There’s something wonderfully honest about a whiskey sour. No smoke and mirrors, no mile-long ingredient list—just whiskey, citrus, and sweetness, shaken together until they become more than the sum of their parts. Whether you like yours sharp and bracing, frothy with egg white, or dressed up with a red wine float as a New York sour drink, mastering a great whiskey sour recipe gives you a whole family of cocktails to play with.
Let’s walk through it slowly, glass in hand.
What Exactly Is a Whiskey Sour?
At its core, a whiskey sour cocktail is a “sour”: one spirit, one citrus, one sweetener. That template shows up everywhere in cocktail culture—margaritas, daiquiris, sidecars—but the whiskey sour drink might be the most comforting of the lot.
In its simplest form, you’re working with:
- Whiskey
- Fresh lemon juice
- Sugar (usually as simple syrup)
Shake it with ice, strain it into a glass, garnish if you like, and you’re done. That’s your basic answer when someone asks, “What’s in a whiskey and sour?” or “What’s the whiskey sour cocktail recipe?”
Over the years, bartenders have added little twists:
- A splash of egg white to create the creamy Boston Sour
- A float of dry red wine to turn it into a dramatic New York whiskey sour
- Swapping in different sweeteners (honey, maple, ginger syrup)
- Experimenting with different styles of whiskey—bourbon, rye, Irish, Scotch
Yet the structure stays the same. Spirit, sour, sweet. Once you understand that, you can see how every sour whisky drink you encounter is just a variation on this backbone.
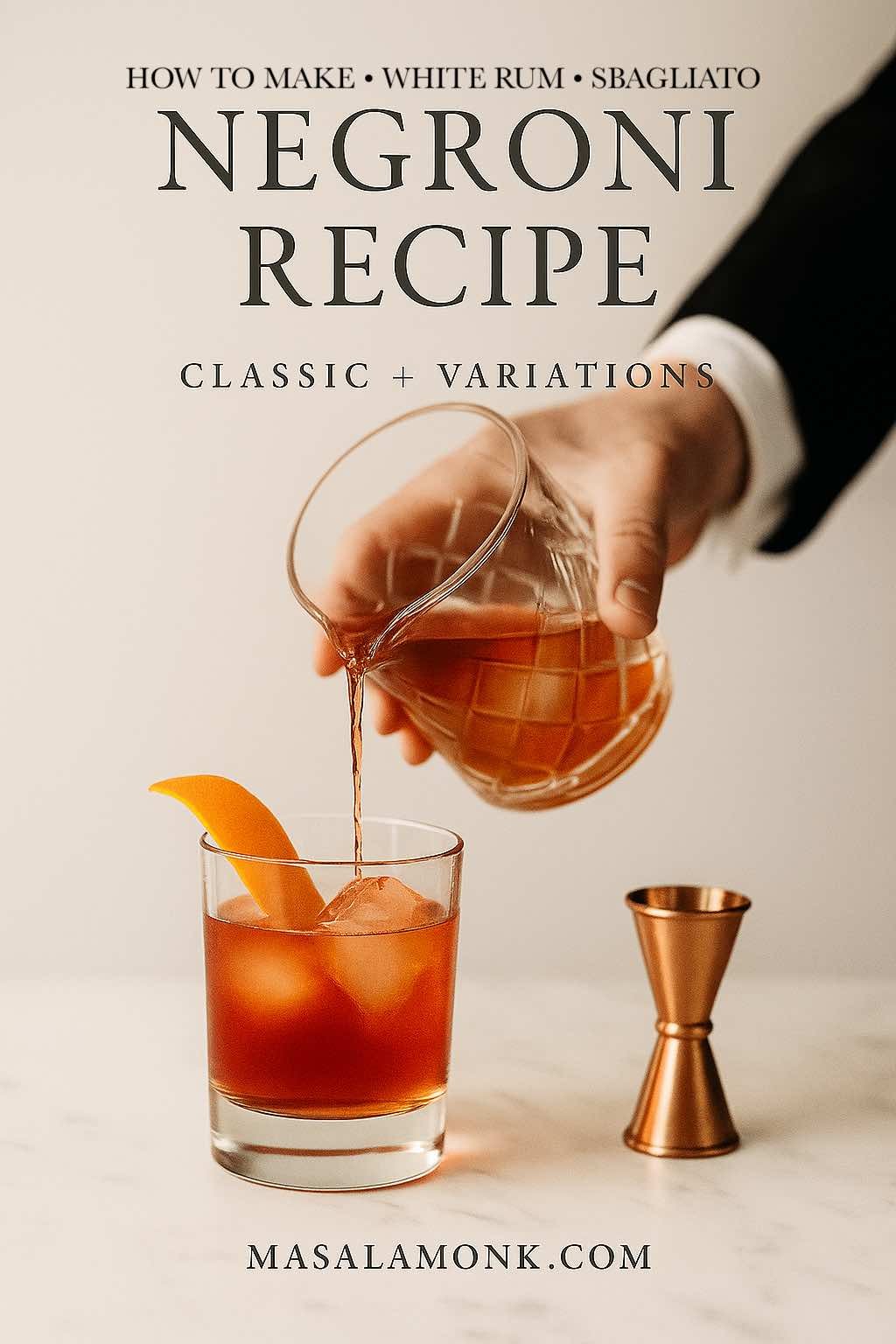
