Bloating after meals is common. The feeling is tight, pressurised, and distracting. Fortunately, relief rarely requires a complicated plan. Small shifts work first. Gentler foods, calmer drinks, and steadier habits often ease pressure quickly. In this guide, you’ll see what to eat when bloated with gas, which drinks soothe best in the morning, how to pick fibre that helps rather than hurts, and where food intolerances fit in. You’ll also learn how to use targeted helpers wisely, not endlessly.
If you notice red flags—weight loss, persistent vomiting, blood in stool, fever, or anaemia—please speak with a clinician. Otherwise, let’s get practical and calm things down.
Quick Relief Foods and Drinks: What to Eat When Bloated with Gas
To begin, keep your plate simple. Choose a low-fermentation base like plain rice or quinoa. Add eggs or firm tofu. Pair with soft greens such as spinach, zucchini, lettuce, or cucumber. This gentle trio digests more quietly.
Portion size still matters. Even friendly foods can stack up. The Monash FODMAP team explains how FODMAP stacking can tip a meal over your comfort line. They also show why serving size is crucial. During a flare, keep portions moderate. Afterwards, increase gradually.
Next, swap fizz for warmth. Ginger tea and peppermint tea are classics for good reason. Ginger shows human data for faster gastric emptying in functional dyspepsia, which many experience as less “stuck” heaviness. See the 2023 review. Peppermint, especially as enteric-coated oil, has clinical support for global IBS symptoms. The American College of Gastroenterology highlights peppermint in its guideline summary and full text: ACG overview and ACG PDF.
Also Read: What You Need to Know About Gut Inflammation and Digestive Health
Morning Drinks That Help: What to Eat When Bloated with Gas at Breakfast
Mornings set the tone. Start with warm water. It is basic yet gentle. Then pour ginger or mint. Ginger’s evidence on gastric emptying is mixed but encouraging. It remains a sensible first cup on unsettled mornings. Here’s the evidence overview.
Peppermint helps differently. It relaxes intestinal smooth muscle. Many notice less cramping and pressure. The ACG guideline supports peppermint for IBS-type symptoms. Here’s the link for ease: ACG guideline. If reflux bothers you, test timing and dose. Adjust as needed.
Prefer a culinary path? Our practical tour of the best tea for digestion covers fennel, cardamom, chamomile, and ginger blends. If mint is your favourite, see the guide on peppermint tea for IBS and bloating. It shows how to brew and use it consistently.
Low-FODMAP in Real Life: What to Eat When Bloated with Gas Without Staying Restrictive
A low-FODMAP approach often cuts gas and pressure. It helps many with IBS-type bloating. Still, the goal isn’t lifelong elimination. Instead, it’s to discover your personal tolerance and then re-expand variety. During flares, keep plates smaller. Avoid stacking several “green” foods in one sitting. The Monash explainers on stacking and serving size make this clear.
Which greens are easier? Spinach, lettuce, cucumber, and zucchini are common wins at moderate serves. Which tend to bloat? Broccoli heads, cabbage, and kale stems can be gassier for some. Cook well. Keep portions measured. Pair with rice or quinoa to dilute fermentable load.
On calmer days, keep variety exciting. Our list of foods that help you debloat covers snacks and produce that many find comfortable. You’ll see kiwi, banana, cucumber, fennel, ginger, and pumpkin. Use it for quick ideas when you’re busy.
