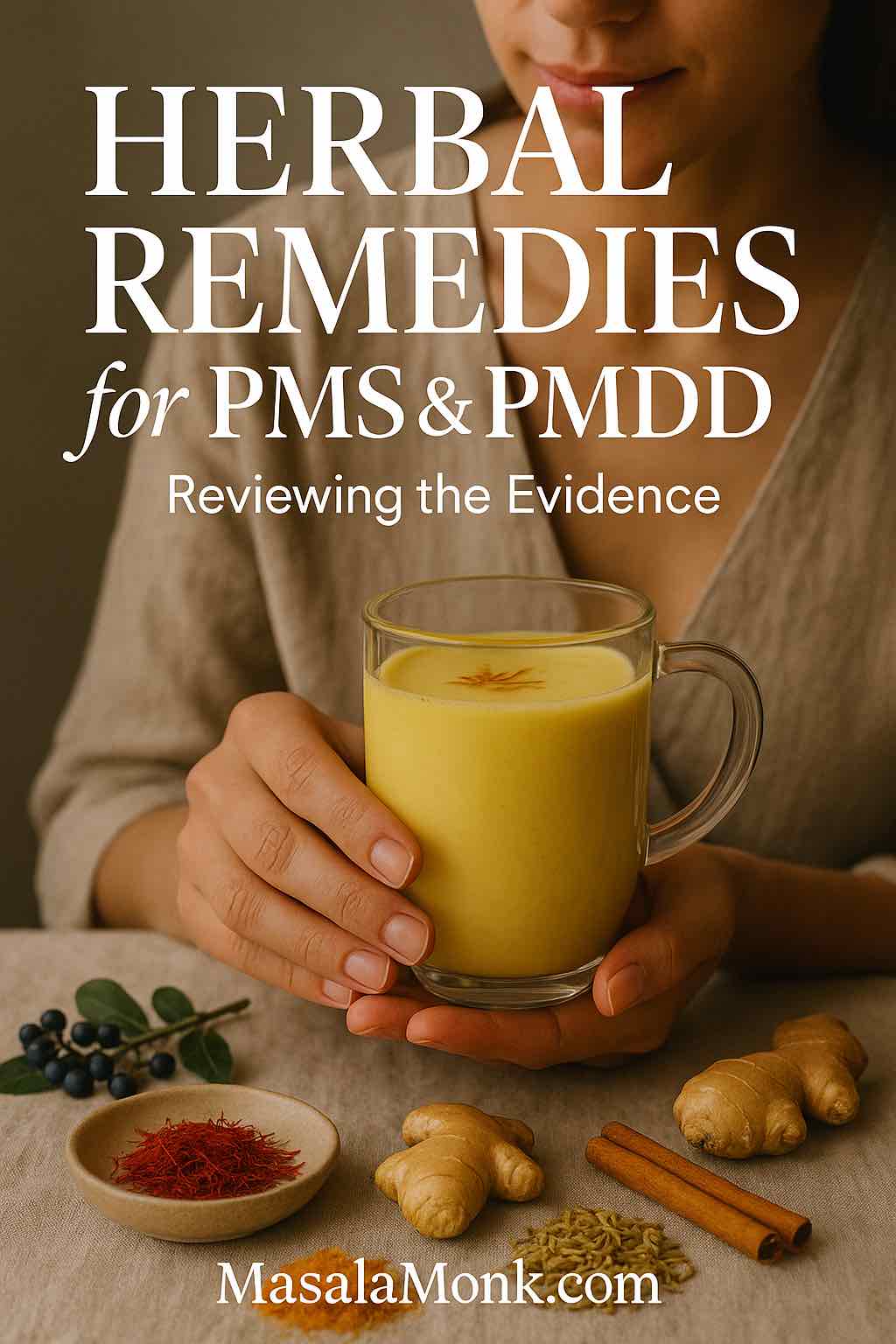
PMS and PMDD don’t just nudge mood; they can reshape sleep, appetite, focus, and even how social you feel. Although quick fixes rarely last, a small circle of botanicals and time-tested formulas actually show human data for relief. In this guide, we zero in on the best herbs for PMS—and where a few of them fit for PMDD—while staying practical about dosing, timelines, and safety. If symptoms are severe or disabling, fold any natural plan into clinician-guided care as outlined in the ACOG clinical guideline on premenstrual disorders.
Before you dive in: “natural” doesn’t equal “risk-free.” Most people do well with thoughtful choices and realistic timelines; however, pregnancy and lactation are special cases, and medication interactions matter. With that in mind, let’s begin with the best-supported options and then move into traditional remedies that may help in specific situations.