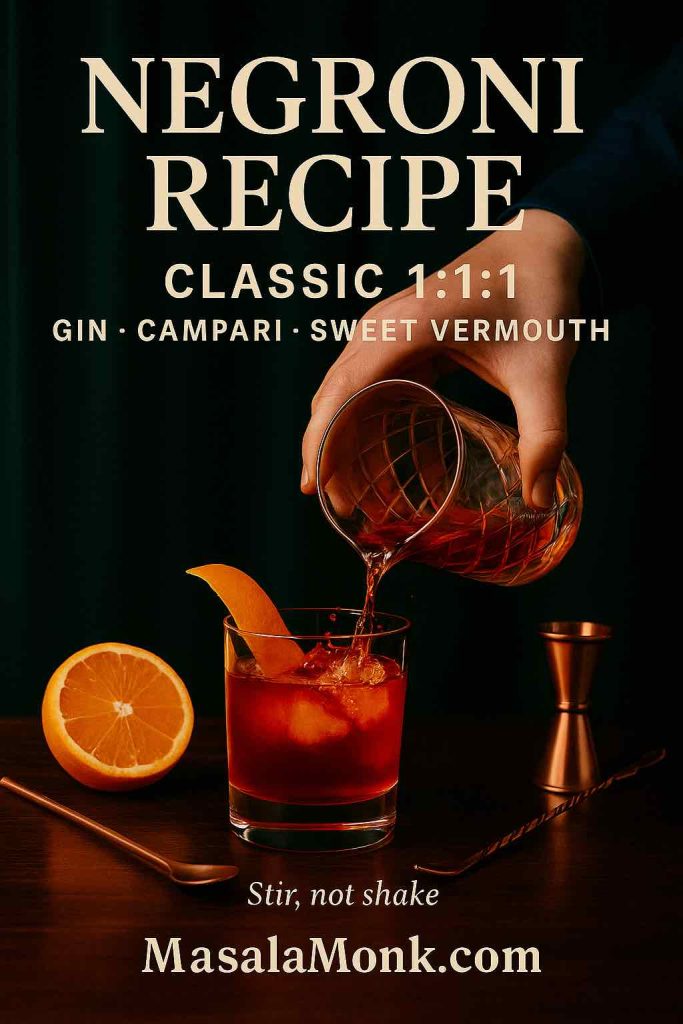
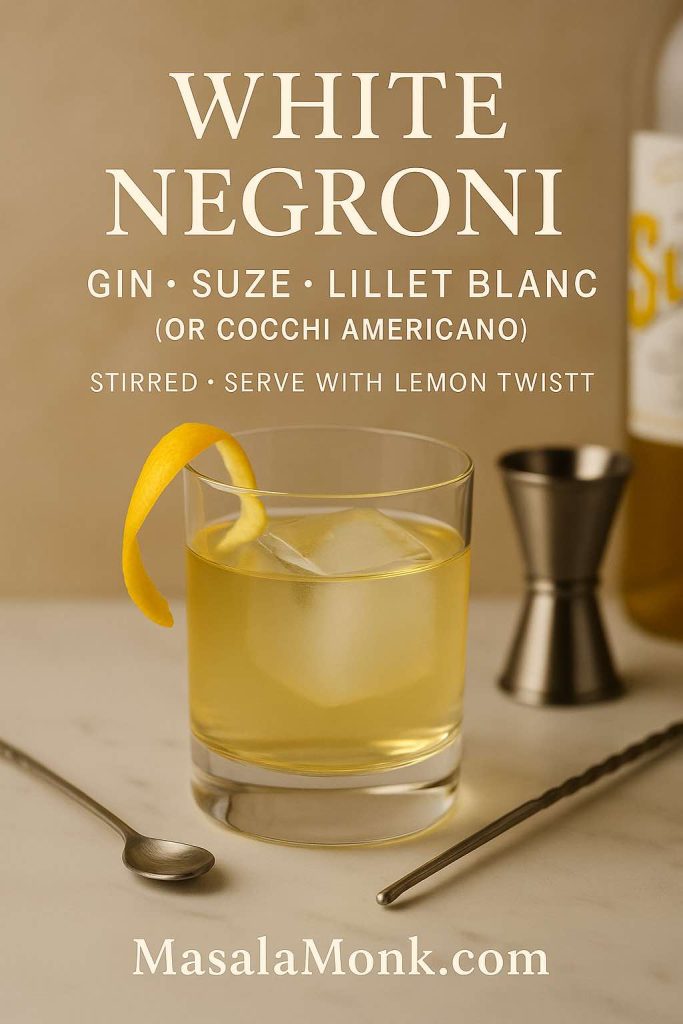
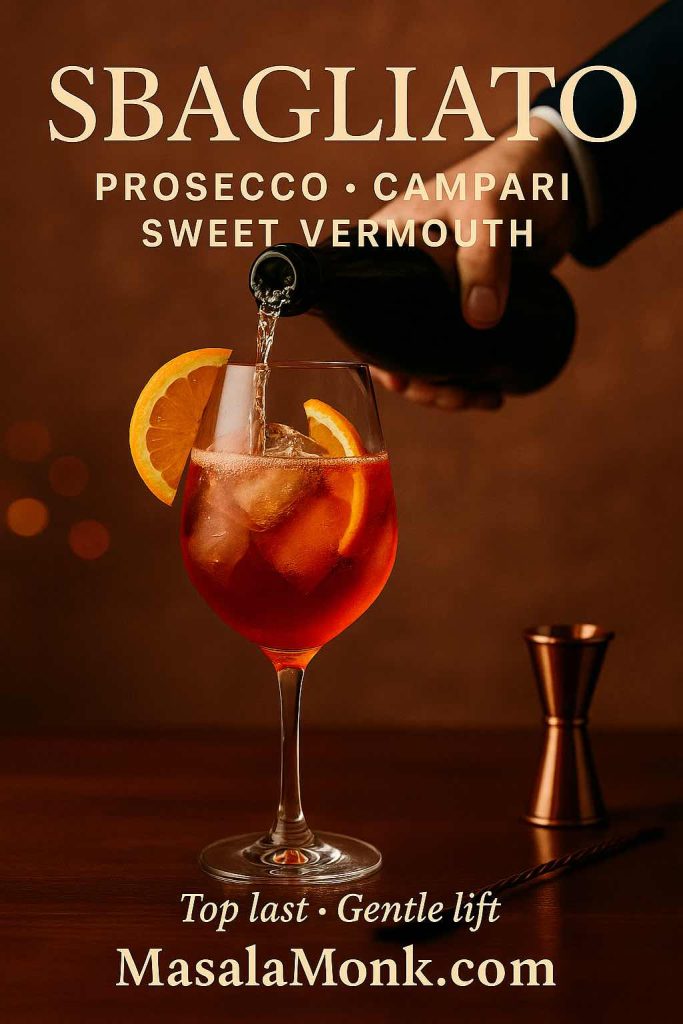
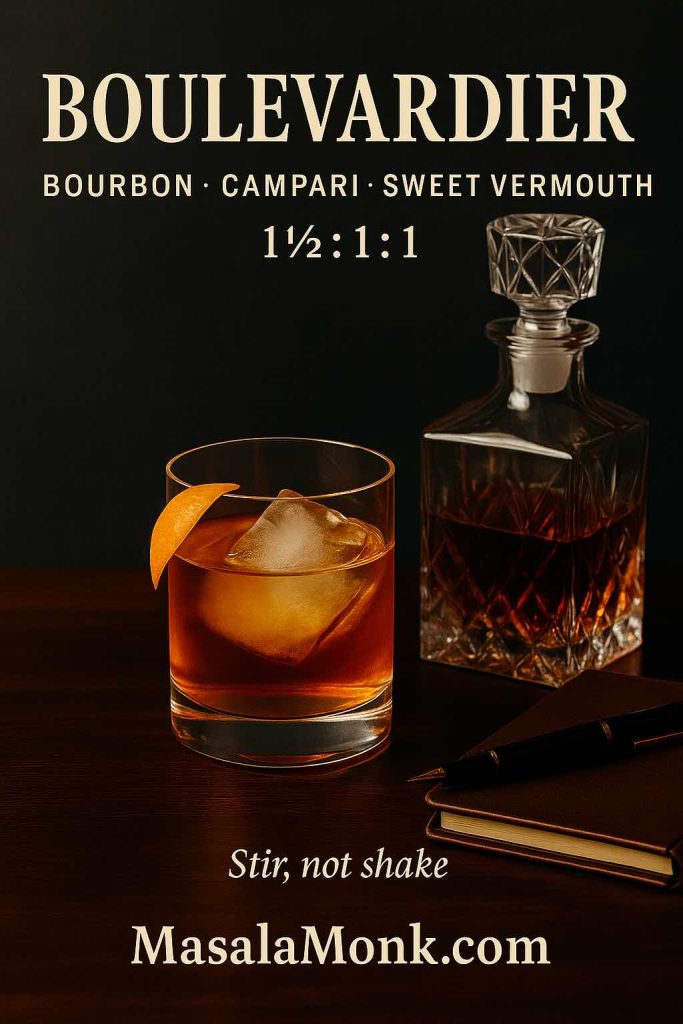
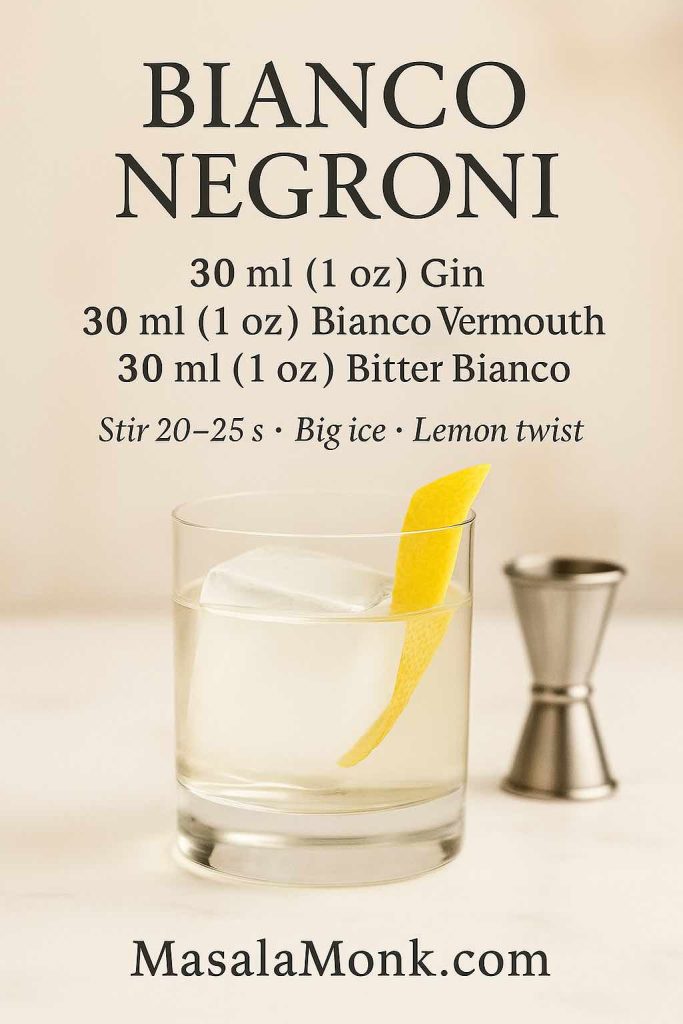
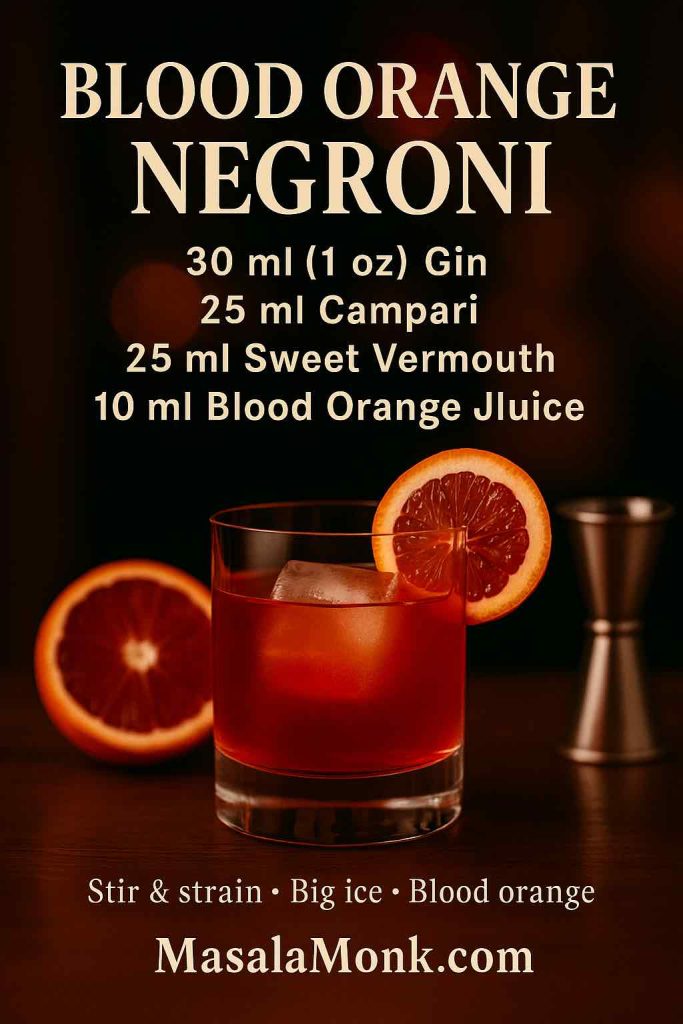
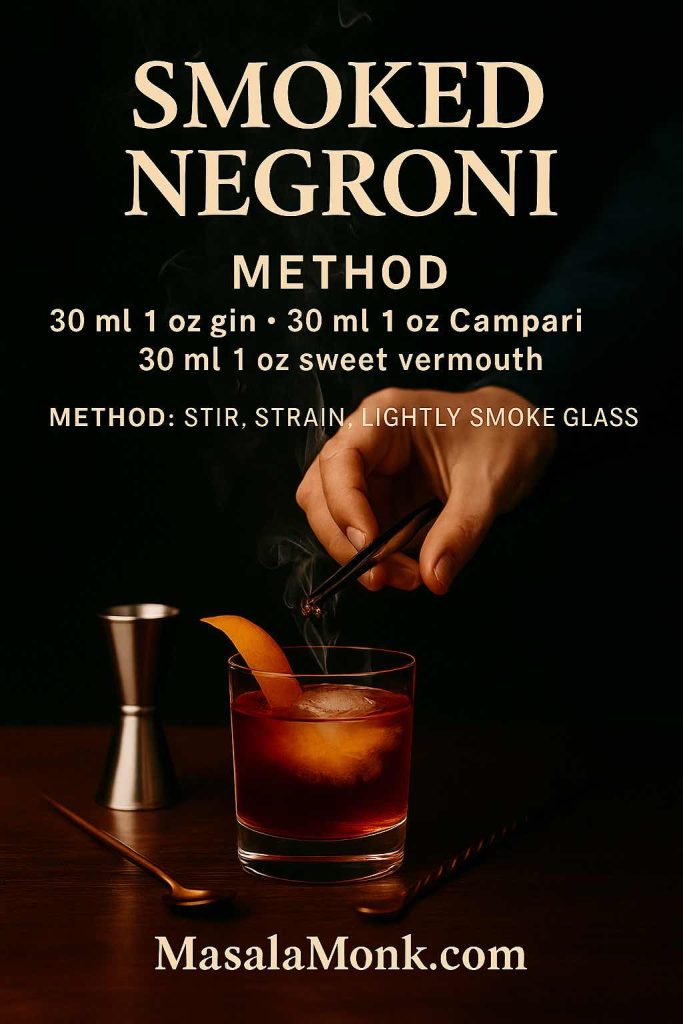
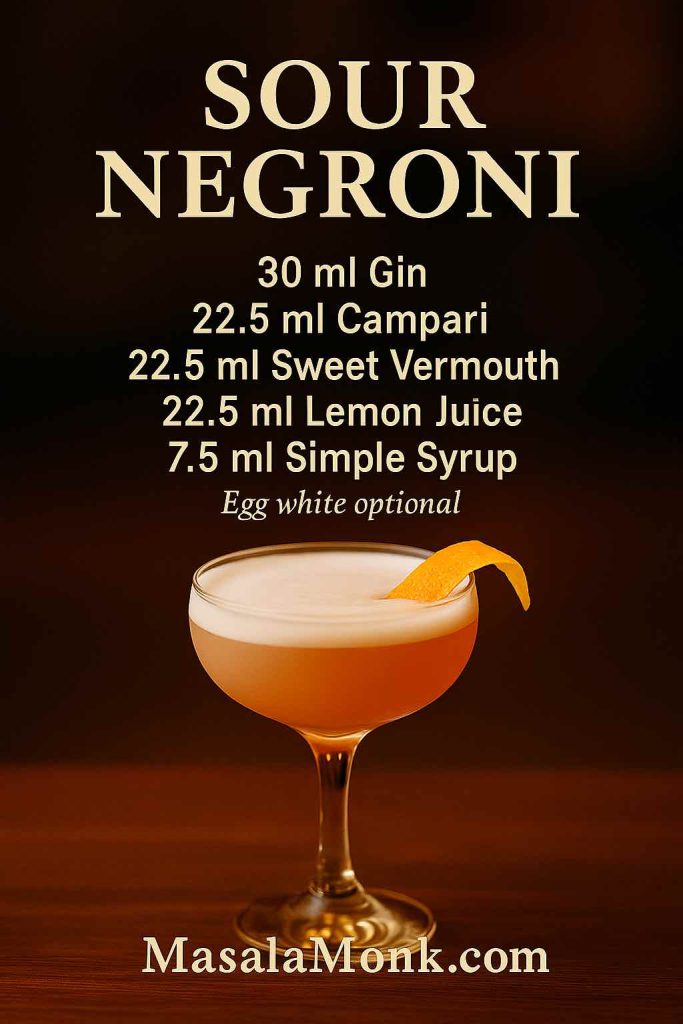
Also Read: Negroni Recipe: Classic Cocktail & Its Variation Drinks
A Short, Spirited History
Like many great drinks, the traditional whiskey sour grew out of necessity. Long before cocktail bars and Instagram, sailors mixed spirits with lemon or lime juice and sugar to ward off scurvy and make rough spirits more palatable on long voyages. Over time, that practical mixture migrated onto dry land and into early American bars.
By the mid-19th century, manuals like Jerry Thomas’s Bartender’s Guide were formalizing the idea of “sours”—brandy sour, gin sour, whiskey sour. The original whiskey sour recipe would have been pretty rustic by modern standards: spirit, citrus, and powdered sugar, maybe with a bit of water to help it dissolve.
Fast forward to today, and the drink still follows the same logic, though we’ve traded powdered sugar for simple syrup, added the option of egg white, and fine-tuned the whiskey sour ratio so it suits modern palates. Meanwhile, new variations keep spinning off—from the red-wine-topped New York sour cocktail recipe to maple- and spice-laced twists like the Nutmeg Maple Whiskey Sour you’ll find in Masala Monk’s nutmeg-inspired cocktails for Saturday nights.
