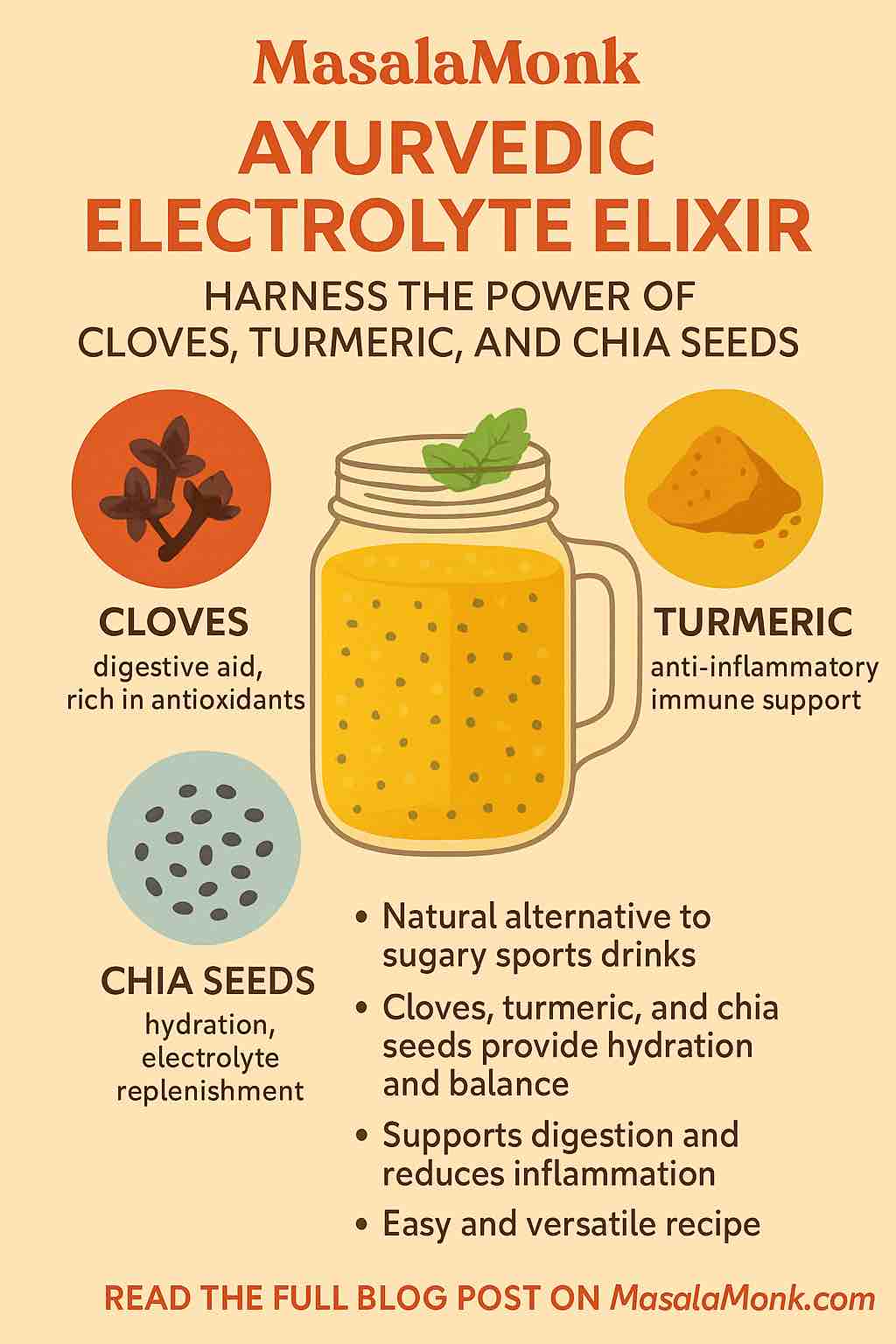
Tired of reaching for artificial sports drinks every time you feel dehydrated or drained? There’s a better way—a recipe that blends the wisdom of Ayurveda with modern science, featuring the remarkable trio of cloves, turmeric, and chia seeds.
