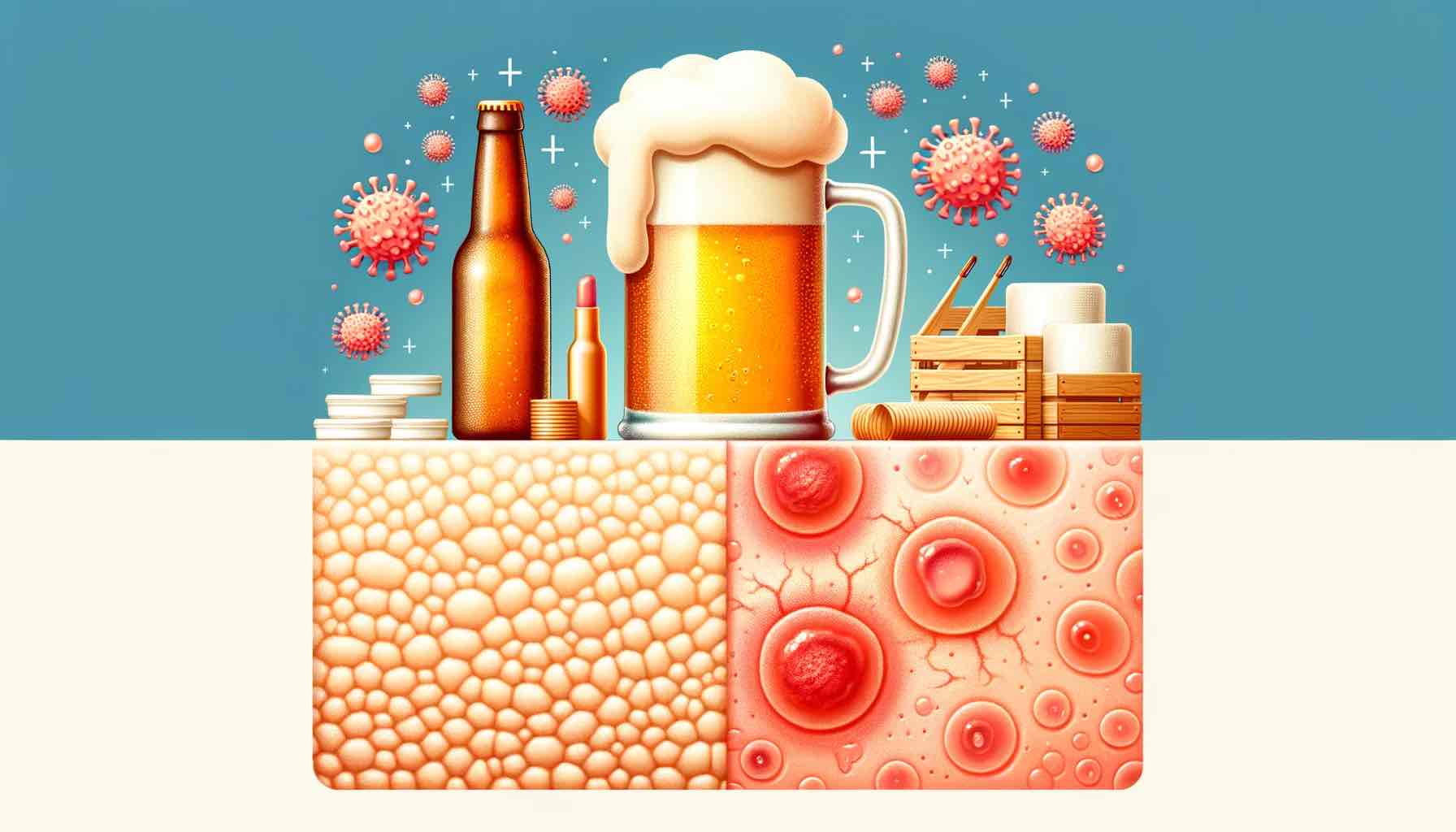
Dermatitis is an umbrella term used to describe various conditions that cause inflammation of the skin. Among the most common forms are eczema, contact dermatitis, and seborrheic dermatitis. These conditions, though diverse in their symptoms and triggers, share the common hallmark of inflamed, often itchy and irritated skin. The journey of understanding dermatitis begins with a closer inspection of its most prevalent forms—eczema and psoriasis.