The drink has evolved, but its spirit hasn’t changed much: a simple, reliable way to turn whiskey and lemon into something you want to linger over.
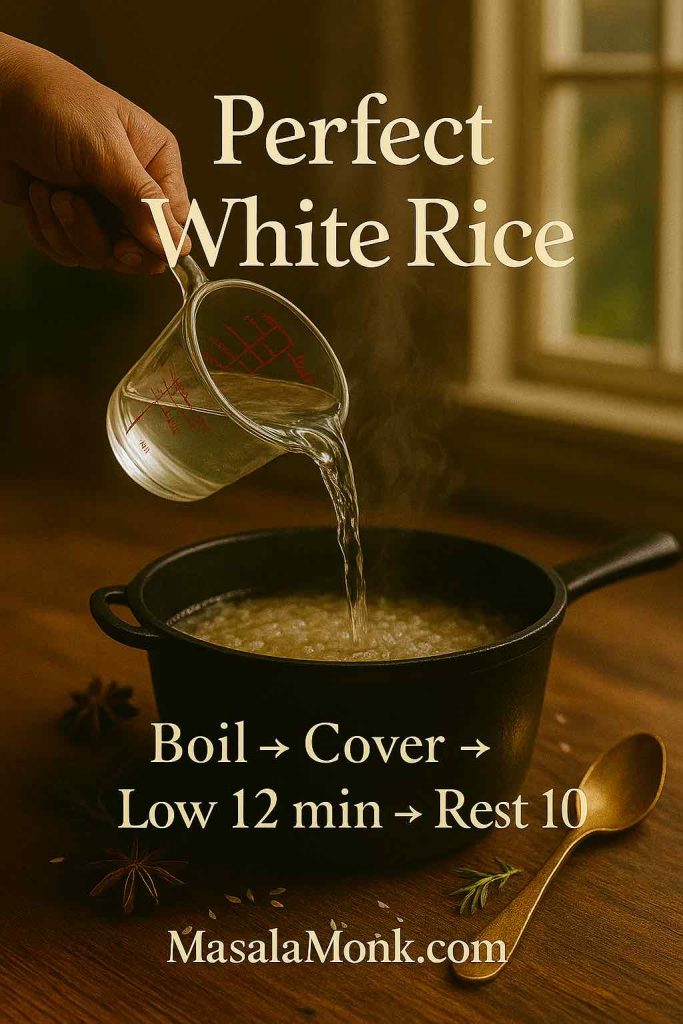
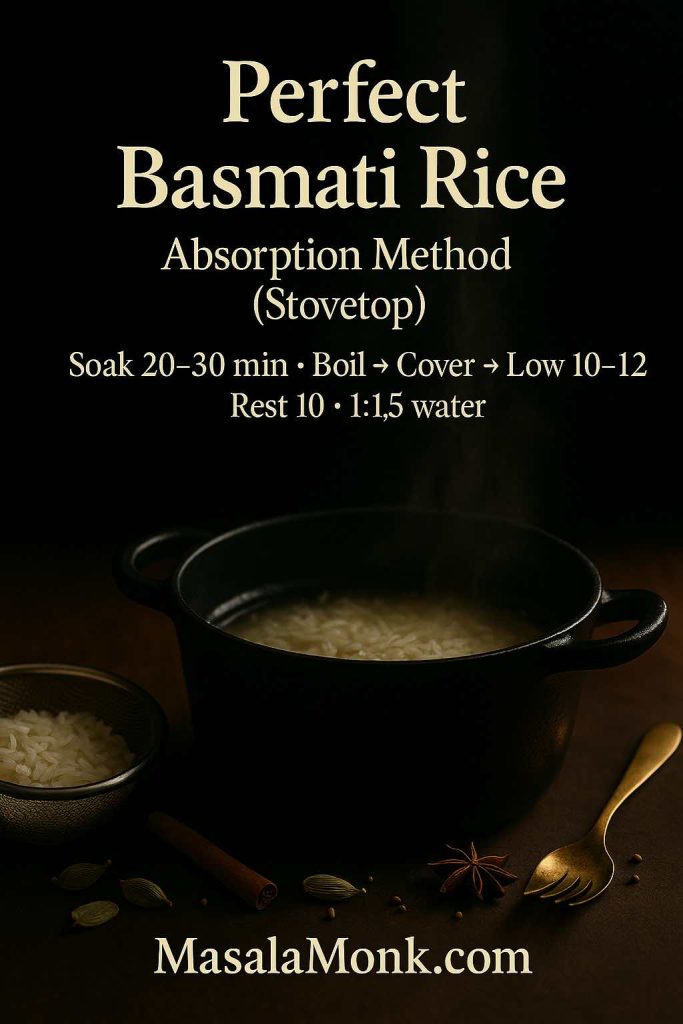
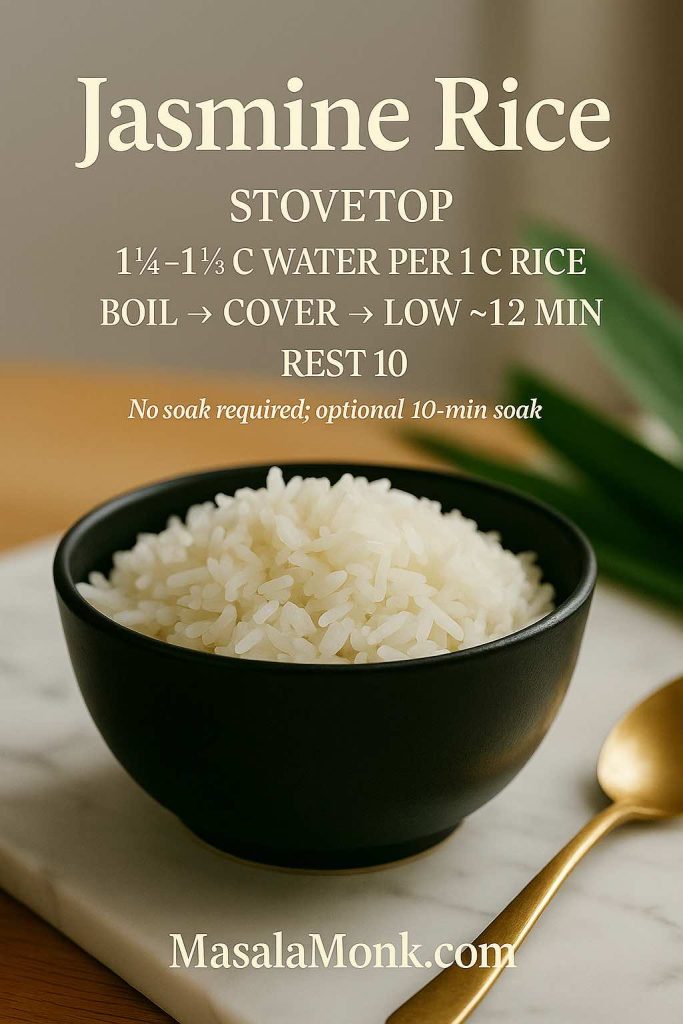
Also Read: How to Cook Perfect Rice Every Time (Recipe)
Whiskey Sour Ingredients: The Building Blocks
Before shaking, it helps to get familiar with the core whiskey sour ingredients and why they matter.
1. Whiskey
The whiskey is your base, so choose wisely. Almost any style can work:
- Bourbon – The default for a bourbon whiskey sour and bourbon sour. It’s naturally sweet, with notes of vanilla and caramel that play beautifully with lemon.
- Rye – Spicier and drier, great for a rye whiskey sour if you like more bite.
- Irish whiskey – Light, smooth, and friendly. Ideal for an easy-drinking Irish whiskey sour or Jameson whiskey sour.
- Scotch – Malty and sometimes smoky. That’s your scotch sour, scotch whiskey sour, or sour scotch, and it can be delicious in the right hands.
Later on, when you’re ready to get very specific about the best whiskey for whiskey sour, you can dip into more brand-focused guides like Masala Monk’s deep dive on what to mix with Jim Beam or bottle lists from cocktail sites that compare bourbon and rye for mixed drinks.
2. Fresh Lemon Juice
Lemon is the “sour in whiskey sour.” It’s what turns a glass of straight spirit into a refreshing lemon whiskey drink and gives the cocktail its signature brightness.
