Living with arthritis means managing pain, stiffness, and inflammation on a daily basis—but did you know that what’s on your plate can make a real difference in your symptoms? Recent research, alongside thousands of personal stories from people living with arthritis, shows that certain foods can make things worse… while others can be a secret weapon for relief.
If you or someone you love has osteoarthritis, rheumatoid arthritis, or any other inflammatory joint condition, read on for the five worst foods to avoid, why they’re problematic, and what you can enjoy instead—all based on the latest science and what actually works in real life.
1. Ultra-Processed Foods: The Silent Saboteurs
What are they?
Think ready-to-eat snacks, packaged sweets, breakfast cereals, instant noodles, frozen meals, and almost anything that comes with a long ingredient list and a bright wrapper.
Why are they bad for arthritis?
Ultra-processed foods (UPFs) are loaded with unhealthy fats, sugars, refined carbs, preservatives, and additives. A major U.S. study published in 2025 found that for every 10% increase in calories from UPFs, arthritis risk jumped by 4–5%. These foods stoke inflammation, cause weight gain (which stresses your joints), and may even change how your muscles and bones function【pubmed.ncbi.nlm.nih.gov】【qps.com】【mdpi.com】.
User voices:
“Whenever I slip back into snacking on chips and cookies, my fingers swell up the next day.” — Reddit user, r/Thritis
What to eat instead:
Reach for real food! Try roasted chickpeas or nuts instead of chips, or homemade oat bars instead of packaged granola.
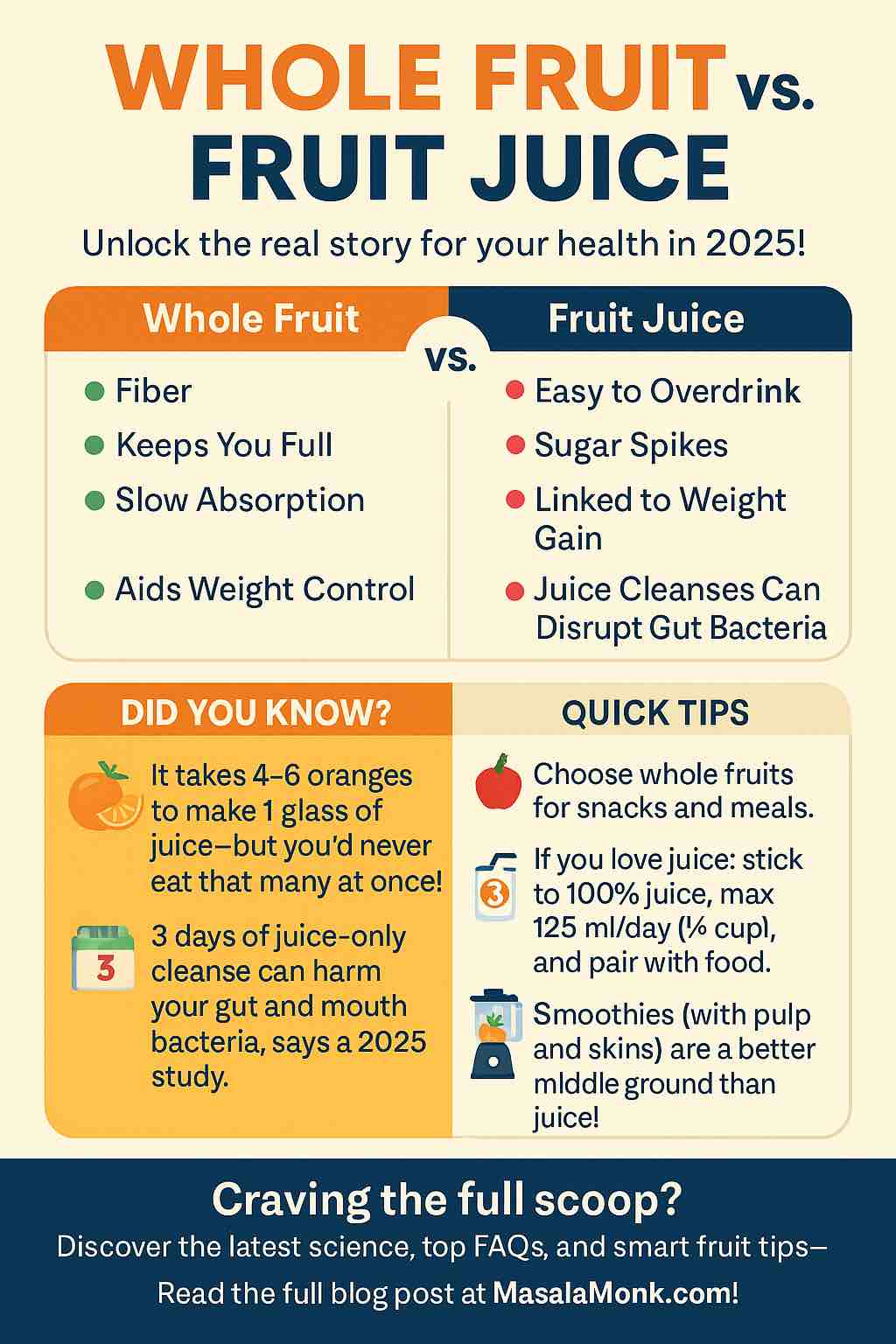
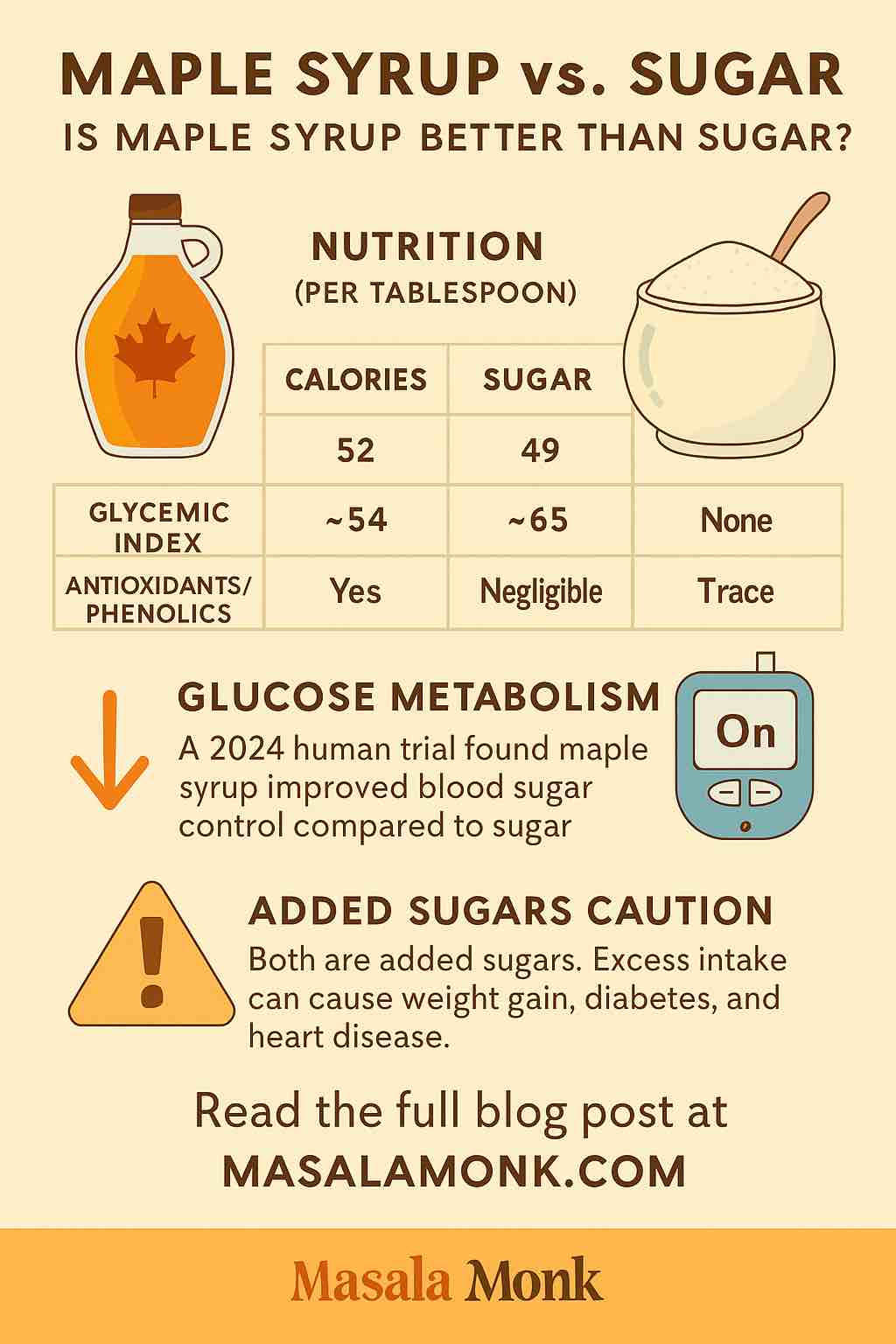
2. Sugar and Refined Carbs: Sneaky Inflammation Triggers
What are they?