Eczema and Psoriasis: A Closer Look at Causes
Genetic Predisposition:
Both eczema and psoriasis have a genetic component that predisposes individuals to these conditions. Genes play a pivotal role in how our bodies respond to external irritants and internal triggers. In the case of eczema and psoriasis, certain genetic markers can make individuals more susceptible to the environmental factors that trigger these conditions.
- Gene Mutations: Mutations in specific genes can affect the skin’s barrier function or the immune system response, laying the groundwork for eczema or psoriasis.
- Family History: A family history of eczema, psoriasis, or other autoimmune diseases significantly increases the likelihood of an individual developing these conditions.
Immune System Response:
An overactive or misdirected immune system is often at the heart of both eczema and psoriasis. The immune system, designed to protect the body from harmful invaders like bacteria and viruses, sometimes reacts to harmless substances or even the body’s own cells, causing inflammation.
- Inflammatory Cytokines: In individuals with eczema or psoriasis, certain immune cells release inflammatory cytokines, substances that promote inflammation, causing the characteristic skin symptoms of these conditions.
- Autoimmunity: In psoriasis, the immune system attacks healthy skin cells, accelerating skin cell turnover and causing the thick, scaly patches characteristic of this condition.
Environmental Triggers:
The environment plays a crucial role in triggering the symptoms of eczema and psoriasis. Everything from allergens to irritants and infections can initiate or exacerbate the inflammatory skin responses seen in these conditions.
- Allergens: Common allergens like pollen, pet dander, and mold can trigger eczema flare-ups.
- Irritants: Substances like detergents, soaps, and certain fabrics can irritate the skin and trigger both eczema and psoriasis.
- Infections: Infections, particularly streptococcal infections, can trigger psoriasis flare-ups, while certain viral and bacterial infections can exacerbate eczema.
The complex interplay between genetics, the immune system, and environmental triggers orchestrates the onset and course of eczema and psoriasis. Understanding these dynamics is crucial in developing effective management strategies for these often persistent skin conditions.
Sudden Onset Eczema in Adults
As dermatological mysteries go, the sudden appearance of eczema in adulthood can be a perplexing scenario. Unlike its more common counterpart that manifests in childhood, adult-onset eczema often catches individuals off guard. Here’s a closer look into this sudden unwelcome guest.
The Unseen Trigger
Adult-onset eczema, often known as atopic dermatitis, doesn’t play by the general rules. While eczema is often associated with childhood, adults are not immune to this skin condition. The peak occurrence for adult-onset eczema often appears in the 50s, although it can emerge at any age.
- Stress: Adult life comes with its fair share of stress, and for some, the skin reacts by developing eczema.
- Harsh Soaps and Detergents: The skin’s battle with harsh chemicals often leads to dermatological discontent, paving the way for eczema.
Identifying Triggers
Just as with childhood eczema, the adult version also has its list of triggers. Identifying and avoiding these triggers can be a significant step toward managing the condition.
- Extreme Temperatures: Both hot and cold extremes can trigger eczema flare-ups.
- Allergens: Pollen, pet dander, and other common allergens can be culprits behind a sudden eczema flare.
A Life-Altering Appearance
The sudden appearance of eczema can significantly impact an adult’s life. From the incessant itch to the visible red patches, eczema can be both a physical and emotional burden.
- Quality of Life: The incessant itch and irritation can disrupt sleep, focus, and overall quality of life.
- Social Impact: Visible eczema can also have a social impact, affecting self-esteem and social interactions.
The sudden onset of eczema in adults is a stark reminder that skin health is a lifelong endeavor. Understanding the triggers and seeking timely treatment can significantly ease the journey through adult-onset eczema.
Contact Dermatitis: Unwanted Contact
Contact dermatitis is a reactive condition of the skin manifesting as a result of direct contact with certain substances. It’s as if the skin throws a mini revolt against certain materials or substances it finds irksome. The skin’s reaction can range from mild irritation to a more severe allergic response. Let’s break down the uninvited contact further:
Types of Contact Dermatitis:
Contact dermatitis chiefly categorizes into two types based on the nature of the reaction.
