux for some.
- Pro Tip: If chocolate is a must, choose a small portion after a meal, not on an empty stomach.
5. Caffeinated Drinks
- Examples: Coffee, some teas, energy drinks, cola.
- Why They’re a Problem: Caffeine can lower LES pressure and increase acid production. Even decaf coffee may be problematic for some.
- Pro Tip: Switch to non-caffeinated herbal teas (like ginger or chamomile) and limit coffee intake.
Do Read: Is Coffee Bad for Acid Reflux? Caffeine and Heartburn and for a take on Decaf, go here: Decaf Coffee and GERD: Is Decaf Coffee Better for Acid Reflux?
6. Alcohol
- Examples: Wine, beer, cocktails, spirits.
- Why It’s a Problem: Alcohol relaxes the LES and can directly irritate the digestive lining. Red wine and beer are common offenders.
- Pro Tip: Limit alcohol, enjoy with food (not on an empty stomach), or choose mocktails.
7. Carbonated Beverages
- Examples: Soda, sparkling water, beer, kombucha.
- Why They’re a Problem: Bubbles increase stomach pressure and cause burping, which can push acid upward.
- Pro Tip: Try flat water or lightly flavored, non-carbonated drinks.
In case you’re looking for some beverage options, please do read What to Drink for Acid Reflux and Heartburn Relief: Soothing Solutions That Work
8. Onion, Garlic, and Mint
- Why They’re a Problem: These can relax the LES (especially raw onion and garlic) and are high in FODMAPs—a class of carbs known to aggravate symptoms in some people.
- Pro Tip: Cook these ingredients thoroughly, use in moderation, or substitute with herbs like parsley or basil.
Also Read: Managing Acid Reflux: Foods to Avoid for a Soothing Digestive Experience
What Recent Research Says: Beyond the Obvious
Emerging research (2023–2025) points to some surprising truths and extra triggers:
• Ultra-Processed Foods
Hidden acids, fats, and preservatives in fast food, chips, commercial dressings, and processed snacks can worsen reflux—even if they’re not spicy or fried.
Tip: Read labels, cook more at home, and watch for “vinegar,” “citric acid,” and added fats.
• Large & Late Meals
Big portions stretch the stomach and increase acid production. Eating close to bedtime is linked to nighttime heartburn.
Tip: Eat smaller, more frequent meals. Aim for dinner at least 2–3 hours before lying down.
• Diet Patterns Matter
Low-fiber diets and those high in red/processed meats are associated with more reflux symptoms.
Tip: Favor Mediterranean-style eating—lots of veggies, whole grains, lean proteins, and healthy fats.
• Individual Triggers
What sets off reflux for one person may not bother another.
Tip: Keep a simple food and symptom diary for 2–3 weeks to spot your unique patterns.