The best herbs for PMS: start where evidence is strongest
Chasteberry (Vitex agnus-castus) for PMS Relief
If you’re ranking the best herbs for PMS, chasteberry nearly always makes the podium. Randomized controlled trials and meta-analyses suggest standardized Vitex extracts ease global PMS—breast tenderness, irritability, headaches—when taken daily and evaluated over two to three cycles. For an accessible overview of uses, dosing, and cautions, skim the NCCIH chasteberry fact sheet. Because Vitex may interact with hormone-sensitive conditions and contraceptive regimens, it’s smart to touch base with your clinician before starting.
How people use it: standardized extract 20–40 mg once daily, usually in the morning; reassess after 2–3 cycles. For more granular safety and lactation details, the NIH pharmacology monographs (e.g., LactMed/monograph detail) are useful.
Everyday support while you trial Vitex: round out your routine with colorful food. Our practical primer—For Women: The Rainbow Diet for PMS Relief—maps satisfying plates to symptom patterns.
Saffron (Crocus sativus) in PMS and PMDD
When mood leads the picture—or PMDD features are prominent—saffron is compelling. In a double-blind randomized trial, saffron reduced PMS severity by cycles three to four; in another controlled study, it improved PMDD symptoms with good tolerability. Many protocols use 15 mg twice daily or 30 mg once daily, often focused on the luteal phase, with a fair evaluation after about two cycles. If you like reading primary sources, see the PMS RCT’s abstract at BJOG via PubMed and the PMDD trial available on PubMed Central.
How to bring it into daily life: capsules are convenient, but you can also integrate saffron in the kitchen. Start with a clear, friendly explainer—What is Saffron?—and then try a calming evening ritual like saffron-infused milk.
Ginger (Zingiber officinale) – one of the Best Herbs for PMS
If cramps hijack days one to three, ginger is one of the simplest, best-studied options. Systematic reviews and meta-analyses indicate that 750–2,000 mg/day of powdered ginger, taken during the first 3–4 days of bleeding, reduces dysmenorrhea pain—sometimes performing comparably to NSAIDs in head-to-head trials. For a readable overview, check the open-access meta-analysis on PubMed Central; for a more clinical snapshot, browse a recent PubMed abstract as well.
Practical ways to use it: capsules make adherence easy, but there’s nothing wrong with going culinary—strong ginger tea or a spiced smoothie can help. For a kitchen-first approach try Ginger & Herbal Teas: 5 Blends for Morning Sickness Relief.
Turmeric / Curcumin (Curcuma longa) as a PMS Relief Remedy
While not every trial agrees, the trend line for curcumin looks promising. A recent double-blind RCT reported improvements in both PMS scores and dysmenorrhea; several reviews echo a benefit signal, although heterogeneity exists. Because plain curcumin absorbs poorly, many study products include bioavailability enhancers—so labels matter. Typical research dosing lands around 500–1,000 mg/day, assessed after one to two cycles. You can read a 2025 RCT free in BMC Primary Care, then cross-check with a 2024 synthesis for broader context.
A simple habit to start: add a small, steady dose via food—pair turmeric with fat and a pinch of black pepper. Our Turmeric & Magnesium-Rich Smoothies show how to make this painless.
Cinnamon (Cinnamomum spp.) & Fennel (Foeniculum vulgare) in PMS
Two traditional antispasmodics deserve attention if cramps dominate. In randomized trials with students, cinnamon reduced pain, bleeding, and nausea over the first three days of menses; study dosing often looked like ~500–1,000 mg capsules, three times daily during days 1–3. You can read an open-access trial on menstrual bleeding and systemic symptoms on PubMed Central. Meanwhile, systematic reviews suggest fennel reduces primary dysmenorrhea pain compared with controls or NSAIDs, though study quality varies—see the clinical snapshot via PubMed and a broader 2020 review in Nutrients.
How to weave them in: for quick relief, mirror trial patterns during early menses; for gentler days, make a mild cinnamon-ginger tea with a pinch of fennel for sweetness. If you enjoy a heritage angle, our saffron series—culinary uses and a traditional medicine lens—connects kitchen rituals to modern evidence.
Also Read: The Benefits of Turmeric Ginger Cinnamon Tea for Weight Loss and Overall Well-being
Beyond the top tier: traditional botanicals worth a cautious look
Not every remedy earns a first-line spot; nonetheless, several traditional plants have small but intriguing human studies. Consider these as second-line experiments after you’ve tried the best herbs for PMS above.