Fresh makes a big difference. Bottled juice tends to taste flat or sharp in the wrong way, while fresh lemons give you aroma and zest along with acidity. If someone asks about whiskey and lemon juice or drinks with whiskey and lemon, this is the heart of the answer: fresh citrus, not shelf-stable juice.
3. Sweetener
Traditional recipes used sugar and water; today, most bartenders reach for:
- Simple syrup – Equal parts sugar and water, dissolved. This is the most common simple syrup for whiskey sour and makes it easy to adjust sweetness.
- Maple syrup – For a maple whiskey sour, especially in colder weather.
- Honey syrup – For a honey lemon whiskey sour, floral and cozy.
- Ginger syrup – For a ginger whiskey sour with a warming kick.
Even if you’re using a flavoured syrup, the logic is the same: balance the lemon with enough sweetness that the cocktail tastes harmonious rather than punishingly sour.
4. Egg White (Optional)
Egg white is technically optional, but if you’ve ever admired a cocktail with a thick, silky foam on top, you’ve seen what it can do. Adding a small amount and shaking properly turns your drink into a luscious whiskey sour with egg white—what many people call a Boston Sour.
You’ll also see recipes labelled:
- Whiskey sour cocktail recipe egg white
- Whiskey sour cocktail with egg white
- Whiskey drink with egg white
All of them are describing this creamy variation. We’ll get into the technique in a moment.
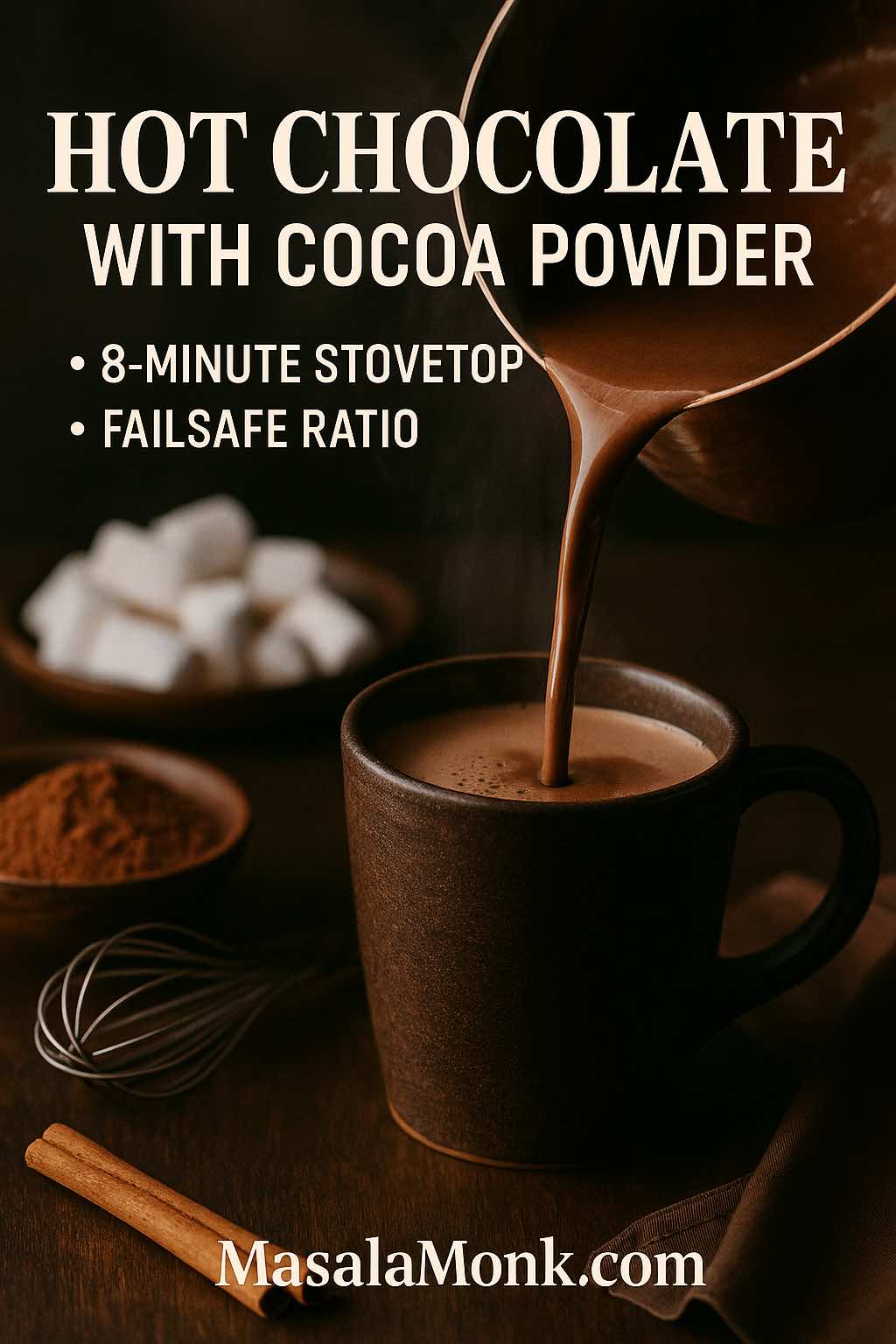
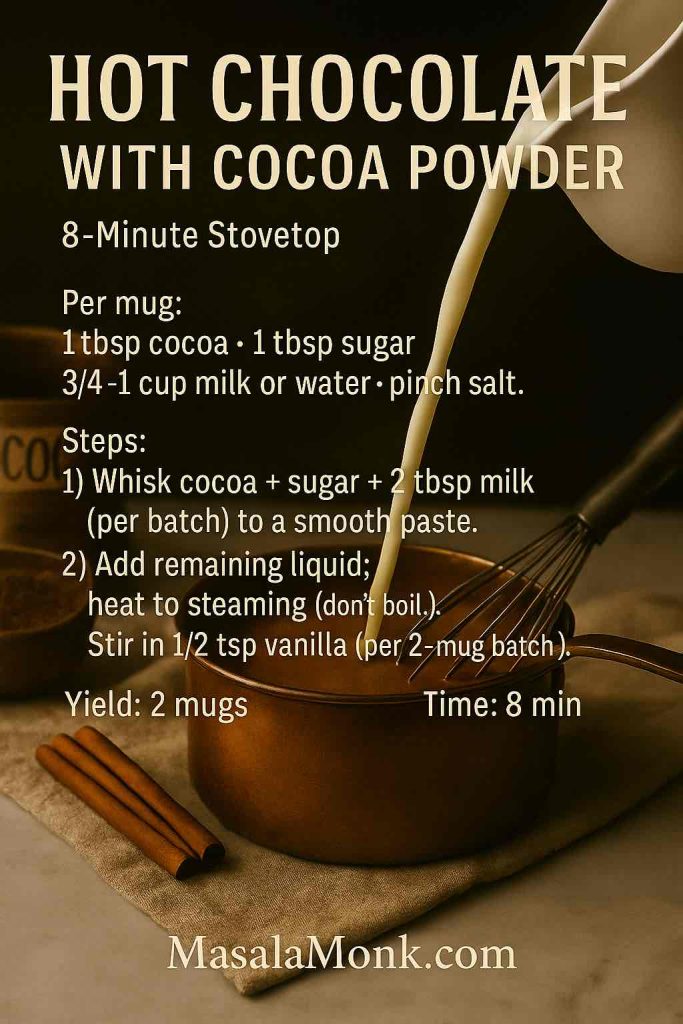
Also Read: Homemade Hot Chocolate with Cocoa Powder Recipe
Classic Whiskey Sour Recipe (No Egg)
Let’s start with the most straightforward whiskey sour recipe: clean, bright, and easy to remember.