So, What Can You Eat?
The good news: plenty! Most people tolerate these foods well:
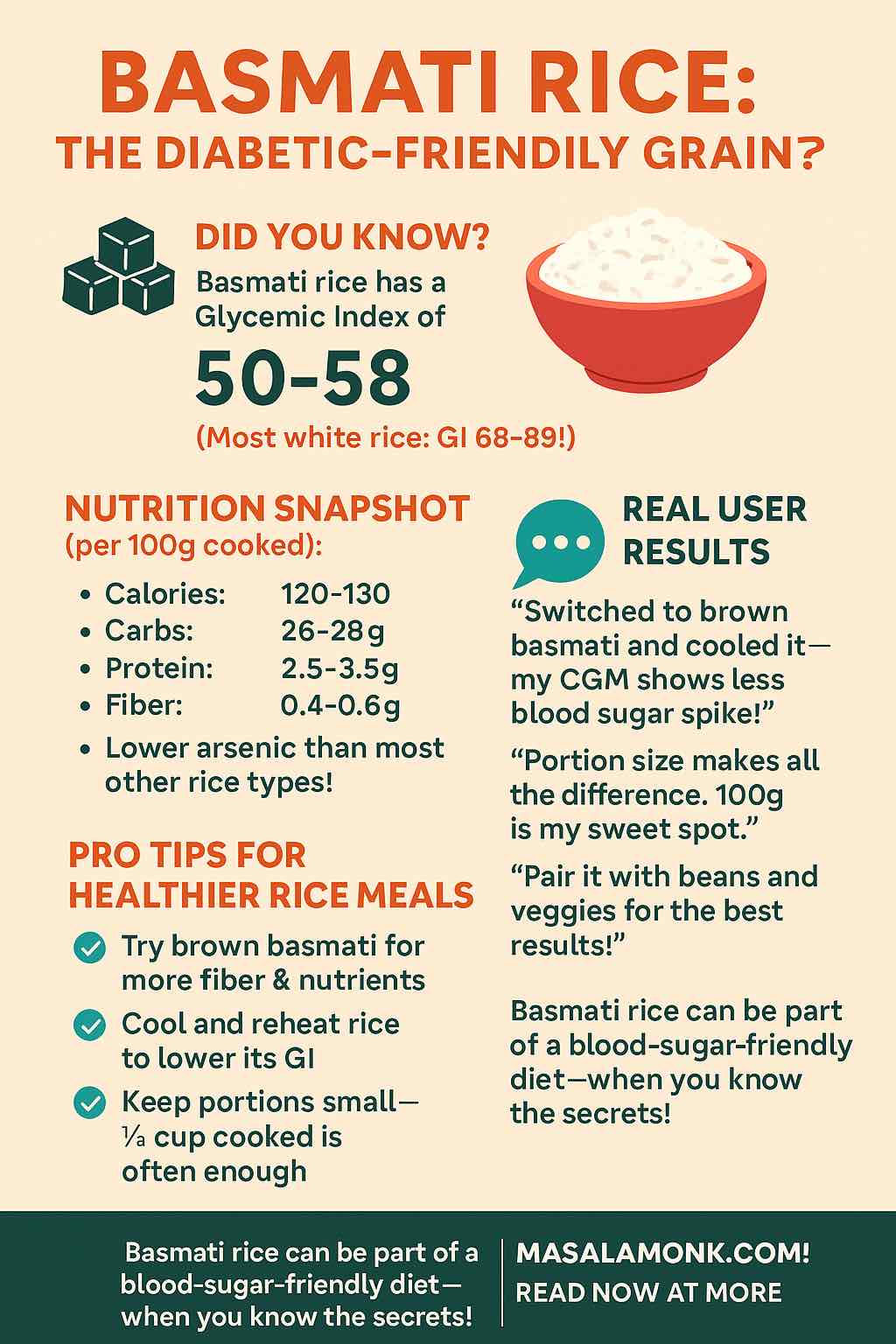
- Oatmeal, whole-grain bread, brown rice
- Bananas, melons, apples (peeled), pears
- Leafy greens, broccoli, asparagus, green beans, zucchini
- Skinless chicken, fish, lean turkey, eggs (not fried)
- Ginger (natural anti-inflammatory), fennel, parsley, basil
- Non-citrus herbal teas (chamomile, licorice root, ginger)
- Low-fat dairy (if tolerated; yogurt can be soothing)
Do Read: Ginger for Heartburn and Acid Reflux: Natural Relief or Digestive Myth?
Examples of Popular Foods & Their Relation to Acid Reflux
While the classic triggers like fried foods, caffeine, and citrus are well known, many people still have questions about everyday favorites that don’t always appear on “standard” reflux lists. Search data and patient experiences show that foods like mayonnaise, peanut butter, and popcorn often come up in conversations about heartburn and GERD. These items can be confusing because some people tolerate them well while others find they cause immediate discomfort.
To clear up the uncertainty, let’s take a closer look at how these specific foods may affect acid reflux, why reactions vary, and what practical swaps or adjustments can make them easier to enjoy.
Mayonnaise and Acid Reflux: Creamy Condiment or Hidden Trigger?
Many people wonder, “does mayonnaise cause acid reflux or heartburn?” The answer isn’t the same for everyone, but here’s what we know.
Mayonnaise is a high-fat condiment made primarily from oil, egg yolks, and often vinegar or lemon juice. The fat content is the biggest concern: fatty foods slow down digestion and relax the lower esophageal sphincter (LES) — the valve that keeps stomach acid where it belongs. When the LES relaxes, acid can escape upward, causing that familiar burning sensation.
Another factor is added acids like vinegar or lemon juice, which are common in mayo. These can further irritate an already sensitive esophagus. Store-bought mayonnaise may also contain preservatives and stabilizers, which can be problematic for some individuals with reflux.
That said, not everyone with GERD reacts to mayonnaise. Some people tolerate small amounts, especially reduced-fat or avocado-based mayonnaise, which contain less fat and may be easier on digestion.
Pro Tips:
- If you suspect mayo is a trigger, try switching to low-fat versions or alternatives like hummus or mashed avocado.
- Keep portion sizes small — a thin spread is less likely to cause trouble than a heaping spoonful.
- Combine mayo with reflux-friendly foods (like whole-grain bread and lean turkey) rather than fatty meats or fried items.