Whether you’re sweating it out at the gym, recovering from an illness, or just looking to supercharge your daily hydration, this elixir offers more than just a thirst-quencher. Let’s dive deep into how these ingredients work together, why science backs their synergy, and how you can start sipping today.
What’s an Electrolyte Elixir—And Why Ayurveda?
Electrolytes—like sodium, potassium, magnesium, and calcium—are vital minerals that maintain your body’s fluid balance, nerve function, and muscle health. Lose too many through sweat, exercise, illness, or heat, and you’ll feel the difference: think headaches, cramps, fatigue, or even dizziness.
Modern sports drinks try to replace these, but often contain artificial colors, flavors, and loads of sugar. Ayurveda, India’s ancient system of medicine, offers natural alternatives using kitchen spices and seeds. An elixir in Ayurveda isn’t just about hydration; it’s about balance—nourishing your body, mind, and even your mood.
Meet the Power Trio
1. Chia Seeds: Nature’s Hydration Hack
Chia seeds might not be traditional to Ayurveda, but they fit right in with its principles of holistic hydration:
- Electrolyte-rich: Chia is high in magnesium, calcium, and potassium.
- Gel-forming: Soaked chia swells to form a gel that releases water slowly, keeping you hydrated longer.
- Fiber & Omega-3s: These promote gut health and stable energy.
- Modern science: Studies show chia seeds support sustained hydration and electrolyte balance (PubMed).
2. Turmeric: The Golden Healer
Turmeric (Haridra in Ayurveda) is famed for:
- Anti-inflammatory & antioxidant power (thanks to curcumin)
- Support for liver and digestive health
- Tridoshic action: Suitable for all body types, balances excess heat and toxins
- Immunity boost: Recent studies (2024–2025) reinforce turmeric’s immune-modulating effects and support for gut health
3. Cloves: Digestive Dynamo
Cloves (Lavanga) aren’t just for chai! They offer:
- Warming and digestive properties: Stimulate the “agni” or digestive fire
- Antimicrobial and antioxidant activity (due to eugenol)
- Relief from bloating and nausea
- Science-backed: Modern research validates cloves for gut comfort and immune support
Why This Combo Works: The Science of Synergy
- Electrolyte Restoration: Chia delivers minerals; a pinch of Himalayan salt adds sodium for full-spectrum balance.
- Digestive Harmony: Turmeric and cloves prevent digestive heaviness or discomfort often caused by regular electrolyte drinks.
- Sustained Hydration: The gel from soaked chia means your cells get water slowly and steadily—ideal after a workout, in hot weather, or even during fasting.
- Anti-inflammatory & Antioxidant Shield: Turmeric and cloves guard against inflammation, support recovery, and help your immune system function optimally.
- Improved Nutrient Absorption: Black pepper (optional) can be added to boost curcumin absorption; a little fat (like coconut oil or ghee) increases bioavailability even more.
How to Make Your Ayurvedic Electrolyte Elixir
You’ll need:
- 1 cup filtered or coconut water (for extra potassium)
- 1 tablespoon chia seeds (soaked 10–15 minutes)
- 1/4 teaspoon turmeric powder (organic preferred)
- 1–2 whole cloves (lightly crushed) or 1/8 teaspoon clove powder
- Pinch of black pepper (optional)
- Pinch of Himalayan pink salt or rock salt
- 1 teaspoon raw honey or jaggery (optional, to taste)
- Juice of half a lemon (for vitamin C and flavor)
Instructions:
- Soak the chia seeds in water (or coconut water) for at least 10 minutes, until a gel forms.
- Add the turmeric, cloves, black pepper, salt, and sweetener. Mix thoroughly.
- Squeeze in fresh lemon juice just before drinking.
- Stir well and enjoy—preferably at room temperature or slightly warm (especially good for Vata types).
Dosha-Friendly Customizations
- Vata (dry/cold): Use warm water, add a touch of ghee or coconut oil for grounding.
- Pitta (hot/intense): Use more coconut water and less black pepper; focus on the cooling effects of chia.