Simple Whiskey Sour
This is your go-to simple whiskey sour, perfect for a weeknight drink or a first experiment at home.
Ingredients (1 drink)
- 50 ml (1¾ oz) whiskey
- 25 ml (¾–1 oz) fresh lemon juice
- 20–25 ml (⅔–¾ oz) simple syrup
- Ice
- Lemon wheel or twist, plus a cherry
Think of this as the standard whiskey sour recipe ml and whiskey sour measurements you can rely on. It’s essentially a 2:1:1 whiskey sour ratio, which is easy to scale up.
Method
- Add the whiskey, lemon juice, and simple syrup to a cocktail shaker filled with ice.
- Shake briskly for 10–15 seconds, until the outside of the shaker is frosty.
- Strain into a rocks glass filled with fresh ice.
- Garnish with a lemon wheel or twist and a cherry.
That’s it. In just a few steps, you’ve made an easy whiskey sour from scratch. You can call this your basic whiskey sour, classic whiskey sour, traditional whiskey sour recipe, or just “my house whiskey sour.”
If a friend asks, “How do you make a whiskey sour?” or “How do I make a whisky sour at home?”—this is the version to teach them.
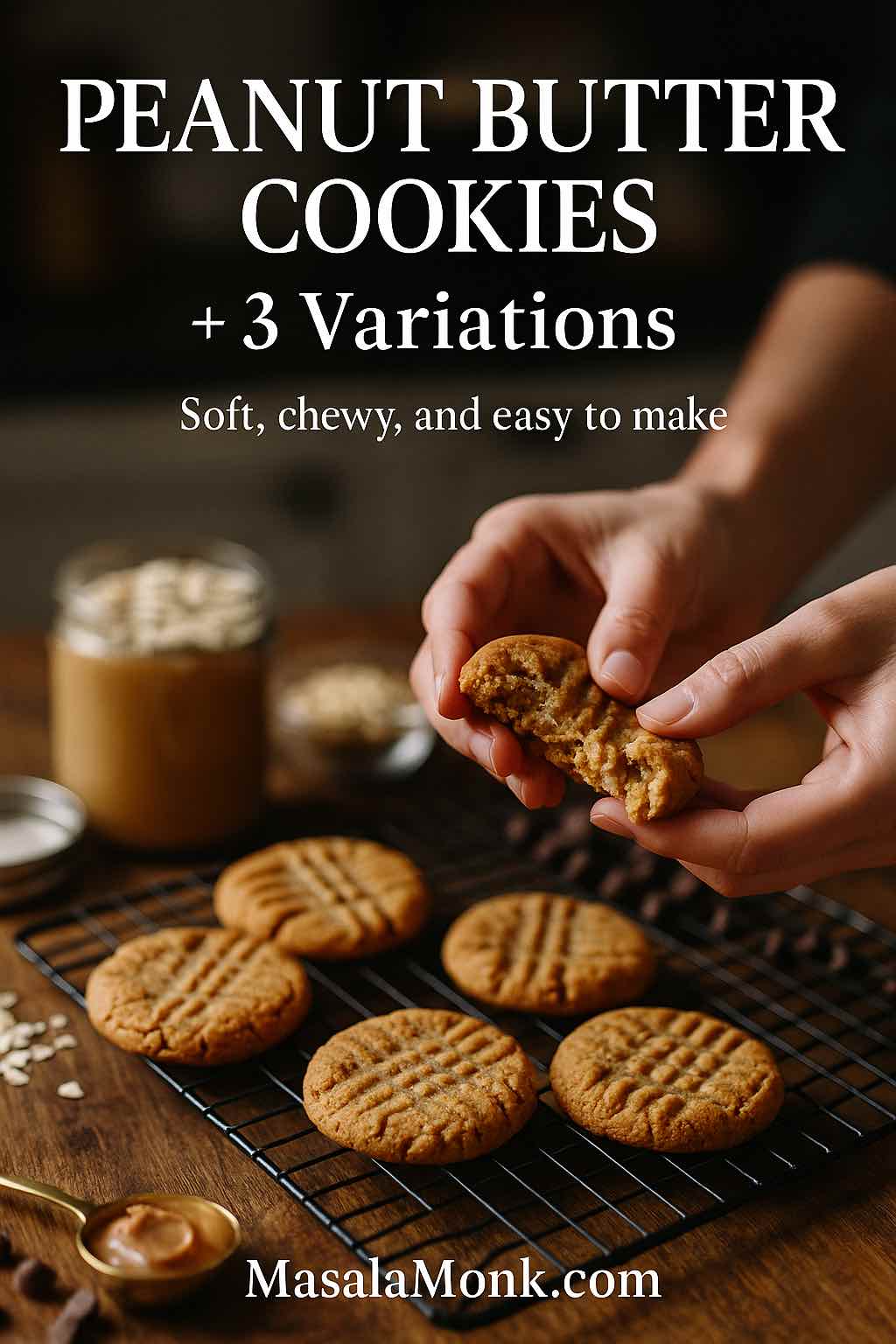
Also Read: Peanut Butter Cookies (Classic Recipe & 3 Variations)
Whiskey Sour Recipe with Egg White (Boston Sour)
Once you’re comfortable with the basic build, you might want to explore the creamy, velvety side of the style: the whiskey sour with an egg white, often referred to as a Boston Sour.
Why Add Egg White?
Egg white doesn’t change the flavour dramatically; instead, it transforms texture. It gives the drink:
- A thick, luxurious foam cap
- A softer, rounder mouthfeel
- A canvas for a few drops of aromatic bitters
That’s why you’ll sometimes see recipes titled egg white whisky sour or boston sour cocktail. They’re all talking about the same technique.
Egg-White Whiskey Sour Recipe
Ingredients (1 drink)
- 50 ml (1¾ oz) whiskey
- 25 ml (¾–1 oz) fresh lemon juice
- 20–25 ml (⅔–¾ oz) simple syrup
- 10–15 ml (⅓–½ oz) egg white (about half the white of a large egg)
- Ice
- Bitters + lemon twist, to garnish
Method
- Add whiskey, lemon, simple syrup, and egg white to a shaker without ice.
- Seal and dry shake for about 10–20 seconds. This whips air into the egg white.
- Open the shaker, add ice, and shake again until chilled.
- Strain into a rocks glass over ice or into a chilled coupe.
- Dot the foam with a few drops of bitters and garnish with a twist.
You now have a lush, restaurant-worthy whiskey sour cocktail. If you want more context about this style and why bartenders swear by the dry-shake method, you can always look to classic recipe resources like Liquor.com’s take on the whiskey sour or similar guides that spell out both the egg and no-egg versions in detail.
Anyone looking for a whisky sour recipe with egg white or a whiskey sour cocktail recipe that looks truly pro will be delighted with this version.