Fibre, Re-thought: The Kind That Won’t Blow You Up
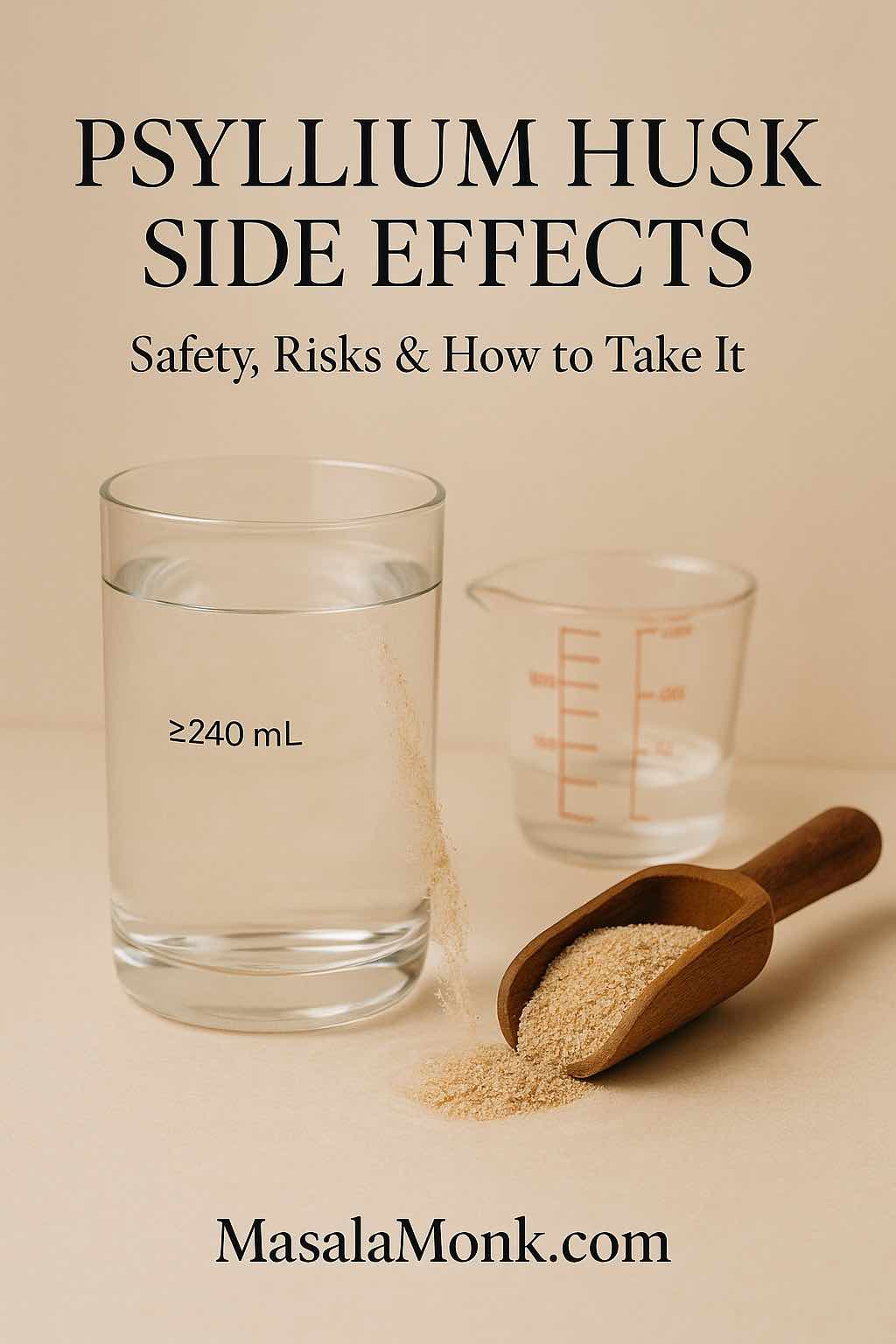
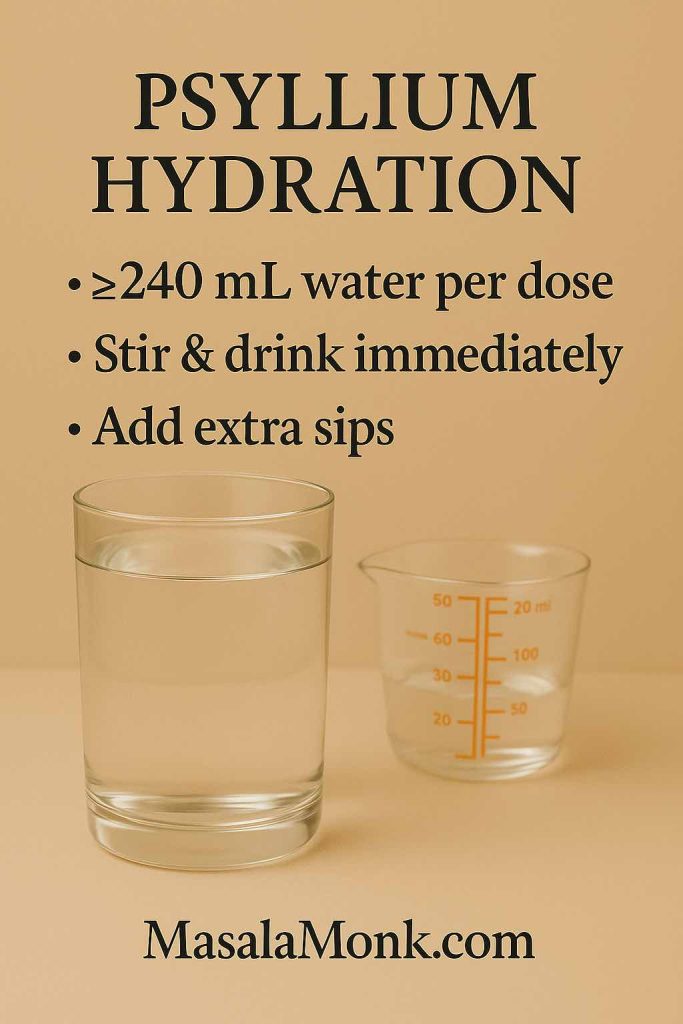
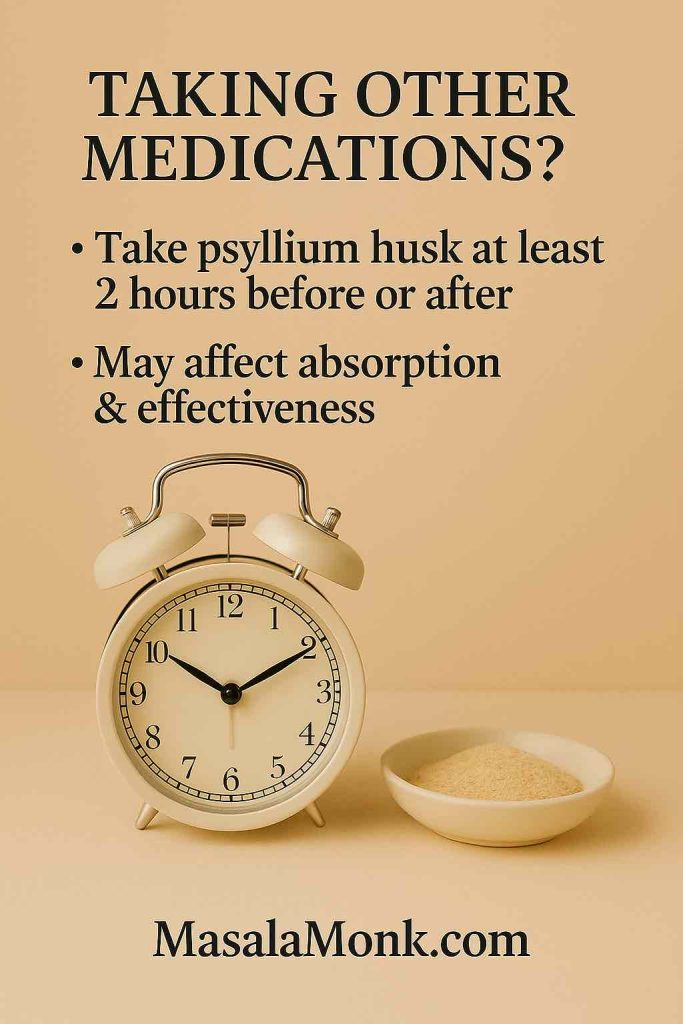
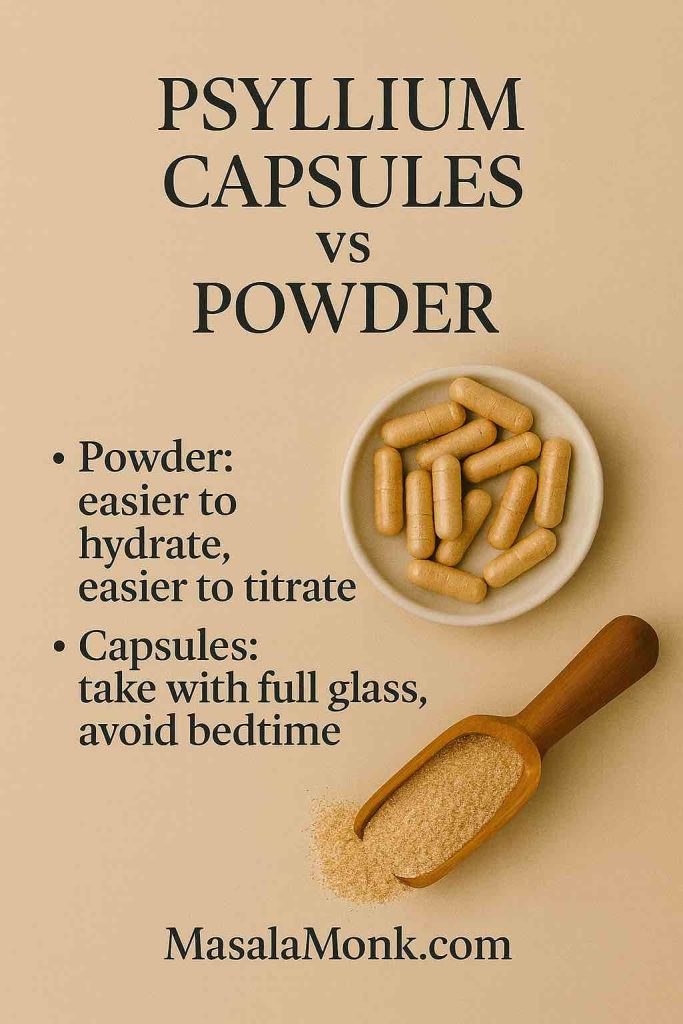
Fibre is essential for long-term gut health. Yet type matters. Soluble, viscous, relatively poorly fermentable fibres are friendlier during flares. Psyllium (ispaghula) is the classic choice. In contrast, highly fermentable prebiotic fibres—inulin and FOS—can raise gas when symptoms are active.
The ACG specifically recommends soluble fibre for global IBS symptoms. Here is the ACG overview. For a bite-sized recap, their slide deck is handy: ACG 2021 slides.