Sugary drinks (soda, sweetened lassi, energy drinks), candies, pastries, white bread, and most desserts.
Why are they bad for arthritis?
Sugars and refined carbs spike blood sugar, raise levels of inflammatory chemicals in your body, and can worsen joint pain and swelling. They also drive weight gain and insulin resistance, which are linked to worse arthritis outcomes【eatingwell.com】【healthline.com】.
User voices:
“Sugar is the main trigger for my flares. Cutting it out made a huge difference.” — Reddit user, r/rheumatoid
What to eat instead:
Switch to whole grains (millet, brown rice, whole-wheat chapati), fresh fruit, or a small piece of dark chocolate when you crave something sweet.
3. Red and Processed Meats: Inflammation on a Plate
What are they?
Beef, pork, lamb, hot dogs, sausages, bacon, and most deli meats.
Why are they bad for arthritis?
Red and processed meats are high in saturated fats and advanced glycation end products (AGEs), which promote inflammation and may damage joint tissues. Several studies link frequent consumption to higher rates of RA and more severe osteoarthritis【nature.com】【eatingwell.com】.
User voices:
“My joints always feel worse after a weekend of barbecued meat and burgers.” — Community post, arthritis.org
What to eat instead:
Try plant-based proteins (beans, lentils, tofu), fish rich in omega-3s (salmon, sardines), or lean poultry.
4. Omega-6-Rich Seed Oils: The Imbalance Problem
What are they?
Corn, sunflower, soybean, and cottonseed oils (often used in processed foods and fried street food).
Why are they bad for arthritis?
These oils are not bad in moderation, but when consumed in large amounts—without enough omega-3s—they can tip the body toward inflammation. The latest research suggests keeping these oils in check and balancing them with sources of omega-3 fatty acids【eatingwell.com】【healthline.com】.
User voices:
“Cutting back on fried foods made with these oils calmed down my morning stiffness.” — Facebook arthritis support group
What to eat instead:
Use olive oil, mustard oil, or ghee (in moderation), and add flaxseed, chia seeds, and walnuts to boost your omega-3s.
5. High-Purine Foods (Certain Dals, Alcohol, Nightshades): The Surprising Triggers
What are they?
- Purine-rich lentils: Masoor dal (red lentils), some seafood, organ meats.
- Nightshades: Tomatoes, potatoes, eggplant, bell peppers (controversial; only an issue for some).
- Alcohol: Beer, spirits, and sometimes wine.
Why are they bad for arthritis?
High-purine foods can raise uric acid, triggering gout and worsening some forms of inflammatory arthritis. Nightshades contain compounds (like solanine) that may cause flares in sensitive people. Alcohol not only raises uric acid but also dehydrates and interacts with many arthritis meds【timesofindia.indiatimes.com】【health.com】【eatingwell.com】.
User voices:
“I didn’t believe nightshades mattered until I stopped tomatoes for two weeks—my hands were so much less swollen.” — Reddit user, r/autoimmunity
What to eat instead:
- Choose moong dal, masoor split dal, or urad dal over masoor whole dal.
- Experiment with removing and reintroducing nightshades to see if you react.
- If you drink, do so sparingly and always hydrate.
Why This All Matters: Food, Inflammation, and Your Daily Life
- UPFs and sugar can worsen joint pain even before you see weight gain.
- Balance is key: Some people tolerate nightshades or dairy just fine, while others do not.
- The gut-arthritis connection: Latest science confirms your gut bacteria and gut health play a role in arthritis. Highly processed foods and excess sugar damage beneficial bacteria, while fiber and fermented foods (like idli, dahi, chaas) help.
- It’s personal: Keep a food-symptom journal—what triggers you might not trigger your friend.
Practical, Real-World Swaps
| If You Eat This… | Try This Instead! |
|---|---|
| Packaged chips/snacks | Roasted chickpeas, nuts |
| Sweets, soda | Fresh fruit, jaggery-based treats |
| Fried foods in seed oil | Home-cooked with olive oil/ghee |
| Red/processed meat | Lentils, beans, tofu, fish |
| Masoor dal (whole) | Moong dal or split masoor |
| Lots of white bread | Brown rice, millet, oats |
How to Start: Small Steps That Work
- Begin by reading ingredient labels—look for added sugars, seed oils, and preservatives.
