Let’s be honest: Most of us living with diabetes—or supporting someone who is—have heard about “miracle” foods, magic supplements, and endless hacks that promise easier blood sugar control. Apple cider vinegar (ACV) has topped that list for years, popping up everywhere from social media trends to serious scientific journals. But does it actually work? Who is it for? What can you expect if you try it? Let’s go beyond the hype, break down the latest science, real user experiences, practical tips, and critical safety info so you can decide if ACV deserves a spot in your routine.
What Actually Is Apple Cider Vinegar?
Apple cider vinegar starts life as humble apple juice, which is first fermented by yeast to alcohol, and then by bacteria into acetic acid—the main “active” component. If you buy raw, unfiltered ACV, you’ll see a cloudy mass at the bottom (“the mother”), which contains probiotics and enzymes.
People have used vinegar as a tonic for thousands of years, but in the last decade, it’s exploded as a health trend, especially for weight loss, gut health, and—you guessed it—blood sugar.
What Does Science Say About ACV for Diabetes and Blood Sugar?
Recent research is cautiously optimistic. Here’s what large analyses and individual trials reveal:
- Fasting Blood Sugar (FBS): Controlled studies and dose–response meta-analyses show reductions between 8 and 22 mg/dL in people with type 2 diabetes after several weeks of daily ACV use (usually at 10–30 mL/day).
- HbA1c (the “three-month average” of blood sugar): Some studies report drops of up to 1–1.5 percentage points—most notable when ACV is combined with a healthy eating plan.
- After-meal (postprandial) blood sugar spikes: Multiple trials—and tons of user reports—show that a tablespoon of diluted ACV before or with high-carb meals often blunts the spike that typically follows.
- Insulin & Insulin Resistance: The science here is mixed. Some trials see a rise in insulin, but don’t always see big changes in insulin resistance markers.
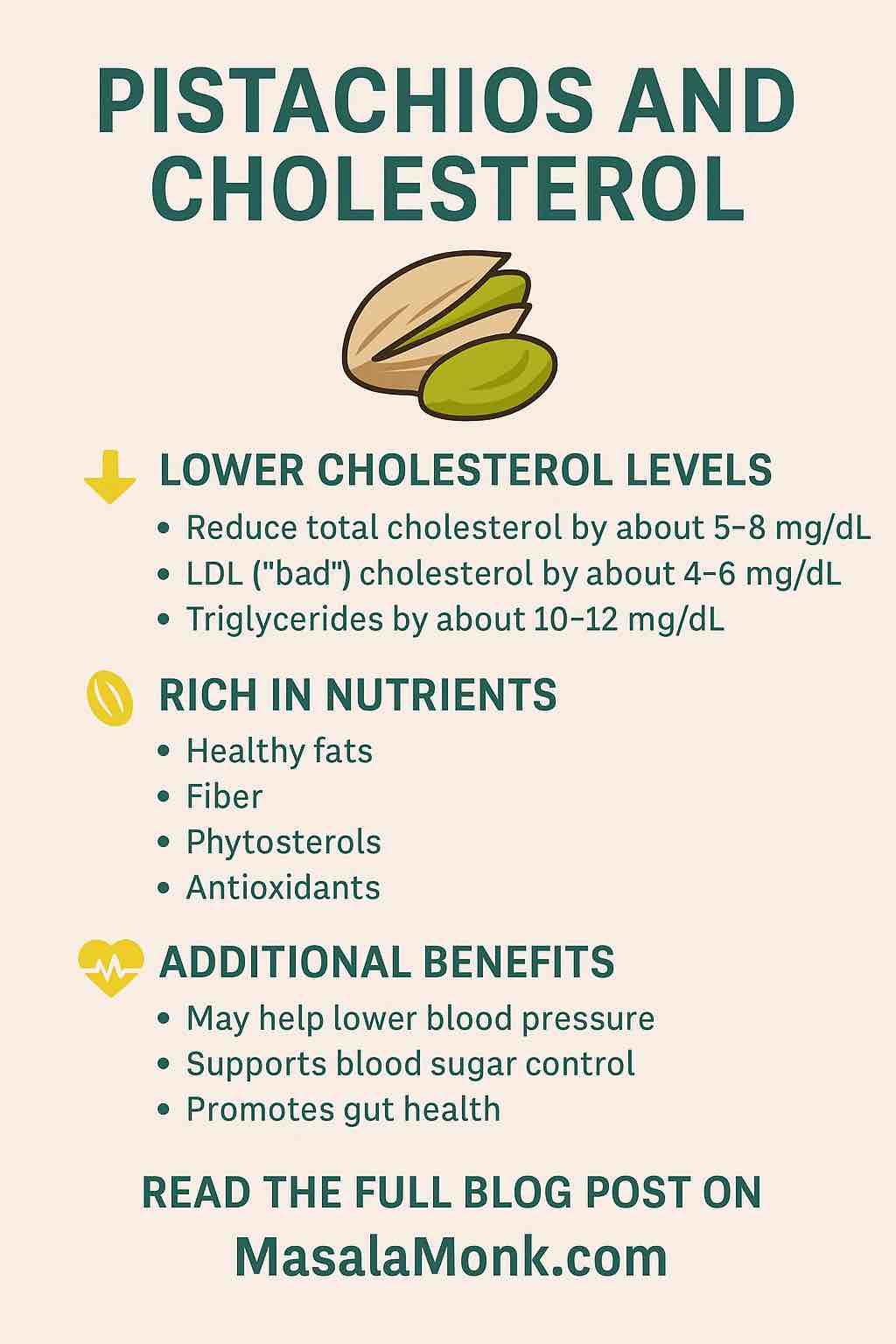
- Cholesterol, Triglycerides & Weight: Some longer studies show modest improvements in LDL (“bad” cholesterol), triglycerides, and even slight reductions in waist circumference or appetite.