What does this look like at breakfast? Swap the raw, dense smoothie for oats or chia. If using psyllium, start low. Stir a small dose into water. Increase slowly. Hydrate well. Keep it steady
Also Read: 10 Creative Chia Pudding Recipes for Every Taste
Prebiotics vs Probiotics: When to Use Them If You’re Already Bloated
Prebiotics feed beneficial microbes. That’s good over time. However, they often increase gas at the start. If you’re mid-flare, wait. Introduce prebiotics later, in tiny steps. Build slowly once symptoms calm.
Probiotics are more variable. Some strains help IBS-type symptoms. Others do little. Benefits, when they appear, usually show within 4–8 weeks. Run a short trial. Track your response. Stop if you feel worse. For balanced expectations, the ACG guideline covers the evidence landscape: ACG 2021.
Also Read: Probiotics and Prebiotics: Digestive Duo for Constipation Relief
Beans, Crucifers, and Workarounds: What to Eat When Bloated with Gas After Dal or Broccoli
Legumes and crucifers are nutritious. They can also be windy. Preparation helps a lot. Soak and rinse legumes. Cook them thoroughly. Cook crucifers well. Keep portions moderate. Pair with rice or quinoa to dilute fermentables.
There’s also a targeted helper. α-galactosidase (e.g., Beano) can reduce gas formation from oligosaccharides. Timing is key. Take it with the first bites of the meal. Randomised crossover work showed fewer flatulence episodes after fermentable loads. Effects vary by person and dose, but many notice a clear difference. See the PubMed abstract and the J Fam Pract trial PDF.