Also Read: Green Tea Shot with Jameson | Recipe & 10 Variations
Whiskey Sour Recipe Without Egg (No-Fuss & Vegan Friendly)
Not everyone is comfortable with egg in a drink, and that’s completely fine. A whiskey sour without egg white is:
- Easier to batch for parties
- Faster to shake on a busy night
- Naturally lighter and more zippy
The good news is you don’t need to change much. The whiskey sour recipe no egg is simply the simple recipe from above: whiskey, lemon, syrup, ice, shake.
You’ll see plenty of variations on the phrase—whiskey sour ingredients no egg, whiskey sour ingredients without egg, whisky sour no egg, whisky sour recipe no egg, whisky sour without egg—but they all boil down to the same thing: a classic, foam-free sour that puts the citrus and whiskey front and centre.
If you still want that foamy look but don’t want to use egg, some bartenders use aquafaba (the liquid from a can of chickpeas) as a vegan substitute. The technique is the same: dry shake first, then shake with ice.
Also read: Béchamel Sauce for Lasagna: Classic, Vegan & Ricotta Sauce Recipe
Whiskey Sour with Sour Mix: Shortcuts That Still Taste Great
Sometimes you’re making one perfect drink for yourself. Other times you’re in full host mode and squeezing lemons for ten people feels like too much. That’s where whiskey sour mix comes in handy.

Using Bottled Mix
For a quick-and-easy whiskey sour with sour mix, try:
- 50 ml (1¾ oz) whiskey
- 75–90 ml (2½–3 oz) commercial sour mix
Shake with ice, strain over fresh ice, garnish. That’s your classic shortcut for a whiskey sour drink mix–based serve.
You might also see this loosely described as:
- Whiskey and sour mix
- Sour mix and whiskey
- Whisky sour with sour mix
- Whiskey sour with sweet and sour mix
If you’re already using sour mix for shots and party drinks, you can keep the same bottle on hand for sours. For instance, if you enjoy the Green Tea Shot with Jameson from Masala Monk—Jameson, peach schnapps, sour mix—that same mix gives you a fast route to a Jameson whiskey sour–style drink in a pinch.
Homemade Whiskey Sour Mix Recipe
For better flavour and more control, it’s worth making your own homemade whiskey sour mix. A simple version:
- 1 part fresh lemon juice
- 1 part fresh lime juice (optional but bright)
- 1 part sugar (stirred into the juice or turned into syrup)
Combine, chill, and you’ve got a versatile lemon sour recipe drink base that works for:
- Classic whiskey sweet and sour highballs
- Batch whiskey sour recipe with sour mix pitchers
- Other sour-style cocktails and even tea-based drinks
Masala Monk’s love affair with tea and whiskey shows up in posts like their cinnamon-spiced iced tea whiskey cocktails and saffron iced tea cocktails, and a homemade sour mix slots perfectly into that style of mixing.
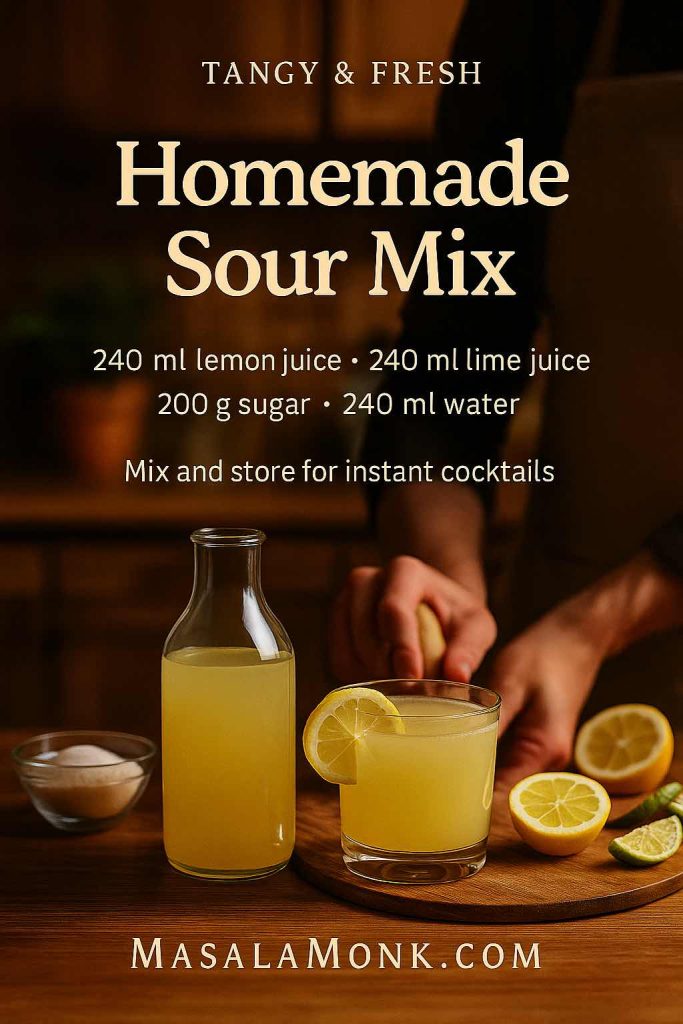
Once your mix is ready, you can use roughly 50 ml whiskey to 75–90 ml of your sour blend for a fast, consistent drink. It may not be as precise as the single-serve whiskey sour from scratch, but it’s very party-friendly.
Also Read: Crock Pot Lasagna Soup (Easy Base + Cozy Slow-Cooker Recipes)
Best Whiskey for Whiskey Sour: Choosing the Right Bottle
Talk to ten bartenders about the best whiskey for whiskey sour recipe, and you’ll get at least twelve opinions. That said, a few patterns show up again and again.
Bourbon
Bourbon is the classic choice for a bourbon whiskey sour or bourbon sour:
- Naturally sweeter, with vanilla, caramel, and baking-spice notes
- Often feels rounder and softer with lemon juice
- Plays nicely with a wide range of sweeteners, from simple syrup to maple
When you’re browsing the shelf, look for a bottle you’d happily sip neat but don’t mind mixing. If you’ve already been experimenting with ideas from “what to mix with Jim Beam” style articles—including highballs, long drinks, and sours—that same Jim Beam or similar bourbon will make a very solid good whiskey for whiskey sour.
Rye
Rye brings more spine to the party. A rye whiskey sour:
- Tastes drier and spicier
- Leans into pepper and baking spice notes
- Works beautifully if you don’t like your cocktails overly sweet
If you already enjoy Manhattan-style drinks, a rye-based sour might feel like the perfect bridge between sharp and refreshing.
Irish Whiskey
For something lighter, Irish whiskey is tailor-made for a whiskey and lemon combination. A Jameson sour or Jameson whiskey sour tends to be:
- Smooth and approachable
- Slightly grassy or cereal-like in a pleasant way
- Great for people who say they “don’t really like whiskey” but enjoy balanced cocktails
In fact, if you’ve made the Green Tea Shot mentioned earlier, you already know how friendly Jameson is with sour mix and citrus.
Scotch & Beyond
Scotch in a sour can be a little more polarizing, yet a good scotch sour drink or scotch sour cocktail can be lovely:
- Blended scotch gives you malt, honey, and a gentle smokiness
- Some peated whiskies add a smoky surprise to the lemon
The same logic applies when you’re playing with other recipes on Masala Monk that feature bourbon or rye—like the cinnamon Old Fashioned–style cocktails or cinnamon-spiced iced tea highballs. If a whiskey works there, it will probably work in a sour too.
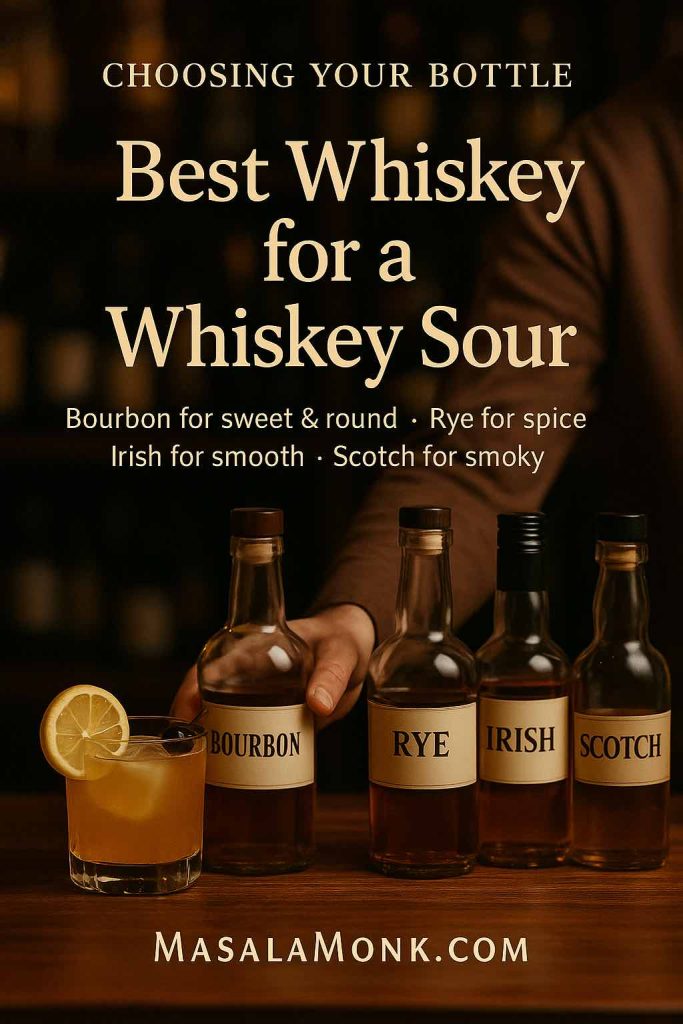
So What’s “Best”?