The caveat? Most trials are small (30–100 people), relatively short (4–12 weeks), and there’s variation in how ACV is used. That said, results are promising—especially as a low-risk add-on for people with type 2 diabetes or prediabetes.
How Does ACV Work for Blood Sugar? The Science, Simply Explained
It’s not magic—there are actual biological reasons vinegar can impact blood sugar:
- Slows stomach emptying: Acetic acid makes food move through your stomach more slowly, so carbs hit your bloodstream gradually rather than all at once. This means smaller sugar spikes after you eat.
- Improves glucose uptake: Some lab research suggests ACV activates a pathway (AMPK) that helps your muscles soak up more sugar from the blood.
- Reduces sugar production in the liver: ACV contains polyphenols that may tell your liver to make less glucose.
- Suppresses appetite: Some people find vinegar helps them feel fuller faster, which might indirectly help with portion control and blood sugar.
This multi-pronged approach is why many experts see ACV as a helpful “adjunct”—a tool, not a treatment—alongside diet, exercise, and medication.
What Do Real People Say? User Experiences from the Diabetes Community
The best way to balance science is with real stories. Here’s what people are actually experiencing:
“It definitely helps my post-meal spikes.”
“The first morning I tried ACV my spike was only up to 145. The next day, after the same breakfast, it was 125! I just use 1 Tbsp in water before I eat.”
— Type 2 diabetes, Reddit user
“Noticeable difference with high-carb meals.”
“Whenever I have pasta or rice, I take a tablespoon of ACV in a glass of water before eating, and my numbers don’t go as high. Doesn’t work miracles, but it helps.”
— r/diabetes_t2
“Not a fan of the taste, but capsules work.”
“I just can’t stand the vinegar taste, but the ACV capsules seem to work the same for me, as long as I use them before meals.”
— r/prediabetes
“Didn’t notice a big difference.”
“I tried ACV every day for a month and saw no change. Maybe it’s just me, or maybe it works better if you’re insulin resistant.”
— r/diabetes_t2
“Caution: It can cause stomach issues.”
“Don’t drink it straight! I did that once and got bad heartburn. Now I dilute it and use a straw, and it’s fine.”
— r/diabetes_t2
“Best results when combined with other healthy habits.”
“My A1C dropped, but I was also walking more, eating fewer carbs, and drinking ACV. Hard to say how much the vinegar did alone.”
— r/prediabetes
Practical Advice: How to Use ACV for Blood Sugar Management
Want to try it? Here’s a smart, safe way:
- Start slow: Begin with 1 teaspoon (5 mL) of ACV diluted in a big glass of water (8–12 oz, or 240–350 mL).
- Work up to 1–2 tablespoons (15–30 mL) per day if tolerated, split into two or three doses (before main meals).
- Timing: Take ACV 10–20 minutes before meals, especially those with higher carbs.
- Always dilute! Straight vinegar can burn your throat and erode tooth enamel.
- Use a straw to protect your teeth, and rinse your mouth afterwards.
- Don’t overdo it: More is not better. Stay under 2 Tbsp per day unless your doctor advises otherwise.