- Irritant Contact Dermatitis: When something irritates the skin, like a harsh soap, detergent, or certain chemicals, irritant contact dermatitis occurs. It’s the skin’s way of saying, “I don’t like this one bit.”
- Allergic Contact Dermatitis: This occurs when the skin decides to launch an allergic reaction to a substance, like nickel or poison ivy. It’s not just a matter of dislike; it’s an outright rejection.
Red Flags: Symptoms to Watch Out For
The skin doesn’t keep its discontent to itself; it shows visible signs of distress.
- Redness and Irritation: The most common signs of contact dermatitis include redness, irritation, and itching.
- Blisters: In more severe reactions, blisters filled with clear fluid can develop, providing a clear signal that the skin is not in a happy place.
Does It Spread?
A common myth about contact dermatitis is that it’s contagious or that it can spread to other areas of the body. However, contact dermatitis doesn’t spread to other people or other parts of the body unless those areas also come into contact with the irritant or allergen.
- Contained Reaction: The reaction remains contained to the area of contact, a clear indication of the skin’s boundary of discontent.
Avoidance is Key
The best strategy to deal with contact dermatitis is to identify and avoid the irritants or allergens causing the reaction.
- Patch Testing: Allergy testing can help identify the substances that trigger allergic contact dermatitis, aiding in the avoidance strategy.
- Gentle Skin Care: Using gentle soaps and moisturizers can help prevent irritant contact dermatitis.
Contact dermatitis reminds us of the skin’s sensitive nature and its readiness to protect itself against perceived threats. By understanding the triggers and symptoms of contact dermatitis, individuals can take steps to avoid these unwanted skin reactions and maintain a peaceful rapport with their skin.
Eczema on the Neck: An Itchy Predicament
The neck, a highly visible and sensitive area, can unfortunately be a common site for eczema flare-ups. The itchiness, redness, and irritation characteristic of eczema can be particularly bothersome when it decides to settle in the neck region. Let’s delve into the causes and impact of this localized nuisance.
The Itchy Instigators
Eczema on the neck may not always have a clear-cut cause, but there are certain common instigators.
- Allergens: Allergic reactions to substances such as nickel in jewelry, certain fabrics, or even some skincare products can trigger eczema flare-ups on the neck.
- Irritants: The skin on the neck might react adversely to harsh soaps, detergents, or even the fabric of a scarf or collar.
Stress and Weather Woes
Certain non-tangible factors also play a significant role in triggering or exacerbating eczema on the neck.
- Stress: High-stress levels can worsen eczema symptoms. The neck, being a common tension-holding area, might exhibit eczema flare-ups during stressful times.
- Weather Changes: Cold, dry weather can make the skin on the neck dry and itchy, leading to eczema flare-ups.
Management and Mitigation
Managing eczema on the neck involves a blend of lifestyle modifications and topical treatments.
- Moisturizing: Regular moisturizing with a gentle, hypoallergenic moisturizer can help keep the skin on the neck soft and less prone to irritation.
- Avoidance of Irritants: Identifying and avoiding irritants, whether they be certain fabrics or skincare products, can significantly help in managing eczema on the neck.
Seeking Professional Help
Persistent or severe eczema on the neck warrants a visit to a dermatologist who can prescribe topical treatments or other interventions to manage the condition effectively.
- Topical Treatments: Topical steroids or calcineurin inhibitors can be effective in reducing inflammation and itchiness associated with eczema on the neck.
Eczema on the neck can be a highly visible and bothersome condition. Understanding the triggers and employing effective management strategies can significantly help in alleviating the symptoms and improving the quality of life for individuals dealing with this itchy predicament.
Unraveling Seborrheic Dermatitis on the Scalp
Seborrheic Dermatitis, a common skin condition, often chooses the scalp as its playground. It’s known for causing dandruff, but it can also lead to redness, scaly patches, and irritation. Let’s delve into what triggers this condition and the symptoms that herald its presence on the scalp.
Underlying Causes:
Seborrheic Dermatitis is often a result of a combination of factors rather than a single cause.
- Yeast Overgrowth: A type of yeast found on the skin, Malassezia, is often implicated in seborrheic dermatitis. When this yeast grows too much, it can irritate the skin and cause extra skin cells to grow.
