Eczema, or atopic dermatitis, is a stubborn skin condition that affects millions of people—itchy, flaky, sometimes painful, and always searching for answers. It’s no wonder so many of us end up down rabbit holes, asking: Could gluten be making my eczema worse? Should I try going gluten-free? With social media overflowing with “before and after” gluten-free skin transformations, it’s time to get the facts—straight from the latest research.
What Is Gluten, Anyway?
Gluten is a protein naturally found in wheat, barley, and rye. It gives bread its chewy texture and is hidden in everything from pasta and pastries to soy sauce and salad dressings. For most people, gluten is just another ingredient. But for some, it can trigger significant health issues—especially if you have celiac disease or non-celiac gluten sensitivity (NCGS).
Eczema: The Skin’s Cry for Help
Eczema is more than dry skin. It’s an inflammatory condition where the skin’s protective barrier doesn’t work as well as it should. Triggers are as varied as life itself—detergents, weather changes, stress, and yes, sometimes even what we eat. But the link between food and eczema is complicated and highly individual.
Gluten and Eczema: The Science So Far
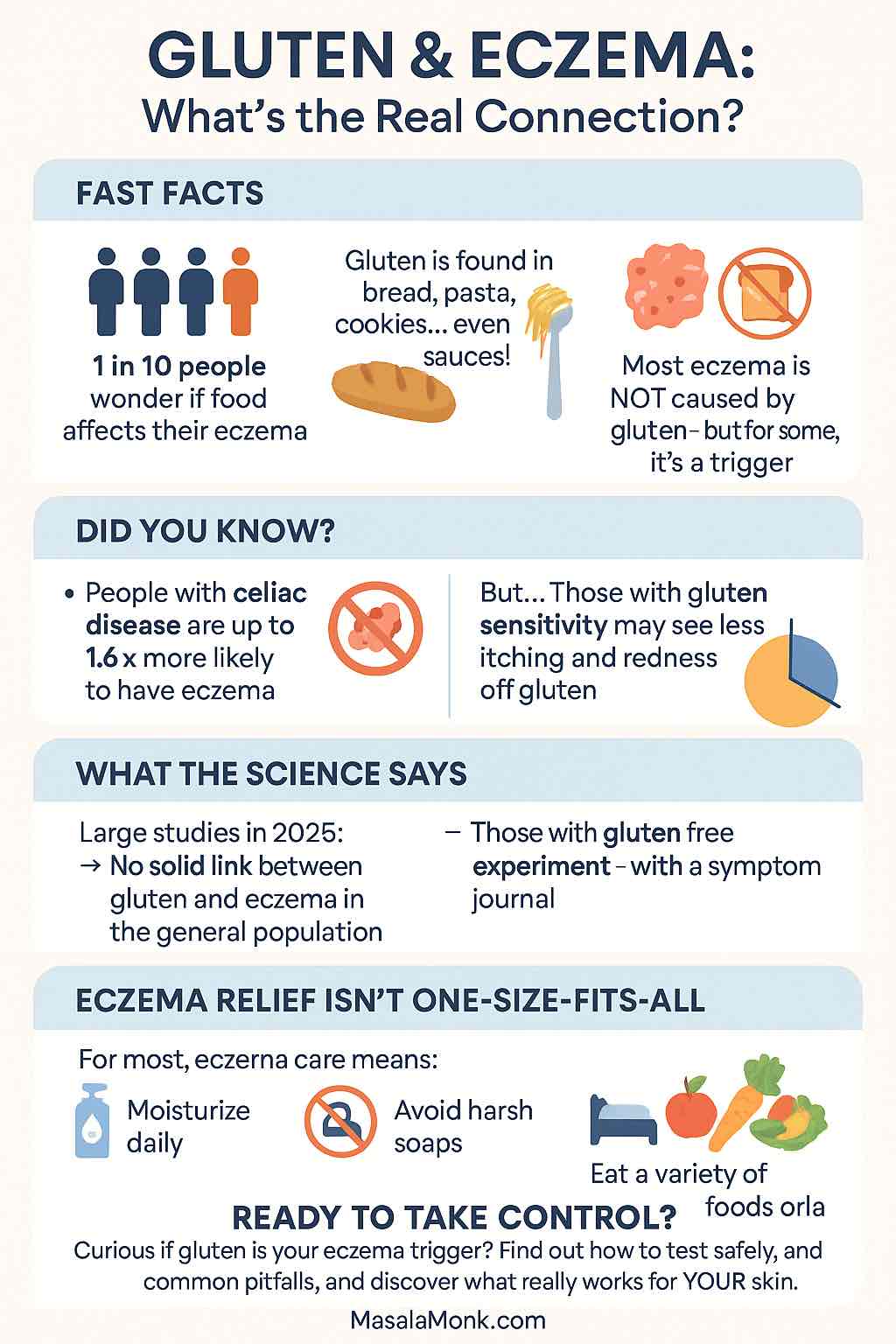
Let’s get one thing out of the way: For most people, gluten does not cause eczema.
What Do the Latest Studies Say?
- Large population studies (like the 2025 UK Penn Medicine cohort) show that having celiac disease may slightly increase your risk of developing eczema, but the absolute risk is low and most people with eczema do not have celiac disease or gluten sensitivity.
