Eczema affects millions worldwide, causing dry, itchy, inflamed skin that can be both physically uncomfortable and emotionally draining. While traditional treatments like corticosteroids and moisturizers are common, many people search for natural remedies—one of the most popular being apple cider vinegar (ACV).
If you’ve typed queries like “apple cider vinegar for eczema,” “does apple cider vinegar help eczema,” or “vinegar bath for eczema,” you’re probably curious whether ACV can actually help your skin condition. In this guide, we’ll dive deep into the facts, myths, benefits, risks, and how to use ACV safely.
What Is Eczema? A Quick Overview
Before exploring ACV’s potential role, it helps to understand eczema itself. Eczema, or atopic dermatitis, is a chronic skin disorder characterized by:
- Dry, cracked, and itchy skin
- Red or inflamed patches
- Blisters or oozing in severe cases
- A tendency to flare up due to triggers like allergens, stress, or irritants
There are several types of eczema, including:
- Atopic dermatitis (most common)
- Dyshidrotic eczema (small blisters on hands/feet)
- Stasis dermatitis (caused by poor circulation)
- Contact dermatitis (reaction to irritants/allergens)
Effective eczema treatment usually requires a combination of moisturizing, avoiding triggers, and sometimes medication.
Why Apple Cider Vinegar? What Makes It So Popular?
Apple cider vinegar has a long history in folk medicine, credited with antibacterial, antifungal, and anti-inflammatory properties. It’s made by fermenting apple juice, resulting in acetic acid, vitamins, and minerals.
People believe ACV can:
- Restore the skin’s natural acidic pH (normally around 4.5-5.5)
- Help fight bacteria like Staphylococcus aureus, which can worsen eczema
- Act as a mild exfoliant to remove dead skin cells
- Soothe itchiness and inflammation
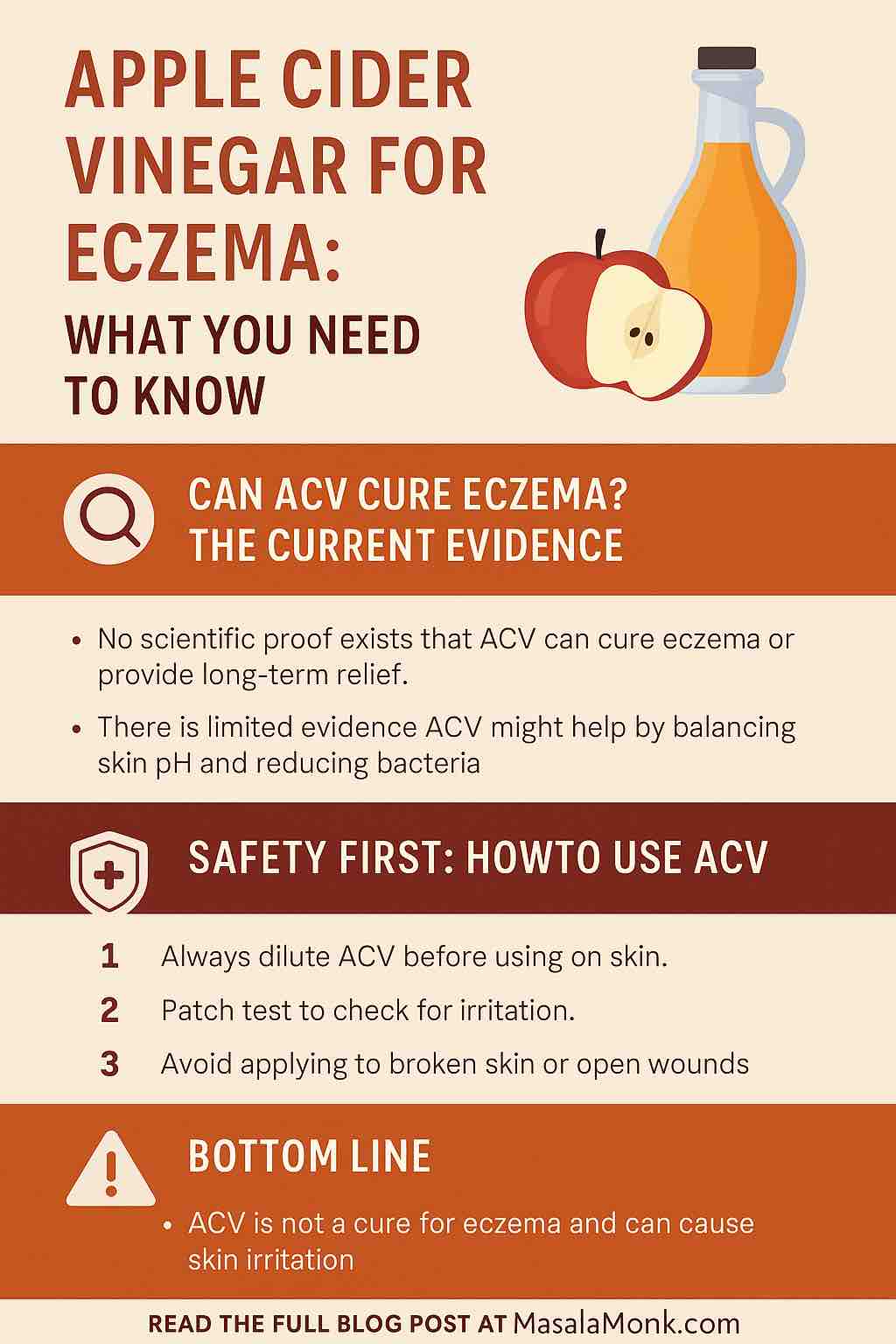
What Does the Science Say About Apple Cider Vinegar and Eczema?
The Good: Possible Benefits
- Skin pH and Barrier Restoration:
Eczema disrupts the skin’s acid mantle, raising the pH and weakening the barrier. ACV is acidic and may help restore the skin’s natural pH, potentially improving barrier function. A few small studies have shown temporary pH lowering effects after ACV application. - Antimicrobial Effects:
Some lab studies demonstrate ACV’s ability to inhibit the growth of bacteria and fungi, including Staphylococcus aureus, which commonly colonizes eczema lesions and triggers flare-ups.
The Caution: Limitations and Risks
- Lack of Robust Clinical Trials:
Unfortunately, rigorous human studies on ACV’s efficacy for eczema are scarce. Most evidence is anecdotal or from small pilot studies. - Skin Irritation and Burns:
ACV is acidic and can cause irritation, dryness, or chemical burns—especially when used undiluted or on broken skin. One study noted mild side effects like itching and discomfort in most participants using ACV topically.
How to Use Apple Cider Vinegar for Eczema: Best Practices
1. Dilution Is Key
Never apply undiluted ACV directly to your skin. A safe starting dilution is:
- 1 part ACV to 10 parts water for topical use
For example, mix 1 tablespoon of ACV into 10 tablespoons of water. This reduces acidity enough to minimize irritation.
2. Conduct a Patch Test
Before applying ACV broadly, test a small diluted patch on your forearm or behind your ear. Wait 24 hours to see if redness, itching, or burning develops.
3. Try Vinegar Baths
Adding ACV to bathwater is a gentle way to use it:
- Add 1-2 cups of ACV to a warm bath
- Soak for 10-15 minutes
- Pat skin dry afterward (avoid rubbing)
Vinegar baths may help reduce bacteria on the skin and soothe itchiness.
4. Avoid Broken or Cracked Skin
ACV should not be applied to open wounds, raw eczema patches, or severely inflamed areas to prevent pain and further irritation.
5. Frequency and Duration
Start with 1-2 applications per day or vinegar baths 2-3 times weekly. Adjust based on skin reaction.
ACV and Different Types of Eczema: What You Should Know
Dyshidrotic Eczema and ACV
For those with dyshidrotic eczema, the blisters can be particularly sensitive. Some people find diluted ACV helpful to dry blisters and reduce itching, but proceed carefully and consult your dermatologist.
Stasis Dermatitis and ACV
This type of eczema stems from circulation problems. ACV might help with bacterial control during flare-ups, but the underlying vascular issues require medical management.