- Medical Conditions: Individuals with certain medical conditions like Parkinson’s disease, HIV, or those recovering from stressful medical conditions might experience seborrheic dermatitis.
- Seborrhea: People with oily skin or hair are more prone to developing seborrheic dermatitis.
Manifesting Symptoms:
Seborrheic dermatitis makes its presence known through a range of symptoms.
- Flaky Scalp: The most common symptom is dandruff, where white or yellow flakes of skin appear on the scalp and in the hair.
- Red to Purple Skin Tone: The affected skin may become red, and in some individuals, it may take on a purplish hue.
- Greasy Patches: Sometimes, the skin can develop oily, greasy patches covered with white or yellow scales.
Hair Loss Connection:
While seborrheic dermatitis itself doesn’t cause hair loss, the itching and scratching if severe, can lead to hair loss.
- Follicle Damage: Excessive scratching can damage hair follicles, leading to temporary hair loss.
Seeking Relief:
Managing seborrheic dermatitis involves a combination of good skincare practices and medical treatments.
- Shampoos: Medicated shampoos containing ingredients like ketoconazole, selenium sulfide, or pyrithione zinc can be effective.
- Topical Treatments: Topical antifungals and steroids can help control inflammation and yeast overgrowth on the scalp.
Seborrheic dermatitis on the scalp can be an irritating and sometimes embarrassing condition. However, with the right treatment and management strategies, individuals can effectively control symptoms and prevent flare-ups, paving the way to a clearer, more comfortable scalp.
Lichenoid Dermatitis: A Pathologic Puzzle
Lichenoid Dermatitis is a skin condition that often mirrors the symptoms of other dermatological ailments, adding a layer of complexity to its diagnosis and understanding. It presents itself as small, itchy, and often painful bumps on the skin, resembling lichen on rocks. Delving deeper into this condition unveils a pathologic outline that is distinct yet intricate.
Pathologic Outlines:
The pathology of Lichenoid Dermatitis is a narrative told through microscopic examination.
- Cellular Infiltration: The hallmark of lichenoid dermatitis is a band-like infiltration of inflammatory cells at the junction of the epidermis and dermis, a crucial clue for pathologists.
- Epidermal Changes: Accompanying cellular changes in the epidermis include vacuolar alteration of basal keratinocytes and often, the presence of Civatte bodies.
Triggering Factors:
Lichenoid Dermatitis can be triggered by a variety of factors, making its management a tad challenging.
- Drugs and Medications: Certain medications can trigger lichenoid reactions, necessitating a thorough review of an individual’s medication list when diagnosing this condition.
- Infections: Hepatitis C infection has been associated with lichenoid dermatitis, highlighting the interplay between systemic infections and skin reactions.
Diagnostic Journey:
The diagnostic odyssey for Lichenoid Dermatitis often involves a close collaboration between clinicians and pathologists.
- Skin Biopsy: A skin biopsy followed by a microscopic examination is often the gold standard for diagnosing Lichenoid Dermatitis.
- Clinical Correlation: A thorough clinical examination and history-taking are crucial for correlating the pathological findings with the clinical picture.
Treatment and Management:
Management of Lichenoid Dermatitis focuses on addressing the underlying triggers and providing symptomatic relief.
- Topical Steroids: Topical corticosteroids remain a mainstay of treatment for alleviating inflammation and itchiness.
- Systemic Therapy: In severe or extensive cases, systemic therapy such as oral steroids or immunosuppressive agents may be considered.
Lichenoid Dermatitis is a dermatological enigma with a unique pathological outline. Its understanding requires a fine balance between clinical acumen and pathological insights. Addressing the underlying triggers and employing a structured treatment plan can significantly improve the quality of life for individuals grappling with this skin condition.
Eczema in the Groin: A Delicate Dilemma
The groin, a sensitive and often concealed area, can unfortunately be a target for eczema, making it a particularly uncomfortable experience. This condition, known for its relentless itch and irritation, when localized in the groin, can affect daily activities and personal comfort significantly. Here’s a closer look into this delicate dilemma.
The Inflammatory Intruder
Eczema in the groin is often a result of an overactive immune system responding to various triggers.
- Allergens and Irritants: Substances like soaps, detergents, or even the fabric of underwear can trigger eczema in the groin area.