- Choose “real food” 80% of the time: If your grandmother would recognize it, you’re on the right track!
- Keep a simple journal: Write down what you eat and how your joints feel for a few weeks.
- Try one change at a time: Cut sugar for 2 weeks, or swap in moong dal for masoor. Notice what changes.
- Stay curious, not rigid: What works for you might surprise you!
The Power of Food: What’s Been Proven to Help
- Mediterranean-style diets (whole grains, fruits, veggies, olive oil, legumes, fish) cut RA risk by nearly 30%【nature.com】【eatingwell.com】.
- Bamboo rice (in new animal studies) reduces inflammation—future research may make this a new “superfood” for arthritis【timesofindia.indiatimes.com】.
- Time-restricted eating (10-hour daily window) may lower inflammation in animal models【frontiersin.org】.
- Fermented and fiber-rich foods support a healthy gut and reduce inflammation.
The Bottom Line
You don’t have to overhaul your entire diet overnight, but small, steady steps—like cutting back on UPFs, sugar, and red meat, and exploring more whole, plant-based foods—can make a noticeable difference. Backed by cutting-edge science and the wisdom of people living with arthritis, these changes are some of the most practical and powerful tools you have.
Arthritis may be a part of your life, but it doesn’t have to rule your plate!
Have a question or want a sample meal plan, India-friendly or Mediterranean-inspired? Share your story or request below—let’s build a community of healing, one meal at a time.
References (for more reading):
- The Mediterranean Diet May Help Lower Rheumatoid Arthritis Risk, New Study Says
- Why making a diet change may help your arthritis
- NIN study finds bamboo rice eases rheumatoid arthritis symptoms
- This one food habit could shield you from arthritis, obesity and diabetes
- The 8 Worst Foods to Eat for Inflammation
- User Experiences: Reddit r/Thritis
10 Most Frequently Asked Questions About Diet & Arthritis
1. Can changing my diet really help my arthritis symptoms?
Answer:
Yes, many people experience less joint pain, stiffness, and swelling after reducing ultra-processed foods, added sugars, and unhealthy fats. While food isn’t a cure, the right diet can be a powerful tool for managing symptoms and improving quality of life.
2. Which foods are most likely to cause arthritis flare-ups?
Answer:
Common triggers include ultra-processed snacks, sugary foods and drinks, red/processed meats, fried foods in omega-6-rich oils, and in some people, certain lentils (like masoor dal), nightshade vegetables, and alcohol.
3. Is there a specific diet that’s best for arthritis?
Answer:
The Mediterranean diet, rich in fruits, vegetables, whole grains, legumes, fish, olive oil, and nuts, has the strongest evidence for reducing inflammation and lowering arthritis risk. Plant-based diets and whole-food eating also show benefits.
4. Should I avoid all nightshade vegetables if I have arthritis?
Answer:
Not necessarily. Only a minority of people with arthritis react to nightshades (tomatoes, potatoes, eggplant, peppers). Try eliminating them for a few weeks—if you notice improvement, continue; if not, you can likely eat them without worry.
5. Is dairy bad for arthritis?
Answer:
It depends on the individual. Some people find dairy worsens their symptoms, while others tolerate it well. If you suspect dairy is an issue, try excluding it for a month and monitor your symptoms.
6. What about masoor dal and other lentils?
Answer:
Recent reports suggest masoor dal (red lentils) may aggravate joint pain in purine-sensitive people (e.g., gout or some RA). Moong dal, urad dal, and split masoor dal are generally better tolerated.
7. Can I still enjoy treats if I have arthritis?
Answer:
Absolutely! The key is moderation. Opt for occasional homemade treats with natural sweeteners, fruit, or dark chocolate, and focus on whole-food snacks most of the time.
8. What can I do if I’m unsure which foods are causing my symptoms?
Answer:
Try keeping a food and symptom journal for a few weeks. This helps identify patterns and potential triggers. Elimination diets—removing one suspect food group at a time—can also be very helpful.
9. How long will it take to notice improvement after changing my diet?
Answer:
Some people see changes in as little as 2–4 weeks, especially with sugar or processed food reduction. For others, it may take a few months of consistent changes to see real benefits.
10. Should I stop my medication if my diet helps my arthritis?
Answer:
No. Always talk to your doctor before making any changes to your medication. Diet can be an excellent support, but it is not a substitute for prescribed medical treatment.