When people ask for:
- Best whiskey for whiskey sour
- Best whiskey for sour
- Best whisky for a whisky sour
- Whisky sour best whisky
…they’re usually looking for reassurance more than a single magical brand. As a guideline:
Choose a whiskey you’d drink on the rocks, with enough character to stand up to lemon and sugar, but not so precious that you feel guilty shaking it.
That’s your sweet spot.
Also Read: Cottage Cheese Lasagna Recipe | Chicken, Spinach, & Ricotta
Whiskey Sour Variations You’ll Want to Try
Once you’ve locked in your house whiskey sour recipe, you can start branching out. The sour template is incredibly flexible, so experimenting is half the fun.
New York Sour
The New York sour (sometimes called a Continental Sour) is a classic variation that adds a red wine float on top of a standard whiskey sour.
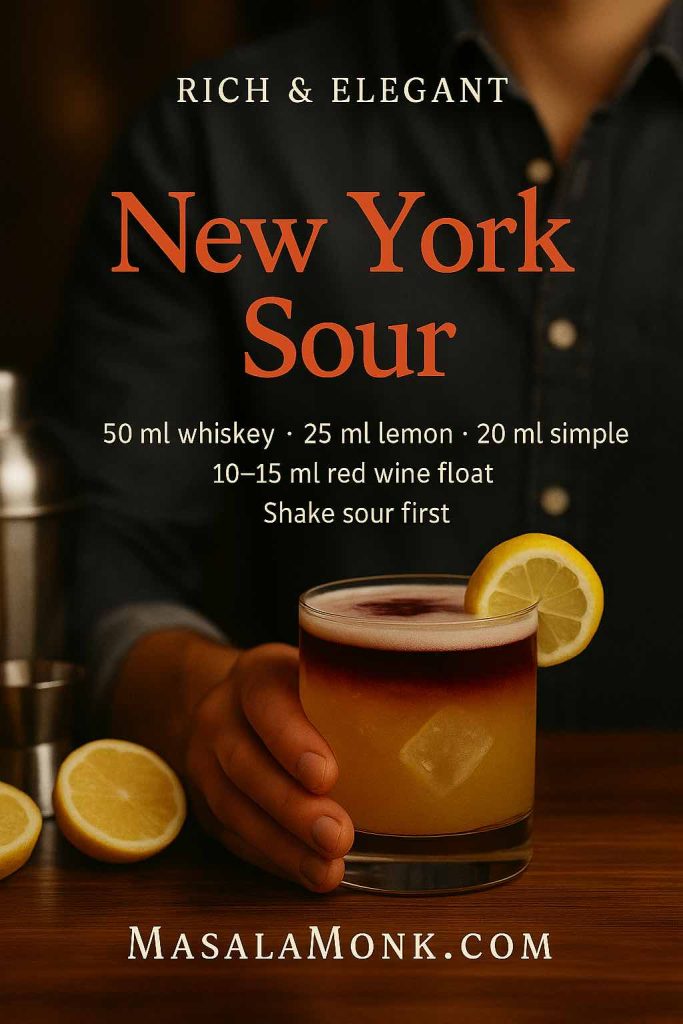
To make one:
- Shake your usual sour—either with or without egg white.
- Strain into a rocks glass over ice.
- Gently pour 10–15 ml (½ oz) of dry red wine over the back of a spoon so it floats on the surface.
The result is a layered drink with a deep purple cap and a fruity, winey aroma. It’s the answer to anyone looking for a New York sour drink or a more dramatic whiskey sour cocktail for dinner parties.
If you’d like a step-by-step benchmark, you can peek at Liquor.com’s New York Sour cocktail recipe, then tweak it to taste at home.
Maple, Nutmeg & Dessert-Like Sours
For colder evenings, swapping simple syrup for maple syrup gives you an instant maple whiskey sour. Add a dusting of nutmeg and perhaps a splash of bitters, and you’re in dessert territory.
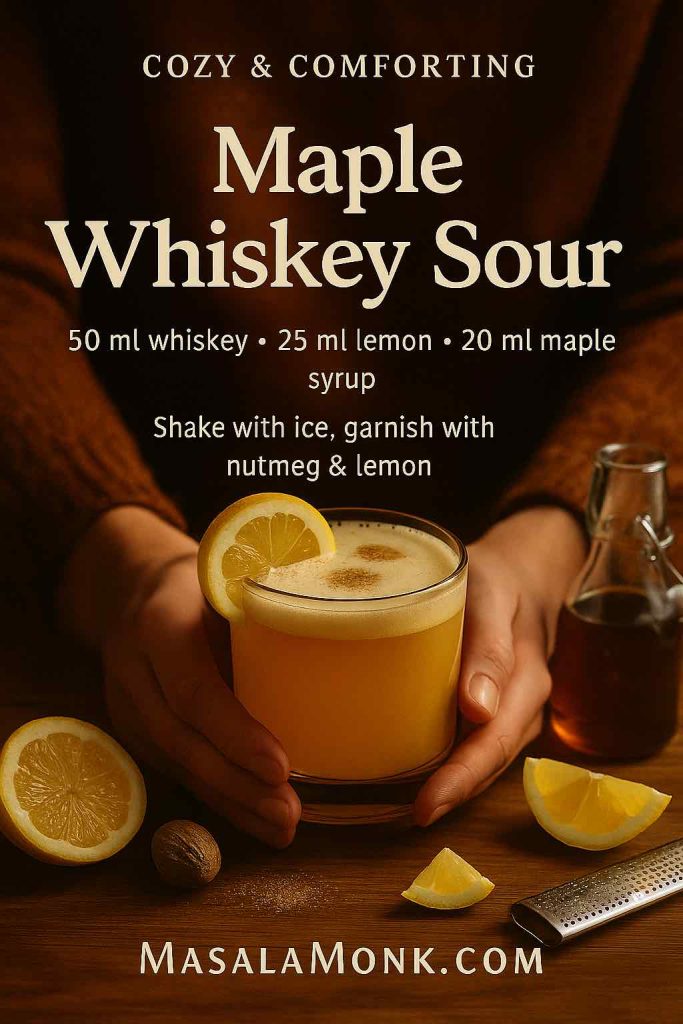
Masala Monk goes even further in their Nutmeg Maple Whiskey Sour, combining whiskey, maple, lemon, and nutmeg into a spiced, wintery twist. That’s a perfect example of how a basic whiskey sour recipe becomes something special with just one or two smart adjustments.
Amaretto & Whiskey Sours
If you enjoy nutty flavours, amaretto is your friend. A few ways to play:
- Amaretto whiskey sour – Split the base between whiskey and amaretto, then add lemon and a touch of syrup.
- Amaretto sour with whiskey – Start from an amaretto sour and add a shot of whiskey for depth.
- Amaretto bourbon sour or bourbon amaretto sour – Bourbon for richness, amaretto for almond sweetness.

You’ll find similar pairing ideas in Masala Monk’s piece on what mixes well with Baileys, where creamy liqueurs, nutty spirits, and whiskey frequently share the same glass. Once you see how well those flavours work together, folding amaretto into your whiskey sour feels very natural.
Fruity Whiskey Sours
Fruit-driven riffs are an easy way to soften the drink and make it more playful:
- Cranberry whiskey sour or cranberry orange whiskey sour
- Cranberry whiskey drink with lemon and a bit of sugar
- Apple whiskey sour, peach whiskey sour, or pineapple whiskey sour
- Cherry whiskey sour with muddled cherries plus juice
A simple approach is to replace part of the lemon or syrup with a fruit juice or puree, then rebalance to taste. If you already enjoy whiskey cranberry, cranberry and whiskey, or whiskey cranberry juice combos, you’re only a small step away from a full-blown whiskey sour variation.
Tropical-leaning recipes like Masala Monk’s coconut water cocktails show another path: lighter, longer drinks that keep whiskey as a base but weave in coconut, citrus, and sweetness. That approach also plays nicely with sour-style builds.
Tea & Spice Sours
Tea and spices open up a more sophisticated side of the sour template:
- Brewed black tea or Earl Grey can replace some of the water in your simple syrup or even stand in for part of the lemon.
- Spiced syrups (cinnamon, clove, star anise) can add warmth without overpowering.
For more inspiration, you can browse Masala Monk’s tea-driven cocktail collections, like their Earl Grey and bourbon iced tea cocktails or the saffron-infused iced tea recipes. Many of those drinks follow the same spirit–citrus–sweet blueprint as a sour, just stretched into a taller, more refreshing format.
Also Read: How to Make Churros (Authentic + Easy Recipe)
Glassware, Garnish, and Little Details
Although the whiskey sour cocktail feels relaxed and unfussy, a few small choices can change how it feels in the hand.
Glassware
Traditionally, a whiskey sour drink is served:
- In an old fashioned (rocks) glass over ice, or
- “Up” in a coupe or sour glass, without ice, especially when made with egg white
Serving on the rocks feels more casual and forgiving. Pouring it into stemware, on the other hand, makes it feel like a proper “cocktail-hour” moment, particularly when you’ve shaken in egg white and topped the foam with bitters.
Garnish
You don’t need a garnish for the drink to taste good, yet small touches do a lot:
- A lemon wheel or twist emphasises the citrus
- A cherry nods to old-school bar style
- A few drops of bitters on egg-white foam add aroma and visual flair
From there, you can get playful—an orange twist with a whiskey old fashioned sour spin, a cinnamon stick for a winter variation, or even a sprig of herb for a lighter whiskey and lemon cocktails vibe.