Prefer tradition? Try saunf after meals. A pinch of fennel seeds is a classic. For a friendly explainer and a simple fennel tea, read Fennel Seeds for Digestion, Freshness, and Calm.
Dairy Dilemmas: Lactose, Lactase, and Friendlier Choices
If dairy makes you bloated, lactose is a likely reason. Many tolerate yogurt and hard cheeses better than milk. Fermentation helps. Lactose content is lower. Lactose-free options and lactase tablets widen choices when dining out.
For practical guidance, see the NHS pages. This NHS Inform overview explains symptoms and strategies: lactose intolerance. The NHS also outlines dairy and alternatives. A clinic leaflet gives concise tips on tolerated cheeses and yogurt: UHB NHS lactose intolerance PDF.
While you experiment, you might prefer a mint routine. A gentle tea after lunch. Capsules with dinner if appropriate. For a clear how-to, see peppermint tea for IBS and bloating. Keep it flexible. Match the plan to your day.
“Gluten Bloat,” or Wheat Fructans? Read This Before You Cut a Food Group
Outside coeliac disease, gluten often gets blamed for post-meal tightness. The real issue, for many, is fructans. Fructans are FODMAPs. They are concentrated in wheat and some related grains. In a controlled crossover trial, adults with self-reported gluten sensitivity reacted more to fructans than to gluten. Symptoms included bloating. Skim the research here: PubMed record and the ScienceDirect abstract.
What does that mean for everyday eating? Try a low-FODMAP grain strategy first. Properly fermented sourdough can also feel easier for some. This distinction preserves variety. It prevents unnecessary, long-term restriction.
Also Read: All About Gluten: Symptoms, Testing, Diet & 7-Day Gluten-Free Meal Plan
Cooking and Prep Methods That Calm a Bloated Belly
Technique matters. Gentle cooking often equals gentler digestion.
- Soak and rinse legumes. Then cook until soft. Undercooked legumes are harder work.
- Cook crucifers thoroughly. Steam or sauté until tender. Raw piles can be windy.
- Choose softer textures. Soups, khichdi, or congee feel easier in a flare.
- Season smartly. Fresh ginger, fennel, and mint are soothing. Heavy garlic and onion can be gassy for some.
- Cool and reheat rice or potatoes occasionally. A little resistant starch can help stool form. Still, watch your response.
Also Read: The Best Greens for Gut Health and Digestive Wellness
Hydration, Salt, and the “Puffy” Feeling
Bloating and water retention feel similar. They are not the same. Gas comes from fermentation and swallowed air. Puffiness comes from fluid shifts.
- Hydrate steadily. Sipping through the day helps motility.
- Watch salty take-away meals. Salt invites water retention. That swelling can mimic gas.
- Skip big gulps of fizzy water. Bubbles add volume. Save carbonation for calmer days.
- Limit sugar alcohols. Sorbitol, mannitol, and xylitol can be gassy. Check gum, “diet” ice creams, and protein bars.
Also Read: Healthy Oat Protein Bars – 5 Easy No Sugar Recipes for Snacks
Pace, Posture, and Breath: Small Habits With Big Payoffs
Food choices matter. So does pace.
- Eat slowly. Chew well. Fast meals push extra air into the gut.
- Sit tall while eating. Then take a relaxed 10–15-minute walk.
- Try a few calming breaths. Inhale through the nose. Exhale longer than you inhale. Gentle parasympathetic tone supports motility.
- Leave space before bed. Very late dinners can feel heavy.
- Schedule “calm” meals. A quiet, unhurried breakfast can change the whole day.
Consistency beats intensity. A small, steady plan prevents the next flare more than a strict week ever will.
Lunch and Dinner Templates: What to Eat When Bloated with Gas
Here are easy templates. Rotate them across the week.
Template 1: Rice bowl. Warm rice. Eggs or firm tofu. Spinach or zucchini. A spoon of yoghurt if tolerated. A squeeze of lemon if you like it. Sip ginger tea.
Template 2: Quinoa plate. Quinoa. Grilled fish or paneer if tolerated. Cucumber and lettuce. A drizzle of olive oil. Mint tea after.