- Sweat and Moisture: The groin being a warm, moist area is conducive for irritation, which can precipitate an eczema flare-up.
Characteristic Symptoms
The symptoms of eczema in the groin are characteristic yet can cause a great deal of discomfort.
- Itchiness: The relentless itch is often the most bothersome symptom.
- Redness and Inflammation: The affected area may become red, swollen, and irritated.
- Dry, Scaly Skin: Over time, the skin may become dry and scaly.
An Autoimmune Association?
There’s a broader dialogue in the medical community about eczema’s connection to the autoimmune spectrum.
- Immune Response: The immune system’s exaggerated response to triggers is a hallmark of both eczema and autoimmune conditions.
Managing the Uncomfortable
Effective management of eczema in the groin requires a blend of self-care measures and medical treatment.
- Gentle Skincare: Using hypoallergenic soaps and moisturizers can help keep irritation at bay.
- Topical Treatments: Topical steroids or calcineurin inhibitors can be effective in managing symptoms.
- Clothing Choices: Wearing loose, breathable clothing can help minimize irritation in the groin area.
Seeking Medical Guidance
A dermatologist can provide personalized advice and treatment plans to manage eczema in the groin effectively.
- Diagnosis and Treatment: Accurate diagnosis is crucial for effective treatment, which may include topical medications or even phototherapy in severe cases.
Eczema in the groin is a delicate issue that requires a gentle and informed approach for effective management. Understanding the triggers and working closely with healthcare providers can pave the way towards alleviating the discomfort and improving the quality of life.
Varicose Veins and Eczema: A Vein Attempt at Comfort
Varicose veins, those bulging and twisted veins often visible under the skin, can sometimes be accompanied by a type of eczema known as varicose eczema or stasis dermatitis. This condition manifests around the area of the varicose veins and can be a source of itchiness and discomfort. Let’s explore the intertwined relationship between varicose veins and eczema.
The Underlying Connection
Varicose veins and eczema often co-exist due to a common underlying issue of poor circulation.
- Venous Insufficiency: Varicose veins are often a result of venous insufficiency where blood doesn’t flow back efficiently to the heart. This can lead to pooling of blood and increased pressure in the veins, which can irritate the skin and trigger varicose eczema.
Symptoms Unveiled
Varicose eczema presents with symptoms that can significantly affect an individual’s comfort and quality of life.
- Itchy Skin: One of the hallmark symptoms of varicose eczema is itchiness around the area of the varicose veins.
- Discoloration and Scaling: The affected skin may become discolored, often taking on a brownish hue, and may also become dry and scaly.
White Spots: A Sign of Chronicity
In chronic cases of varicose eczema, white spots may appear on the skin due to loss of pigmentation, a sign of long-term skin changes associated with this condition.
- Chronic Changes: The white spots are indicative of the chronic nature of the skin inflammation associated with varicose eczema.
Managing Varicose Eczema
Management aims at improving circulation and providing relief from the symptoms of eczema.
- Compression Therapy: Wearing compression stockings can help improve circulation, which in turn can alleviate the symptoms of varicose eczema.
- Topical Treatments: Topical steroids can help control the itchiness and inflammation associated with varicose eczema.
Preventing Flare-ups
Preventive measures can go a long way in managing varicose eczema and improving the quality of life.
- Regular Movement: Regular exercise and movement can help improve circulation and prevent the worsening of varicose veins and eczema.
- Skincare: Gentle skincare and regular moisturizing can help keep the skin in good condition and prevent flare-ups of eczema.
Varicose eczema is a condition intertwined with varicose veins, each aggravating the other. A comprehensive approach targeting both the venous insufficiency and the skin inflammation can provide relief and improve the quality of life for individuals dealing with this vein attempt at comfort.
Psoriasis and Eczema: Unveiling the Underlying Causes
Psoriasis and eczema are two prevalent skin conditions that can cause significant discomfort and self-consciousness. While they share similarities like red, itchy skin, their underlying causes and treatment approaches differ. Let’s delve into the root causes of these skin ailments and how they manifest differently.
The Root Causes
Understanding the underlying mechanisms is crucial for effective management and treatment.
- Autoimmune Assault (Psoriasis): Psoriasis is often linked to an overactive immune system where the body mistakenly attacks healthy skin cells, accelerating skin cell turnover.