👉 Key takeaway: Mayonnaise can trigger reflux in some people because of its fat and acidity, but moderation and substitutions can make a big difference.
Peanut Butter and Acid Reflux: Comfort Food or Silent Aggravator?
Another common question is, “is peanut butter bad for acid reflux or GERD?” This one is a little more complicated.
Peanut butter is nutrient-dense, packed with protein, fiber, and healthy fats. On paper, it seems like a good choice. However, the same fat content that makes it filling and nutritious can also be a reflux trigger for certain individuals. High-fat foods take longer to leave the stomach and can relax the LES, creating the perfect storm for acid reflux.
Research and clinical observations suggest that while peanut butter is not universally problematic, about 10% of people with mild reflux and up to 50% of those with severe reflux report it as a trigger. For some, even a small spoonful can lead to chest burning or regurgitation.
The type of peanut butter matters too. Smooth, unsweetened peanut butter is typically better tolerated than chunky or flavored varieties, which may contain added oils, sugar, or salt that worsen reflux. Natural almond or cashew butters, which tend to be lower in additives, may also be gentler options.
Pro Tips:
- Stick to 1–2 tablespoons at a time, ideally paired with reflux-friendly foods (like apple slices or whole-grain toast).
- Avoid peanut butter late at night, since lying down soon after a high-fat snack increases reflux risk.
- If peanut butter consistently triggers you, try switching to almond butter, sunflower seed butter, or even a thin spread of hummus.
👉 Key takeaway: Peanut butter isn’t automatically “bad” for reflux. Many people tolerate it in moderation, but if you notice a connection, consider portion control or exploring alternatives.
Popcorn and Acid Reflux: Snack Attack or Safe Treat?
It’s a question many snack lovers ask: “can popcorn cause acid reflux or heartburn?” The answer depends on how it’s prepared.
Plain, air-popped popcorn is actually a low-fat, whole-grain snack that’s high in fiber and generally reflux-friendly. On its own, it’s unlikely to cause symptoms and can be a good option when you want something crunchy.
The problem comes when we dress it up. Movie-theater popcorn, microwave popcorn, and heavily buttered or seasoned popcorn can be loaded with fat, oils, salt, and artificial flavors — all of which can relax the LES and increase stomach pressure. For many people with GERD, this combination is enough to bring on a flare-up.
Another factor is portion size. Even plain popcorn, eaten in huge quantities, can stretch the stomach and trigger reflux. Moderation is key.
Pro Tips:
- Choose air-popped popcorn and enjoy it plain or lightly seasoned with reflux-friendly herbs (like parsley or basil).
- Skip heavy butter, cheese powders, or spicy toppings, which are common triggers.
- Limit serving size to 2–3 cups at a time to avoid stomach over-distension.
- Pair popcorn with a glass of still water or herbal tea rather than soda or alcohol.
To explore the topic further, we have more information available in this blog post here: Is Popcorn Safe for Acid Reflux, Heartburn, and GERD?
👉 Key takeaway: Popcorn itself is not inherently acidic or reflux-inducing. Air-popped, plain popcorn is usually safe, but buttery, greasy, or spicy varieties are more likely to cause problems.
| Trigger Food | Why It’s a Problem | GERD-Friendly Alternative |
|---|---|---|
| Fried chicken | High fat, slows digestion | Grilled chicken |
| Mayo | High fat + vinegar | Low-fat or avocado mayo |
| Buttered popcorn | Fat + oils | Air-popped, plain popcorn |
| Peanut butter (chunky, flavored) | Added oils, sugar | Smooth, natural peanut butter |
Real-Life, Practical Tips for Managing Acid Reflux
1. Personalize Your Plate
There’s no universal “no-no” list. Track what you eat and how you feel. Adjust as needed—don’t deprive yourself based on generic lists.
2. Eat Mindfully
Chew slowly, don’t rush meals, and avoid overeating. Sit upright for at least 30–60 minutes after eating.
3. Elevate Your Head
If nighttime reflux is a problem, raise the head of your bed by 6–8 inches, or use a wedge pillow.
4. Rethink Drinks
Limit carbonated and caffeinated beverages, and be careful with cocktails. Hydrate mostly with still water and herbal teas.
5. Move, Don’t Nap
Stay active after meals—light walking helps digestion. Wait at least 2–3 hours after eating before lying down.
6. Seek Professional Advice
Persistent, severe, or new symptoms? See a doctor or gastroenterologist. Dietitians can help create a plan tailored to you.
Do read What Foods Neutralize Stomach Acid Immediately?