- Kapha (slow/damp): Amp up the cloves and turmeric, minimize the sweetener.
When & How to Use
- Post-workout: Rehydrate and restore lost minerals.
- Hot days: Keep your system cool and balanced.
- During illness: Especially if you have fever, diarrhea, or dehydration—sip slowly for maximum absorption.
- As a daily ritual: Start your morning or break your fast with this elixir for sustained energy and hydration.
Pro Tips for the Best Results
- Always soak chia before consuming to avoid digestive discomfort.
- Go easy on the cloves—a little goes a long way!
- Choose organic turmeric for better taste and potency.
- Use honey/jaggery only if needed—don’t over-sweeten; let the spices shine.
- Batch prep: Soak chia ahead of time and keep it in the fridge for a few days’ worth of drinks.
What Does the Latest Science Say?
Turmeric: Bibliometric reviews from 2024–25 show explosive growth in studies confirming curcumin’s role in reducing inflammation, improving immunity, and supporting gut health.
Chia Seeds: 2025 wellness guides (and even TikTok trends) recognize chia’s role in electrolyte balance and long-lasting hydration for athletes, office workers, and everyone in between.
Cloves: Modern analyses reaffirm clove’s ancient reputation for supporting digestion, fighting bacteria, and providing antioxidants.
While there’s still a need for large-scale clinical trials on this exact combination, the science behind each ingredient is strong and continues to grow.
Frequently Asked Questions
1. Can I prepare the Ayurvedic Electrolyte Elixir in advance?
Yes, you can soak chia seeds in advance and refrigerate the gel for up to 3 days. For the freshest flavor and maximum potency, add turmeric, cloves, lemon, and salt just before drinking.
2. Is this elixir safe for people with medical conditions?
Generally, it’s safe for most, but if you have allergies, take blood thinners (due to turmeric), or have kidney issues (because of minerals), consult your healthcare provider first.
3. Can I substitute ingredients if I don’t have all three?
Yes! You can use just one or two of the core ingredients. For example, swap chia for soaked basil seeds (sabja) or use ginger instead of cloves if you prefer.
4. Does this drink actually replenish electrolytes like commercial sports drinks?
It provides magnesium, potassium, calcium (from chia), sodium (from salt), and trace minerals. For extreme fluid loss (e.g., heavy sweating, illness), you may need to increase the salt slightly for adequate sodium.
5. Is the elixir suitable for children and seniors?
Yes, but use mild amounts of turmeric and cloves for kids. Skip honey for children under 1 year. For seniors, this elixir is gentle and hydrating, but always check for potential interactions with medications.
6. Can I drink it during fasting or intermittent fasting?
Absolutely. It’s low in calories, supports hydration, and won’t break a fast if you skip sweeteners. The electrolytes and fiber also help prevent dehydration and energy dips.
7. Does it have to be served warm or cold?
Either works! Ayurveda often recommends room temperature or slightly warm drinks for digestion, but on hot days, cold (not iced) is refreshing and effective.
8. What’s the best time to consume this elixir?
Morning is ideal for starting your hydration, after workouts for recovery, or anytime you feel depleted or overheated. It can also help after mild illness.
9. Will turmeric stain my teeth or containers?
Turmeric can stain plastic and some porous surfaces, so use glass containers and rinse promptly. For teeth, regular brushing prevents noticeable staining.
10. Can I add other flavors or herbs?
Definitely! Mint, ginger, cardamom, or rosewater can be added for flavor and extra benefits. Just keep the base ingredients to maintain electrolyte balance.
Final Thoughts
This Ayurvedic Electrolyte Elixir is more than a drink—it’s a ritual of nourishment and self-care. It bridges the wisdom of the ancients with the discoveries of modern wellness science. Next time you’re tempted by a bottle of neon-colored sports drink, try this instead. Your body—and your taste buds—will thank you.
Ready to try it? Share your variations, tips, or experiences in the comments below!
Curious about the science? Check the references for the latest research and deep dives on each ingredient.
Stay hydrated, stay balanced, and embrace the best of both worlds—naturally.