When to Reach for a Whiskey Sour
One of the reasons the whiskey sour cocktail endures is its flexibility. It works in a surprising number of scenarios:
- As an aperitif, when you want something bright but still spirit-forward
- As a slow sipper with snacks or fried foods (the lemon cuts through richness)
- As a bridge drink for people who don’t yet love neat whiskey but enjoy balanced cocktails
- As a base for dessert-leaning twists alongside coffee, chocolate, or creamy liqueurs
If you’re already dabbling in richer whiskey drinks, like cinnamon-spiked Old Fashioneds or dessert-style combinations from Masala Monk’s cinnamon cocktail round-up or their espresso martini variations, the sour gives you a fresher counterpoint—something that feels lighter on the palate without being lightweight.
Meanwhile, if you’re just getting into cocktails, the whiskey sour recipe is a perfect teacher. It shows you how to balance sweet and sour, how to adjust ratios to your taste, and how a small tweak (maple instead of sugar, or rye instead of bourbon) can create a whole new personality in the glass.
Also Read: How to Cook Bacon in the Oven (Crispy, No-Mess, Crowd-Ready Recipe)
Bringing It All Together
By now, the whiskey sour shouldn’t feel mysterious. It’s just:
- A spirit you like
- Fresh lemon juice
- Enough sweetness to balance
- Ice and a good shake
- Optional egg white if you love that silky foam
From that starting point, you can move in any direction you like. Pour in a red wine float and you’ve made a moody New York sour. Stir in maple syrup and nutmeg and suddenly you’re sipping a fireside treat. Reach for amaretto and you get a softer, dessert-like variation. Swap in cranberry juice, pineapple, or peach puree and you’re firmly in fruity-cocktail territory.
And if you ever feel stuck, you can always roam through the broader Masala Monk Cocktails recipe collection and see how often that simple sour logic—spirit, citrus, sweet—shows up in different clothes, from tea cocktails to shaken espresso drinks.

Ultimately, learning one reliable whiskey sour recipe does more than just give you a single drink. It hands you a template, a way of thinking about flavour and balance. Once you’ve felt that click—the moment when whiskey, lemon, and sugar line up just right—you’ll start to spot sour-shaped opportunities everywhere you look.
Also Read: 10 Best Chicken Sandwich Recipes (BBQ, Parm, Buffalo & More)
FAQs
1. What is the classic whiskey sour recipe?
The classic whiskey sour recipe follows a very simple pattern: 2 parts whiskey, 1 part fresh lemon juice, and 1 part sweetener. In practice, that usually means about 50 ml whiskey, 25 ml lemon juice, and 20–25 ml simple syrup shaken with ice and strained into a rocks glass. This basic build gives you a traditional whiskey sour that’s bright, balanced, and easy to tweak into your own version of the perfect whiskey sour.
2. What are the whiskey sour ingredients, with and without egg?
To start, the core whiskey sour ingredients are:
- Whiskey (bourbon, rye, Irish, or Scotch)
- Fresh lemon juice
- Simple syrup (or another sweetener)
That’s all you need for a simple whiskey sour. For a whiskey sour with egg white—often called a Boston Sour—you simply add a small amount of egg white and shake twice (once without ice, once with). When you prefer a whiskey sour without egg instead, you just leave that egg white out and still get a clean, refreshing drink. So “whiskey sour ingredients no egg” and “whiskey sour ingredients without egg” are exactly the same as the classic recipe minus the egg white.
3. How do you make a whiskey sour from scratch at home?
To make a whiskey sour from scratch, follow these steps:
- Measure 50 ml whiskey, 25 ml fresh lemon juice, and 20–25 ml simple syrup into a shaker with ice.
- Shake hard for 10–15 seconds until chilled.
- Strain into a rocks glass over fresh ice.
- Garnish with a lemon wheel or twist and a cherry.
That simple technique answers most of the common questions—how do you make a whiskey sour, how do you make a whiskey sour drink, how do I make a whisky sour, and even make a whiskey sour for a guest. If you want the silky foam version, you just add egg white and use a dry shake first to turn it into a whiskey sour and egg white style cocktail.
4. What’s the difference between whiskey sour with egg white and whiskey sour no egg?
To begin with, both versions use the same whiskey sour measurements and whiskey sour ratio of spirit, lemon, and sweetener. The only difference is texture. A whiskey sour with egg white (or egg white whisky sour) gets a thick, creamy foam and a rounder mouthfeel. A whiskey sour no egg feels lighter and more sharply citrusy. When you see phrases like whisky sour recipe with egg white or whiskey sour cocktail recipe egg white, that’s pointing to the rich, foamy style; meanwhile, whiskey sour recipe no egg, whisky sour recipe no egg, and whisky sour without egg are all describing the same bright, egg-free drink.
5. Can I make a whiskey sour with sour mix instead of fresh lemon?
Absolutely. For convenience, many people use whiskey sour mix or whiskey sour drink mix. To do that, simply mix about 50 ml whiskey with 75–90 ml sour mix, shake with ice, and strain. That gives you a quick whiskey sour with sour mix which is great for parties. When you’re using pre-bottled mixers, you’ll often hear it called whiskey and sour mix, sour mix and whiskey, or whisky sour with sour mix. If you prefer more control, you can prepare a homemade sour mix for whiskey sours with fresh lemon, lime, and sugar, which tastes brighter than most store-bought options and can become your own best whiskey sour mix or best sour mix for whiskey sour.
6. How do I make a whiskey sour with sweet and sour mix?
Instead of separate lemon and syrup, you can reach for sweet and sour mix with whiskey for a streamlined approach. All you need to do is combine around 1 part whiskey to 2 parts sweet and sour mix, shake with ice, and strain. This is often called a whiskey sour with sweet and sour mix, and informally people might just say whiskey and sweet and sour. Although fresh citrus and simple syrup give more nuance, this method is handy when you want to mix several drinks quickly and still stay within the classic cocktail whiskey sour recipe family.
7. What is the best whiskey for a whiskey sour?
When choosing the best whiskey for whiskey sour, think more about flavour than price. Generally, bourbon makes a round, approachable bourbon sour or bourbon whiskey sour with vanilla and caramel notes, while rye creates a spicier, drier whiskey sour drink. Irish whiskey yields a soft, friendly Irish whiskey sour, and Scotch gives you a more adventurous scotch sour or scotch and sour. As a rule of thumb, the best whiskey to use for a whiskey sour is something you enjoy neat but don’t mind mixing—your personal good whiskey for whiskey sour. For many drinkers, that becomes “their” best whiskey sour recipe and the bottle they return to whenever they want a reliable good whiskey sour.
8. How strong is a whiskey sour, and what ratio should I use?
In terms of strength, a standard whiskey sour recipe ml (50 ml whiskey, 25 ml lemon, 20–25 ml syrup) ends up around the same alcohol level as many classic cocktails once diluted with ice. The typical whiskey sour ratio is roughly 2:1:1 (two parts whiskey, one part citrus, one part sweet). You can tweak that if you like it more tart or more sweet, yet this simple ratio is widely used for a classic whiskey sour recipe and keeps the balance predictable. So whenever you see “original whiskey sour recipe” or “traditional whiskey sour,” this kind of proportion is usually what sits behind it.
9. Can I make a whiskey sour without simple syrup or with other sweeteners?
Certainly. While simple syrup is the most common choice, a whiskey sour without simple syrup is still possible. You can dissolve sugar directly into the lemon juice before shaking or use alternatives like honey syrup or maple syrup. For instance, a maple whiskey sour swaps simple syrup for maple, while a whiskey sour with maple syrup leans into a richer, dessert-like profile. Likewise, honey syrup produces a honey lemon whiskey sour that feels soothing and aromatic. As long as you keep the sweet-and-sour balance in line, the cocktail remains recognisably a whiskey sour cocktail even with different sweeteners.
10. Are canned or premade whiskey sours worth trying?
Many brands now offer whiskey sour in a can or bottle so you can simply chill, pour, and enjoy. These premade whiskey sour options are convenient for picnics, travel, or times when you don’t want to measure anything. Although they can’t always match the freshness of a whiskey sour from scratch, they’re a practical alternative when shaking isn’t possible. If you enjoy the flavour, you can later reverse-engineer it at home by adjusting your own whiskey sour recipe—changing the sweetness or citrus level until your homemade version becomes “the best whiskey sour recipe” for your taste.
11. Can I add extra flavours like grenadine, lime, or lemonade to a whiskey sour?
Yes, absolutely; once you understand the base, adding flavours becomes very natural. A whiskey sour with grenadine gets a rosy colour and extra pomegranate sweetness. A whiskey sour with lime adds sharper, more zesty acidity—either alongside lemon or in place of it. For a longer, more casual drink, a whiskey sour with lemonade stretches the cocktail into a refreshing highball. All these variations still sit in the same family as the original whiskey sour, just dressed up to suit your mood or the season.
12. How do I turn a good whiskey sour into my “perfect” whiskey sour?
Ultimately, the perfect whiskey sour is personal. Start with the classic whiskey sour recipe—50 ml whiskey, 25 ml lemon, 20–25 ml simple syrup—then adjust one element at a time. Perhaps you nudge the syrup down for a sharper edge, or increase lemon if you like a very bright whiskey and lemon drink. Maybe you switch from bourbon to rye, or you decide that a foamy whiskey sour with egg is your forever favourite. Gradually, you’ll find your preferred combination of whiskey, ratio, and texture, and that’s when your own traditional whiskey sour recipe quietly becomes “the best whiskey sour recipe” in your house.Thinking