Template 3: Khichdi comfort. Moong dal khichdi with ginger. A side of sautéed zucchini. A pinch of roasted cumin. Fennel tea later.
Template 4: Soup + toast. Blended carrot or pumpkin soup. Sourdough slice if you do well with it. A pat of butter if tolerated. Peppermint tea for dessert.
Template 5: Stir-fry light. Soft-cooked zucchini, bell pepper, and spinach. Tofu for protein. Rice on the side. Ginger-garlic if you tolerate it; otherwise ginger only.
Whenever beans or crucifers feature, consider α-galactosidase with the first bites. Evidence suggests fewer gas events after fermentable loads: PubMed and trial PDF.
Also Read: 6 benefits of adding Quinoa to your diet
Common Pitfalls That Keep You Bloated
People often do many things right. A few small missteps then undo the progress.
- Stacking “safe” foods. Three low-FODMAP items together can still be too much. Revisit FODMAP stacking.
- Portion creep. A “small” bowl becomes large by day four. Check serving size.
- Raw overload. Huge raw salads are tough during flares. Cooked textures digest easier.
- Chugging fizzy drinks. Carbonation plus speed equals discomfort.
- Too much inulin too soon. Prebiotics are useful later, not mid-flare.
- Skipping re-introduction. Elimination is a tool, not a home. Expand when your gut is calmer.
If you need inspiration that still feels indulgent, scan our page of foods that help you debloat. It keeps decisions easy.
Also Read: Food for Constipation Relief & Gut Health : 6 High-Fiber Sandwiches
Gentle Seven-Day Reset (Flexible, Not Rigid)
This is a pattern, not a strict plan. Adjust portions to your hunger and schedule.
Day 1–2. Keep meals small and steady. Rice or quinoa with eggs or tofu. Soft greens like zucchini or spinach. Ginger tea with breakfast. Peppermint tea later. A short walk after lunch.
Day 3–4. Add oats or chia at breakfast. Consider a small dose of psyllium if stools are hard. Hydrate well. Test a yoghurt portion if dairy is unclear. Use lactase with meals out if needed. See NHS guidance for practical swaps: lactose intolerance and dairy and alternatives.
Day 5–6. Re-introduce one higher-FODMAP item in a small amount. Note your response. If beans or crucifers are on the menu, consider α-galactosidase with the first bites. Evidence summary here: PubMed.
Day 7. Review. Which foods felt fine? Which portions were too large? Adjust the coming week. If “gluten” seemed troublesome, remember the fructans story. Many non-coeliac folks react more to fructans than gluten itself. The crossover trial is here: PubMed and ScienceDirect.
Also Read: Psyllium Husk (Isabgol/Ispaghula) Side Effects: Risks, Benefits & How to Take It Safely
Evidence-Based Helpers: How, When, and Why
A few add-ons deserve space in your cupboard.
Peppermint oil (enteric-coated). Use during IBS-type flares. It is supported by the ACG and meta-analyses for global symptom relief. Monitor reflux. Adjust timing as needed. Details here: ACG guideline.
α-galactosidase. Reserve for bean or crucifer-heavy meals. Take with the first bites. Expect fewer gas events, not perfection. Evidence: PubMed and trial PDF.
Simethicone. Safe and widely used. Evidence for chronic bloating alone is mixed. Some feel less pressure in specific contexts. Consider a short, personal trial. Keep it simple. The ACG touches on this in the broader therapy view: ACG page.
Also Read: Top 10 Foods for Gut Health (+ Pre/Probiotics, Best Drinks, Gut-Reset Plan)
Bringing It Together: What to Eat When Bloated with Gas Today, Tomorrow, and Next Week
Let’s pull the pieces into a plan you can repeat with confidence.
Today. Keep it calm. Plate rice or quinoa with eggs or firm tofu. Add a soft green like zucchini or spinach. Sip warm ginger or peppermint tea. If breakfast tends to slow you down, consider psyllium rather than a highly fermentable fibre. The ACG highlights soluble fibre as the smarter first move in IBS: ACG overview.