- Irritant Invasion (Eczema): Eczema, on the other hand, is often triggered by external irritants or allergens, leading to an inflammatory response in the skin.
Genetic Predisposition
Both conditions have a genetic component, making individuals more susceptible to developing either psoriasis or eczema based on their family history.
- Genetic Links: Certain genes have been associated with an increased risk of either psoriasis or eczema.
External Triggers
Both psoriasis and eczema can be exacerbated by external factors, although the specific triggers may vary.
- Stress: Stress is a common trigger for both psoriasis and eczema flare-ups.
- Environmental Allergens (Eczema): Common allergens like pollen, dust mites, or pet dander can trigger eczema.
- Skin Injury (Psoriasis): Injury to the skin, such as a cut or scrape, can trigger a psoriasis flare, known as the Koebner phenomenon.
Spotting the Differences
While they may seem similar, psoriasis and eczema have distinguishing features.
- Appearance: Psoriasis often appears as well-defined, thick, red patches with silvery scales. Eczema, on the other hand, tends to be dry, red to brownish-gray patches with possible oozing or crusting.
- Location: Psoriasis commonly affects the elbows, knees, and scalp, while eczema frequently occurs on the hands, inner elbows, and behind the knees.
The Path to Relief
Managing psoriasis and eczema requires a tailored approach based on the individual’s symptoms, triggers, and the severity of the condition.
- Topical Treatments: Topical corticosteroids are a mainstay in managing both conditions. Other topical treatments include calcineurin inhibitors and PDE4 inhibitors for eczema, and topical retinoids for psoriasis.
- Systemic Treatments: Severe cases may require systemic treatments like biologic drugs, which target specific parts of the immune system.
Psoriasis and eczema, though often confused, have distinct underlying causes and manifestations. Unveiling these differences is key to a targeted and effective treatment plan, paving the way to clearer, more comfortable skin.
Contact Dermatitis: When Skin Meets Irritation
Contact dermatitis is a reactionary tale of the skin, unfolding when it encounters irritants or allergens. The narrative includes redness, itching, and sometimes blisters, making it a rather uncomfortable experience. Delving into the types, triggers, and treatment can provide a roadmap to better skin comfort.
Types of Contact Dermatitis
Understanding the type of contact dermatitis is essential for managing the condition effectively.
- Irritant Contact Dermatitis: This occurs when the skin is exposed to irritating substances like detergents or harsh soaps.
- Allergic Contact Dermatitis: This is a result of the skin’s allergic reaction to substances like nickel, fragrances, or poison ivy.
Blisters and Beyond
Contact dermatitis can progress to form blisters, which can be both painful and itchy.
- Blistery Battleground: The blisters can burst, ooze, and eventually crust over, entering a new stage of healing or further irritation.
Spread or Not?
A common question is whether contact dermatitis can spread. The answer lies in understanding the nature of the reaction.
- Non-Contagious Condition: Contact dermatitis doesn’t spread to other people or other parts of your body unless you come into contact with the irritant or allergen again.
Diagnostic Path
Diagnosis is a path often paved with detailed history taking and skin testing.
- Patch Testing: This is a common method to identify specific allergens causing allergic contact dermatitis.
- Skin Examination: A thorough examination of the skin and a review of your exposure to potential irritants or allergens are key steps in diagnosing contact dermatitis.
Treatment Terrain
The treatment terrain for contact dermatitis is aimed at relieving symptoms and avoiding triggers.
- Topical Creams: Topical steroids are often prescribed to manage inflammation and itching.
- Avoidance: Identifying and avoiding the irritants or allergens causing contact dermatitis is crucial for long-term management.
Contact dermatitis, a common skin ailment, is a tale of irritation and inflammation. With the right diagnostic approach and treatment plan, it’s a tale that can have a soothing ending, leading to healthier, more comfortable skin.
We have covered a variety of dermatological conditions such as psoriasis, eczema, contact dermatitis, seborrheic dermatitis, lichenoid dermatitis, varicose eczema, and scalp eczema, each in its own dedicated section. These sections have explored the causes, symptoms, diagnosis, and treatment options for each condition.