Ginkgo (Ginkgo biloba)
Some randomized, placebo-controlled trials in students found reductions in PMS symptom scores with standardized ginkgo extracts (e.g., EGb 761 variants). Dosing across studies varies, but 40–120 mg twice daily for two cycles is a rough pattern to emulate. Because ginkgo may increase bleeding risk—particularly with anticoagulants or antiplatelets—review medications carefully. For a quick look at the trial evidence, browse the PubMed entry for a classic student-population RCT.
Chamomile (Matricaria chamomilla)
Used both as tea and in extract form, chamomile appears helpful for emotional symptoms of PMS in several small studies; some trials compare favorably to mefenamic acid for pain, though methods differ. If you appreciate a gentle, calming routine, a nightly chamomile tea during the luteal phase is low-effort and inexpensive. A broad review on PubMed Central pulls together the main threads if you’d like a deeper read.
Valerian (Valeriana officinalis)
Thanks to antispasmodic properties, valerian shows a reduction signal for primary dysmenorrhea across a mix of RCTs and meta-analyses. Protocols usually start at pain onset and continue through the first days of menses; capsule strengths differ widely, so follow product labels. Do note: heterogeneity is high, expectations should be moderate, and daytime drowsiness is possible.
Lavender (Lavandula angustifolia) — aromatherapy
Inhaled lavender oil isn’t an ingestible herb, yet it’s a traditional approach with supportive data for PMS-related anxiety and emotional tension. Randomized and crossover trials show small-to-moderate mood improvements when used during the luteal phase over ~three cycles. If you enjoy ritual, a short evening inhalation session pairs nicely with sleep hygiene.
Xiao Yao San / Jia-Wei Xiao Yao San (Traditional Chinese Medicine)
For readers drawn to formula-based traditions, Xiao Yao San (and its “augmented” variant, Jia-Wei Xiao Yao San) has a long history in patterns that include irritability, breast distension, and cycle irregularities. Reviews and meta-analyses suggest symptom relief in PMS/PMDD cohorts, but study quality and formula standardization vary considerably. If you explore this path, work with a qualified TCM practitioner and coordinate with your clinician. A helpful entry point is this overview in BMC Complementary Medicine and Therapies: effects and treatment methods of acupuncture and herbal medicine for PMS.
St. John’s wort (Hypericum perforatum) — not first-line
A few RCTs show a signal for physical/behavioral PMS symptoms; however, mood effects are inconsistent and the interaction profile is enormous (SSRIs/SNRIs, oral contraceptives, anticoagulants, transplant drugs, and more). Unless you’re under close medical supervision, prioritize other options. If you’re evaluating it academically, the PubMed overview is a fine starting place.
PMDD relief: where herbs genuinely fit—and where medicine leads
PMDD isn’t “PMS turned up to 11.” It can be disabling and is best approached as a multimodal condition. Botanicals with the most promise include saffron (best RCT signal) and chasteberry (adjunctive for global symptoms). Nevertheless, frontline treatments—such as SSRIs used continuously or intermittently, specific combined oral contraceptives, and psychotherapy—form the backbone of care. To anchor decisions in reputable guidance, revisit the ACOG premenstrual disorders guideline. While your clinician fine-tunes treatment, consider gentle daily supports—a cup of saffron-infused milk in the late evening, for instance—to ease transitions into sleep.
Using the best herbs for PMS wisely (so you can actually tell if they work)
Rather than starting five things at once, choose one or two that match your pattern:
- Global PMS with breast tenderness and irritability → chasteberry.
- Mood-dominant PMS or PMDD features → saffron first; Vitex second.
- Cramps and low-back ache on days 1–3 → ginger per menses; optionally layer cinnamon or fennel.
Then, commit to a fair trial: 2–3 cycles for chasteberry; about two cycles for saffron; per-menses dosing for ginger/cinnamon/fennel. Throughout, track symptoms briefly once a week (0–10 for pain; 0–10 for mood; 0–10 for energy/sleep; one line on function). After the trial window, decide—continue, adjust dose/timing, or pivot.
Meanwhile, cushion the plan with simple lifestyle anchors. A few minutes of movement on more days than not helps cramps and energy; our quick guide, Women’s Wellness: Exercise and PMS, shows how to ease in without overwhelm. On the plate, shoot for color and fiber; if you want a single, sustainable habit, start by adding one vividly colored veg and one omega-rich food per day, guided by the Rainbow Diet for PMS Relief.