What About Apple Cider Vinegar for Other Skin Rashes and Dermatitis?
Many people search for ACV remedies for skin rashes beyond eczema, including:
- Contact dermatitis
- Fungal infections
- Allergic reactions
While ACV’s antimicrobial and pH-balancing properties might provide mild relief, it’s not a substitute for proper diagnosis and treatment. Misuse can worsen rashes.
Expert Opinions: Should You Use Apple Cider Vinegar for Eczema?
Dermatologists generally recommend caution. While ACV might help some people, it is not a replacement for prescribed eczema therapies like moisturizers, corticosteroids, or immunomodulators.
If you want to try ACV:
- Consult your healthcare provider first
- Use it as a complementary approach, not standalone
- Discontinue if irritation worsens
Real User Experiences: What Are People Saying?
On forums and social media, opinions vary widely:
- Some swear by apple cider vinegar baths and diluted topical application for calming flare-ups
- Others report worsening irritation or burning sensations
- Most agree that dilution and cautious use are crucial
Summary: Is Apple Cider Vinegar Good for Eczema?
- Can ACV cure eczema? No, not based on current evidence.
- Can ACV help eczema symptoms? Possibly, through pH balancing and antimicrobial effects.
- Is ACV safe for eczema? It can be safe if properly diluted and used carefully.
- What’s the bottom line? ACV can be a useful home remedy for some, but not a cure-all. Always prioritize your dermatologist’s guidance.
How to Get Started Safely with Apple Cider Vinegar for Eczema
- Purchase organic, unfiltered apple cider vinegar with “the mother.”
- Dilute properly before every use.
- Patch test and watch for adverse reactions.
- Consider vinegar baths rather than direct application if you have sensitive skin.
- Use alongside your existing eczema treatments, not as a replacement.
Frequently Asked Questions (FAQs)
1. Can apple cider vinegar cure eczema?
No, apple cider vinegar cannot cure eczema. While it may help soothe symptoms by balancing skin pH and reducing bacteria, eczema is a chronic condition that requires ongoing management with prescribed treatments.
2. How should I dilute apple cider vinegar before applying it to eczema-affected skin?
A safe dilution ratio is 1 part apple cider vinegar to 10 parts water. For example, mix 1 tablespoon of ACV with 10 tablespoons of water to minimize irritation risks.
3. Is it safe to use undiluted apple cider vinegar on eczema?
No, applying undiluted ACV can cause skin burns, irritation, and worsen eczema symptoms, especially on broken or sensitive skin.
4. How often can I use apple cider vinegar for eczema?
Start with once daily or a few times a week, such as vinegar baths 2-3 times weekly. Monitor your skin closely and adjust frequency depending on how your skin reacts.
5. Can apple cider vinegar be used on all types of eczema?
While it may provide mild relief for some types like atopic or dyshidrotic eczema, ACV is not a one-size-fits-all treatment. Stasis dermatitis and severe eczema may require specialized medical care.
6. What is the best way to use apple cider vinegar for eczema—topical application or bath?
Both can be effective, but vinegar baths (1-2 cups ACV in a warm bath) tend to be gentler on sensitive skin compared to direct topical application.
7. Are there any side effects of using apple cider vinegar on eczema?
Possible side effects include itching, redness, burning sensation, and skin dryness. Discontinue use immediately if these occur and consult a healthcare professional.
8. Can apple cider vinegar help with skin rashes other than eczema?
ACV’s antimicrobial and pH-balancing properties may help some mild rashes, but it’s important to identify the rash cause and seek appropriate treatment.
9. Should children with eczema use apple cider vinegar?
It’s generally not recommended to use ACV on babies or young children without medical advice due to their sensitive skin.
10. Can I combine apple cider vinegar with my prescribed eczema treatments?
Consult your dermatologist first. ACV may be used as a complementary remedy but should not replace prescribed medications or moisturizers.
Share Your Experience!
Have you tried apple cider vinegar for eczema or skin rashes? What worked or didn’t work for you? Drop a comment below and join the conversation!