Easy & Tasty Ways to Use ACV
- Classic ACV Tonic
- 1 tablespoon ACV
- 8–12 oz cold or warm water
- Optional: squeeze of lemon, dash of cinnamon, or a few drops of stevia
- Simple Vinaigrette
- 2 tablespoons olive oil
- 1 tablespoon ACV
- Pinch of salt, pepper, a squirt of mustard
- In Your Food
- Splash over roasted veggies or greens
- Stir into soup or add to a marinade
- ACV Capsules
- Look for standardized products with clear acetic acid content
- Great if you dislike the taste, but always check for fillers/additives
Are There Risks? Who Should Be Careful?
Most people tolerate ACV well—if it’s diluted. But there are risks and situations where you should avoid or use caution:
- Tooth enamel erosion: Vinegar is acidic. Dilute it, use a straw, rinse your mouth.
- Throat or stomach irritation: If you have reflux, ulcers, or sensitive digestion, start slow or avoid altogether.
- Low potassium: Rare, but possible, especially if you’re on certain diuretics or insulin. Monitor your bloodwork.
- Medication interactions: ACV can potentially amplify the effects of blood sugar-lowering meds—leading to hypoglycemia.
- Chronic kidney disease, stomach ulcers, or serious dental issues: Avoid unless cleared by your doctor.
If in doubt, check with your healthcare provider before adding ACV, especially if you’re on medications, have GI issues, or chronic conditions.
Final Thoughts: Is Apple Cider Vinegar Worth Trying?
Apple cider vinegar isn’t a “miracle cure”—but it isn’t snake oil either. If you have type 2 diabetes or prediabetes, there’s credible science and thousands of real-world reports suggesting ACV can help blunt post-meal blood sugar spikes, modestly lower fasting glucose, and support better A1C—especially when used alongside healthy eating and regular activity.
It’s simple, cheap, low-risk when used correctly, and fits easily into most routines. The biggest effects tend to show up when:
- You’re using it as part of a consistent, balanced routine
- You use it with, or just before, meals (especially starchy or carb-heavy ones)
- You’re tracking your response with a glucose meter or CGM, so you can see what works for you
But remember: The real foundation of diabetes management is still what you eat, how you move, your sleep, stress, and medications when needed. ACV is a helpful “extra,” not a replacement.
Pro tip: Try tracking your before-and-after meal glucose a few times a week when you add ACV, and see how your body responds. If you notice consistent improvements (and no side effects), it might just be a simple win worth keeping in your toolkit.
Questions, stories, or recipes to share? Drop them below!
Frequently Asked Questions (FAQs)
1. How much apple cider vinegar should I take to help manage blood sugar?
Most studies suggest 1–2 tablespoons (15–30 mL) per day, diluted in at least one cup of water, is effective and safe for most people. Start with 1 teaspoon (5 mL) to assess your tolerance, and never exceed 2 tablespoons per day without consulting your healthcare provider.
2. When is the best time to take ACV for blood sugar control?
Taking ACV 10–20 minutes before a meal—especially one high in carbohydrates—seems most effective for reducing post-meal blood sugar spikes.
3. Should I drink ACV straight?
No, never drink it undiluted! Always mix it with water or use it in salad dressings or food to avoid damaging your teeth and irritating your throat or stomach.
4. Can I take ACV if I’m on diabetes medication?
Possibly, but check with your healthcare provider first. ACV can enhance the effect of blood sugar-lowering meds, increasing the risk of hypoglycemia in some people.
5. Do ACV capsules or gummies work as well as the liquid?
Some people find capsules or gummies convenient, but their acetic acid content varies. Look for reputable brands and standardized dosages, but be aware: research focuses mostly on the liquid form.
6. Are there any side effects of taking apple cider vinegar?
Potential side effects include tooth enamel erosion, throat or stomach irritation, and low potassium levels (especially with certain meds). Always dilute ACV and start slow.
7. Can ACV replace my diabetes medication or other treatments?
No. ACV is an adjunct—not a substitute—for prescribed medication, healthy eating, and exercise. Never stop your meds without your doctor’s guidance.
8. How soon will I notice a difference in my blood sugar?
Some people see a difference in post-meal blood sugar within days, while fasting glucose and HbA1c may take several weeks to months to improve. Track your readings for personalized results.
9. Is it safe for everyone with diabetes to use ACV?
Most people tolerate ACV well if diluted, but avoid it if you have stomach ulcers, severe acid reflux, chronic kidney disease, or significant dental issues—unless cleared by your doctor.
10. What’s the best way to include ACV in my diet if I don’t like the taste?
Try using ACV in salad dressings, marinades, or diluted with lemon and a touch of stevia or cinnamon to mask the flavor. ACV capsules are an option, but check for reliable brands and dosages.