Safety first (natural ≠ risk-free)
- Pregnancy & lactation: avoid herbs unless specifically cleared by your clinician.
- Bleeding tendency: take care combining higher-dose ginger, cinnamon, or fennel with anticoagulants or antiplatelets; pause around procedures when advised.
- Hormonal meds: discuss chasteberry if you use hormonal contraception; consider hormone-sensitive conditions. The NCCIH chasteberry overview is a practical primer.
- Interactions minefield: St. John’s wort can reduce the effectiveness of many medications, including oral contraceptives and antidepressants; it’s rarely a first choice.
- Product quality: pick standardized, single-herb products from reputable brands; avoid “mystery blends” with undisclosed amounts.
- Red flags: escalate care for disabling mood symptoms, thoughts of self-harm, sudden severe pelvic pain, fever, very heavy bleeding, or symptoms that feel “different from your normal.”
Best Ways to use these Herbs for PMS Relief
Consistency matters more than intensity. A realistic week might look like this:
- Morning: take chasteberry with breakfast; jot a two-second note on breast tenderness and irritability by evening.
- Luteal phase: add saffron (15 mg twice daily or 30 mg once daily). Create a simple nightly ritual—perhaps that warm cup of saffron-infused milk—to cue sleep and soften mood spikes.
- Days 1–3 (sometimes 4): use ginger capsules (or strong tea), and if cramps are stubborn, layer cinnamon or fennel for the first three days, mirroring study patterns. If you like checking sources, skim the cinnamon RCT and the fennel meta-analysis abstract.
- Anytime: reinforce with food-based anti-inflammatory choices. If you prefer sipping your support, the Turmeric & Magnesium-Rich Smoothies are an easy starting place.
What about other spice-drawer ideas?
Traditions also mention cloves, coriander, and cardamom for comfort. The clinical evidence is thinner, so position them as flavor and ritual, not primary therapy. If you’re spice-curious, here’s a gentle primer on cloves for menstrual pain relief and a broader look at women-centric herb lore in our saffron series; enjoy the heritage stories, but keep expectations modest until robust trials arrive.
When to pivot—and when to escalate
After a fair trial window, step back and reflect: did pain drop at least 30–50%? Is irritability less sharp? Are you sleeping more soundly? If results are only “meh,” either change the match (for example, swap from a Vitex-first approach to a saffron-led plan if mood is the main issue) or adjust dose/timing. For cramps, you might move from ginger alone to ginger plus cinnamon during days one to three. If PMDD features are clear—work impact, relationship strain, or safety concerns—prioritize medical care; herbs can still support edges of mood and energy, but the backbone of treatment shifts. Bookmark the ACOG guideline for that conversation.
FAQs
1) What are the best herbs for PMS?
The best herbs for PMS include chasteberry (Vitex) for overall symptom relief, saffron for mood and global scores, ginger for period cramps, turmeric/curcumin for PMS and dysmenorrhea, and—situationally—cinnamon and fennel for early-cycle pain. Start with one or two, then reassess after a fair trial.
2) How long before these remedies start working?
Chasteberry typically needs 2–3 cycles. Saffron often shows benefits after ~2 cycles. Ginger, cinnamon, and fennel are taken during days 1–3 (sometimes 4) of bleeding and work per-menses. Curcumin usually warrants 1–2 cycles.
3) Which herb helps most with mood swings and irritability?
Saffron is a strong first choice for mood-dominant PMS and PMDD features. Chasteberry can support overall mood changes as well, especially alongside lifestyle routines like sleep and movement.
4) What’s a sensible dosing plan to try first?
Begin with chasteberry 20–40 mg once daily for global PMS and add saffron 15 mg twice daily (or 30 mg once daily) in the luteal phase. For cramps, use ginger 750–2,000 mg/day during days 1–3. Evaluate before changing anything.
5) Are there fast, natural options for severe period pain?
Yes—ginger is the quickest botanical option and pairs well with heat and gentle movement. For stubborn cramps, layer cinnamon or fennel during the first three days of the cycle.
6) Do “best herbs for PMS” differ from herbs for PMDD?
Often, overlap exists. Saffron shows particularly helpful signals for PMDD mood symptoms, while chasteberry may assist overall. Nevertheless, PMDD commonly needs clinician-guided care (e.g., SSRIs or specific contraceptives) with herbs as adjuncts.
7) Can turmeric or curcumin actually help PMS?