This week. Re-introduce foods methodically. Increase portions a little at a time. Note responses. If dairy brings pressure, try lactose-free milk. Test yogurt or hard cheese in small amounts. Use lactase when eating out. For practical tips, see NHS Inform on lactose intolerance and the NHS page on dairy and alternatives.
Dining out. Beans or crucifers on the menu? Consider α-galactosidase with the first bites. Evidence shows fewer gas events after fermentable loads. Read the details: PubMed abstract and trial PDF. If you think “gluten” is the trigger, remember the fructans story. Many non-coeliac folks react more to fructans than gluten itself. The crossover trial is here: PubMed and ScienceDirect.
Rituals. Routine helps more than perfection. Sip a calming blend in the evening. Rotate flavours so the habit sticks. For inspiration, see our best tea for digestion guide. And keep a short list of easy foods on hand. Our page on foods that help you debloat is a quick reference when you are tired or travelling.
Lastly, remember the heart of it. The phrase what to eat when bloated with gas is not a trick. It’s about balance, portions, warmth, and timing. It’s about fibre type and not just fibre grams. And then it’s about cooking methods, pace, posture, and steady routines. Most of all, it’s about testing small changes and keeping the ones that work.
FAQs
1. What to eat when bloated with gas right now?
Choose gentle, low-fermentation foods: plain rice or quinoa, eggs or firm tofu, and soft greens like spinach or zucchini. Moreover, keep portions modest and chew slowly so you reduce air intake and “stacking” effects.
2. What’s the best morning drink for bloating?
Start with warm water; then, consider a small cup of ginger or mint. Additionally, sip slowly rather than gulping—pace often matters as much as the drink itself.
3. Which greens help with bloating, and which can worsen it?
Typically, spinach, lettuce, cucumber, and zucchini feel easier in moderate portions. Conversely, broccoli heads, cabbage, and kale stems can be gassy for some, especially when under-cooked.
4. I’m low FODMAP but still bloated—why?
Portions can add up across a meal or a day, even with “safe” foods. Furthermore, carbonation, sugar alcohols, and eating too fast can trigger symptoms regardless of FODMAP load.
5. What to eat when bloated with gas after beans or crucifer vegetables?
Pair small portions with rice or quinoa; cook thoroughly; and, if needed, use an enzyme product with the first bites. Consequently, you’ll often notice fewer gas events and less pressure.
6. Do prebiotics help or hurt when I’m already bloated?
Prebiotics can support gut health long-term; however, they commonly increase gas early on. Therefore, delay them during flares or start with very small amounts and build slowly.
7. Which fiber doesn’t cause gas?
Psyllium (a soluble, viscous fiber) is usually the first choice during bloated phases. Likewise, oats and chia tend to feel friendlier than highly fermentable inulin or FOS.
8. Does Metamucil help with bloating?
It can, because it is psyllium-based; nonetheless, begin with a low dose and increase gradually. In addition, drink enough water to improve tolerance and stool form.
9. What drink is good to debloat fast?
Warm, non-fizzy options—such as ginger or mint infusions—are simple go-tos. Notably, avoid large carbonated servings during flares since bubbles add volume instantly.
10. What to drink in the morning for bloating and slow digestion?
Try warm water on waking, then a modest cup of ginger or mint with breakfast. Next, add a relaxed 10–15-minute walk to nudge motility without strain.
11. Does dairy make you bloated—and what can you do?
If lactose is the issue, many people tolerate yogurt and hard cheeses better than milk. Alternatively, choose lactose-free options or use lactase when dining out.
12. Is “gluten bloat” really about gluten?
Often it’s the wheat fructans (a FODMAP) causing trouble rather than gluten itself. Consequently, some feel better with low-FODMAP grains or properly fermented sourdough.
13. Do fermented foods cause gas?
They can, especially when added quickly or in large portions. Even so, many people do fine with small amounts once symptoms settle and portions are steady.
14. Are peppermint oil capsules useful for bloating?
They may help IBS-type discomfort and tightness for some adults. However, if you’re reflux-prone, adjust timing and dose, and monitor how you feel.