Sample One-Day Acid Reflux-Friendly Meal Plan
| Meal | Menu Example |
|---|---|
| Breakfast | Oatmeal with banana and a splash of almond milk |
| Snack | Apple slices with a tablespoon of almond butter |
| Lunch | Grilled chicken with quinoa, roasted green beans |
| Snack | Non-citrus herbal tea, handful of unsalted almonds |
| Dinner | Baked salmon, steamed broccoli, brown rice |
| Evening | Melon cubes (if needed) |
The Takeaway: Find Your Balance
You don’t need to give up all your favorites forever. Small, sustainable changes—swapping out known triggers, eating smaller meals, and being mindful of timing—can make a big difference. Use the latest science as a guide, but trust your own experience above all.
Also Read: Baking Soda for Heartburn, Acid Reflux, & GERD
Your journey to a happier gut starts with what’s on your fork. Make it count—one meal at a time.
Got a question, a stubborn symptom, or a favorite reflux-friendly recipe? Share your thoughts below! Your story could help someone else find relief.
FAQs
1. What are the most common foods that cause acid reflux?
The most common triggers are high-fat and fried foods, spicy foods, chocolate, caffeine, alcohol, citrus fruits and juices, tomato-based products, carbonated beverages, and mint. These foods can relax the lower esophageal sphincter (LES) or increase stomach acidity, making reflux more likely.
2. Does mayonnaise cause acid reflux or heartburn?
Mayonnaise can trigger reflux in some people because of its high fat content and added acids like vinegar or lemon juice. These factors can relax the LES and irritate the esophagus. Low-fat or avocado-based mayonnaise may be easier to tolerate, but if you notice symptoms after eating mayo, it’s best to limit or substitute it.
3. Is peanut butter bad for GERD?
Not always. Peanut butter is high in healthy fats and protein, which makes it nutritious but also slower to digest. For some people, this can relax the LES and cause reflux. Smooth, unsweetened peanut butter is often tolerated better than chunky or flavored varieties. If peanut butter bothers you, try almond butter, sunflower seed butter, or smaller portions.
4. Can popcorn cause acid reflux?
Plain, air-popped popcorn is usually safe for people with reflux. The problem arises with buttered, oily, or heavily seasoned popcorn, which can increase symptoms. Portion size also matters—eating a very large bowl can stretch the stomach and trigger reflux. For a reflux-friendly option, choose air-popped popcorn with light, non-spicy seasoning.
5. Is coffee always a problem for people with heartburn?
Not always. Some people tolerate coffee (even regular) just fine, while others get symptoms from even decaf. If you notice heartburn after coffee, try limiting intake, switching to herbal teas, or drinking coffee with food instead of on an empty stomach.
6. Are there any “safe” fruits for people with acid reflux?
Yes. Bananas, melons, apples (peeled), and pears are generally well-tolerated by most people with reflux. Avoid citrus fruits like oranges, lemons, and grapefruits, as they are acidic and more likely to cause symptoms.
7. Can drinking milk help with heartburn?
It depends. Low-fat or nonfat milk may soothe symptoms for some, but full-fat dairy can worsen heartburn. Yogurt with live cultures may help, but tolerance varies. Test small amounts to see how your body reacts.
8. How can I prevent nighttime acid reflux?
Eat dinner at least 2–3 hours before lying down, elevate the head of your bed by 6–8 inches, avoid late-night snacks, and sleep on your left side if possible. These strategies reduce acid backing up into the esophagus during sleep.
9. Are spicy foods always off-limits?
Not necessarily. Some people handle moderate spice without symptoms. If you notice burning or discomfort after eating spicy foods, try milder options or reduce the amount until you find your personal threshold.
10. What should I eat when I have a heartburn flare-up?
Choose bland, low-acid, and non-fatty foods like oatmeal, bananas, toast, steamed vegetables, lean proteins (chicken, fish), and non-citrus herbal teas. Avoid known triggers until symptoms calm down.
11. Are there specific diets proven to help acid reflux?
Mediterranean-style and high-fiber diets have been shown to reduce reflux symptoms in research. Plant-based diets are also helpful for many people. Low-fat, low-acid, and whole-food approaches are best.
12. Do carbonated drinks always cause acid reflux?
Not always, but carbonated drinks (soda, sparkling water, beer) can increase stomach pressure and make symptoms worse for many people. Try non-carbonated beverages and see if your symptoms improve.
13. When should I see a doctor about my heartburn?
If you have heartburn more than twice a week, if symptoms persist despite dietary changes, or if you have trouble swallowing, unexplained weight loss, vomiting, or black stools, see a doctor. These may signal more serious conditions that need medical attention.