Now, as we draw this comprehensive exploration to a close, it’s essential to emphasize the importance of professional medical advice and personalized treatment plans in managing these skin conditions. Whether it’s identifying triggers, selecting the right skincare products, or adhering to medical treatments, a collaborative approach between individuals and healthcare providers is crucial.
Conclusion: Navigating the Skin’s Narrative
Our skin, the largest organ, has a language of its own. It communicates through various signs, symptoms, and conditions, each telling a unique story. Conditions like psoriasis, eczema, and various forms of dermatitis narrate tales of immune responses, external irritations, and internal imbalances. Understanding these narratives, identifying the triggers, and seeking professional medical guidance are pivotal steps towards better skin health.
Each skin condition, be it a common occurrence like eczema or a more complex scenario like lichenoid dermatitis, offers an opportunity to delve deeper into understanding our body’s responses and the external factors influencing them. The path to managing these conditions lies in a blend of self-awareness, medical insight, and a tailored treatment plan.
As we conclude this expedition into the world of dermatological conditions, it’s an invitation to continue exploring, learning, and taking proactive steps towards better skin health. With the right guidance and care, managing and alleviating the symptoms of these skin conditions is an achievable goal, paving the way to improved comfort and quality of life.
FAQs:
- What are the common triggers for eczema and psoriasis?
- The triggers for eczema and psoriasis can vary. Eczema is often triggered by irritants like soaps, detergents, or allergens such as pollen and pet dander. Psoriasis triggers include stress, infections, and skin injuries. Identifying personal triggers with the help of a healthcare provider can significantly help in managing these conditions.
- How is contact dermatitis diagnosed?
- Diagnosis of contact dermatitis involves a thorough examination by a healthcare provider, detailed history taking, and possibly patch testing to identify specific allergens. The diagnostic process aims to differentiate between irritant and allergic contact dermatitis and identify the causative agents.
- Can scalp eczema lead to hair loss?
- Scalp eczema can potentially lead to temporary hair loss due to severe itching and scratching that may damage the hair follicles. However, with appropriate treatment and symptom management, the hair often grows back.
- Is there a cure for lichenoid dermatitis?
- The treatment of lichenoid dermatitis aims to control symptoms and improve the quality of life. While there may not be a definitive cure, symptoms can often be managed effectively with topical treatments, systemic medications, and by avoiding known triggers.
- What is the relationship between varicose veins and varicose eczema?
- Varicose eczema, also known as stasis dermatitis, often occurs in the presence of varicose veins. Poor circulation and increased pressure in the veins can trigger skin irritation and eczema. Management often involves addressing both the venous insufficiency and the skin inflammation.
- How does seborrheic dermatitis differ from other forms of dermatitis?
- Seborrheic dermatitis is often associated with oily areas of the skin and may be linked to a yeast known as Malassezia. It tends to cause dandruff and red, scaly patches on the skin, differentiating it from other forms of dermatitis which may be triggered by allergens, irritants, or circulatory issues.
- Are there natural remedies for managing psoriasis and eczema?
- Some individuals find relief from natural remedies such as oatmeal baths, coconut oil, or aloe vera for managing psoriasis and eczema. However, it’s essential to consult with a healthcare provider before trying any new treatment to ensure it’s safe and effective for your specific condition.
Blog Tags:
Skin Conditions, Eczema, Psoriasis, Contact Dermatitis, Seborrheic Dermatitis, Lichenoid Dermatitis, Varicose Eczema, Scalp Eczema, Dermatology, Skin Care, Skin Health, Allergic Reactions, Skin Irritation, Skin Treatment, Natural Remedies
Further Reading:
Embark on a journey towards understanding and managing eczema and dermatitis better by exploring our comprehensive guides. Learn about the dietary practices that could ease your eczema symptoms in our post on foods to embrace and avoid for eczema relief. Delve deeper into the irritants that often go unnoticed in our discussion on dermatitis: the hidden irritant.
Discover the underlying causes and effective coping mechanisms for these skin conditions in our post on eczema and dermatitis: causes and coping mechanisms. Lastly, explore a soothing remedy by learning about the benefits of oatmeal baths for eczema and dermatitis. Our blogs aim to provide a holistic approach towards understanding and managing these skin conditions better, making your path towards relief an informed and effective one.