15. Are over-the-counter options like simethicone or digestive enzymes worth trying?
Sometimes, yes. Simethicone has mixed benefit for chronic bloat yet is safe for short trials, while alpha-galactosidase can reduce gas from beans and crucifers when taken with the first bites.
16. What to eat when bloated with gas after high-carb meals?
Choose simpler starches such as plain rice or potatoes; add eggs, tofu, or fish; and keep sauces light. Additionally, limit sugar alcohols and big fizzy drinks that can amplify discomfort.
17. Do fennel seeds help with bloating?
They’re a classic after-meal ritual and many people find them soothing. Still, use a small pinch and notice your personal response.
18. Are smoothies good for constipation and bloating?
They can be, if built with calmer ingredients—ripe banana, oats, chia, and water. Yet, avoid large portions of raw crucifers or high-inulin add-ins during flares.
19. What can I eat for bloating when I also suspect food intolerance?
Test one change at a time: smaller portions, lactose-free swaps, or low-FODMAP grains. Then, track results for a week so you can judge each tweak clearly.
20. How do I prevent bloating after eating?
Eat slowly, chew thoroughly, and keep meal sizes steady. Additionally, walk briefly after meals, space fruit portions, and save heavy spice or fat for calmer days.
21. What to eat when bloated with gas at lunch or dinner?
Think “calm templates”: rice with eggs and sautéed spinach; quinoa with tofu and cucumber; moong dal khichdi with ginger and zucchini. Moreover, keep condiments light and portions measured.
22. Do “drinks for digestion and bloating” work better than food changes?
Drinks can help, but food patterning usually leads the way. Ultimately, combine both: gentle meals, warm non-fizzy sips, and consistent routines.
23. Does apple cider vinegar reduce bloating?
Evidence is limited for bloating relief. Even so, if you enjoy it, dilute thoroughly and keep quantities small, especially if you have reflux.
24. What to eat when bloated with gas first thing in the day?
Begin with easy foods: oats or rice porridge, ripe banana, or eggs with sautéed zucchini. Afterward, add a brief walk to encourage movement without jostling.
25. Can bone broth help with bloating?
It’s gentle, warm, and simple, which many people appreciate during flares. Nevertheless, it’s not a cure; pair it with portion control and slower eating.
26. How do I stop bloating after eating out?
Order smaller plates, choose still water, and skip heavy raw piles. Likewise, consider an enzyme with first bites if beans or crucifers are likely.
27. What to eat when bloated with gas if I’m also constipated?
Lean on soluble fiber: oats, chia, kiwi, and small doses of psyllium with adequate fluids. Meanwhile, keep carbonated drinks and large raw salads for calmer days.
28. Why does bloating happen after every meal?
Often it’s a mix of speed-eating, portion size, and fermentable carbs. Therefore, slow down, reduce stacking, and trial simpler menus for a week.
29. What’s the best “debloating drink” before bed?
Choose a warm, non-fizzy beverage in a modest cup and sip unhurriedly. Above all, leave enough time between dinner and bedtime for comfortable digestion.
30. When should I see a doctor about chronic bloating?
Seek care promptly with red flags such as weight loss, rectal bleeding, persistent vomiting, fever, or anaemia. Otherwise, if symptoms persist despite careful changes, book a review to rule out other causes.
Keep Reading (Our Internal Posts)
- Explore soothing blends in teas for digestion, bloating, and gut health.
- Learn simple ways to use saunf in fennel seeds for digestion, freshness, and calm.
- Stock easy ideas from foods that help you debloat.
- Brew a reliable mint routine with peppermint tea for IBS and bloating.
Key External References & Sources
- ACG Clinical Guideline—IBS (diet, soluble fibre, peppermint): overview and full PDF
- Monash FODMAP on FODMAP stacking and serving size
- Ginger and gastric emptying: 2023 review
- α-galactosidase for gas after fermentables: PubMed abstract and trial PDF
- Lactose strategies: NHS Inform and NHS dairy & alternatives
- Fructans vs gluten (Skodje et al., Gastroenterology): PubMed and ScienceDirect