Curcumin has emerging evidence for reducing PMS scores and cramp severity. Use enhanced-bioavailability forms around 500–1,000 mg/day and reassess after 1–2 cycles.
8) Is cinnamon good for more than flavor?
Yes. In multiple trials with students, cinnamon reduced pain, bleeding, and nausea during early menses. It’s best used on days 1–3, alongside ginger if needed.
9) What about fennel for cramps and bloating?
Fennel, a traditional antispasmodic, can ease primary dysmenorrhea and may feel soothing for gas and bloating. Dose per product; start at pain onset.
10) Do ginkgo, chamomile, valerian, or lavender help PMS?
They can, though evidence is smaller. Ginkgo has signals for overall PMS scores; chamomile may calm emotional symptoms; valerian can reduce cramp intensity; lavender aromatherapy supports tension and sleep in the luteal phase.
11) Are Chinese herbal formulas like Xiao Yao San useful?
They’re traditional mainstays with encouraging but variable study quality. If you choose this route, work with a qualified practitioner and keep your physician in the loop.
12) Which herbs are safest to combine?
Commonly combined, saffron + chasteberry (mood + global), or ginger + cinnamon/fennel (pain-focused). Introduce one change at a time, then layer a second after you’ve confirmed tolerance.
13) What should I avoid while testing herbs?
During pregnancy or lactation, skip botanicals unless cleared by a clinician. Be cautious with anticoagulants/antiplatelets when using higher-dose ginger, cinnamon, or fennel. Discuss chasteberry if you use hormonal contraception. Avoid mystery blends with undisclosed amounts.
14) What’s the best way to judge progress?
Track weekly scores (0–10) for pain, mood, energy, sleep, and daily function. After the trial window—2–3 cycles for chasteberry, ~2 for saffron, per-menses for ginger/cinnamon/fennel—continue only if you see meaningful improvement.
15) Can teenagers try natural remedies for PMS?
Yes—begin conservatively with food-first strategies (sleep, hydration, color-rich meals), then consider ginger for cramps. Herbs aimed at hormones (e.g., chasteberry) should be discussed with a clinician, especially in younger teens.
16) What helps most with PMS bloating?
Focus on gentle movement, steady hydration, and salt awareness. For botanicals, fennel may ease fullness; curcumin can support comfort via anti-inflammatory effects. Reassess after one to two cycles.
17) Are there “best herbs for PMS” if headaches or breast tenderness dominate?
Chasteberry is often preferred where breast soreness and cyclical headaches are part of the pattern. Pair with sleep hygiene and consistent meals to reduce triggers.
18) How do I choose a quality product?
Select standardized, single-herb extracts from reputable brands. Look for clear milligram amounts, batch testing, and straightforward ingredient lists. When in doubt, keep the formula simple.
19) What if nothing changes after a fair trial?
Switch strategy: mood-heavy cycles might move from chasteberry to saffron; pain-heavy cycles might add cinnamon or fennel to ginger. If PMDD features are evident or daily life is impaired, prioritize medical care and use botanicals as supportive additions.
20) Final take: what’s the smartest starting combo?
For most readers, the smartest entry is chasteberry for global symptoms plus ginger during days 1–3 for pain. If mood is the main issue, rotate saffron into the luteal phase. Keep it simple, stay consistent, and measure what matters.
External References – Best Herbs of PMS Relief
- Guideline overview: ACOG—Management of Premenstrual Disorders (2023).
- Vitex background and cautions: NCCIH: Chasteberry—Usefulness & Safety and NIH pharmacology notes via LactMed/monograph detail.
- Saffron evidence: PMS RCT at BJOG via PubMed and PMDD RCT on PubMed Central.
- Ginger for dysmenorrhea: open-access meta-analysis on PubMed Central; see also recent PubMed abstracts for updated syntheses.
- Curcumin for PMS/dysmenorrhea: 2025 double-blind RCT in BMC Primary Care with supportive 2024 reviews.
- Cinnamon and fennel for cramps: open-access cinnamon trial on PubMed Central and fennel meta-analysis via PubMed.
- Broader TCM perspective: BMC Complementary Medicine and Therapies overview on acupuncture and herbal medicine for PMS.
Internal reads
- Saffron education and everyday uses: What is Saffron? and soothing saffron-infused milk.
- Food-first support that complements the best herbs for pms: The Rainbow Diet for PMS Relief.
- Kitchen-friendly blends that pair with ginger/curcumin: Turmeric & Magnesium-Rich Smoothies.