- Dermatitis herpetiformis is a specific, gluten-triggered skin rash that looks nothing like classic eczema. It’s intensely itchy, with small blisters—if this sounds familiar, see your doctor for testing.
- In the general population, removing gluten rarely leads to dramatic, consistent improvement in eczema. However, there is a subset of people who report fewer flares and calmer skin on a gluten-free diet.
So Why Do Some People See Improvement?
- If you have undiagnosed celiac disease or NCGS, gluten can contribute to widespread inflammation—including in your skin.
- For some, the improvement may be due to broader changes: eating fewer processed foods, paying more attention to what you eat, and introducing healthier habits overall.
- The famous gut-skin axis: Science is uncovering how what happens in our gut—like increased permeability (“leaky gut”) or imbalanced microbiome—can affect our skin’s health. Gluten can worsen these in sensitive individuals.
How Do I Know If Gluten Is a Problem For My Eczema?
Ask Yourself:
- Do you have digestive symptoms (bloating, diarrhea, pain) with gluten?
- Do you have a family history of celiac disease or gluten sensitivity?
- Have you tried other eczema treatments (moisturizers, topical steroids, trigger avoidance) with little success?
Step-By-Step: Safe Gluten Elimination Trial
- Get Tested First: Before removing gluten, ask your doctor about screening for celiac disease. You need to be eating gluten for tests to work.
- Try a Short Gluten-Free Diet: If tests are negative, but you’re curious, try a strict gluten-free diet for 2-4 weeks. Read labels carefully—gluten hides in surprising places!
- Track Your Symptoms: Keep a food and symptom diary. Note your skin’s appearance, itch level, and any other symptoms.
- Reintroduce Gluten: After the trial, reintroduce gluten for several days and observe. If flares return, you might be sensitive. If nothing changes, gluten may not be your culprit.
- Consult the Experts: A dermatologist or registered dietitian can guide you and help you avoid unnecessary restrictions (and nutritional pitfalls).
What If I Don’t Notice a Difference?
That’s normal! Most people with eczema do not have gluten as a trigger. The best-proven strategies for eczema remain:
- Consistent moisturizing (especially right after showers)
- Identifying and minimizing other triggers (soaps, fragrances, stress)
- Using prescribed medications during flares
Caution: The Risks of Unnecessary Elimination
Gluten-free diets are safe for those who need them, but they’re not automatically “healthier.” Gluten-free processed foods can be lower in fiber and important nutrients. And being overly restrictive can add stress or trigger disordered eating—especially in kids and teens.
The Bigger Picture: Gut Health & Anti-Inflammatory Eating
Emerging research in 2025 is pointing toward overall gut health and whole-diet patterns as more important than cutting out single ingredients. Diets rich in:
- Fruits and vegetables
- Fermented foods (yogurt, kefir, kimchi)
- Healthy fats (olive oil, fatty fish)
- Lean proteins
…all support skin health and can calm inflammation. Gluten isn’t always the villain—sometimes, it’s about the company it keeps.
When To See a Professional
- If your eczema is severe, persistent, or worsening
- If you have symptoms of celiac disease (unexplained weight loss, diarrhea, fatigue, mouth ulcers)
- If you’re considering major dietary changes
In Summary
- Gluten does not cause eczema for most people.
- If you have celiac disease or gluten sensitivity, gluten can trigger or worsen skin issues—including eczema-like rashes.
- A careful, supervised gluten-free trial may help some people—but it’s not a miracle cure.
- Focus on overall diet quality and skin care, not just a single ingredient.
Want to Take Action?
Try this:
Download a food and symptom tracker, talk to your doctor about testing, and make one small, sustainable change this week—like switching to unscented moisturizer or eating an extra serving of vegetables.
And remember: Your eczema journey is unique. The best approach is personalized, patient, and based on your body’s signals—not internet trends.
Have you tried a gluten-free diet for your eczema? Share your experience in the comments below!
Stay curious. Stay kind to your skin. And keep searching for what works for you.
This is for information purpose only. For medical advice, always consult a healthcare professional.
Frequently Asked Questions (FAQs)
1. Can eating gluten make my eczema worse?
For most people, gluten does not directly make eczema worse. However, if you have celiac disease or non-celiac gluten sensitivity, gluten may contribute to skin inflammation or trigger flares.
2. Is there a scientific link between gluten and eczema?
Large studies show no direct link between gluten and eczema in the general population, but there is a higher prevalence of eczema among people with celiac disease or gluten sensitivity.
3. What is dermatitis herpetiformis, and how is it different from eczema?
Dermatitis herpetiformis is a specific, gluten-triggered skin rash (small, itchy blisters), directly linked to celiac disease. It’s distinct from typical atopic dermatitis (eczema).
4. Should I try a gluten-free diet if I have eczema?
If you suspect gluten is a trigger or have digestive symptoms, consult your doctor about testing for celiac disease first. If tests are negative, you can consider a supervised gluten-free trial for 2–4 weeks, tracking your symptoms.
5. How soon would I notice a difference in my eczema after cutting out gluten?
If gluten is a trigger, some people notice changes within 1–4 weeks. However, if you see no change after a month, gluten is likely not a major factor for you.
6. Can children with eczema benefit from a gluten-free diet?
There’s no evidence that children with eczema need to avoid gluten unless they have a diagnosed gluten-related disorder. Always consult a pediatrician or dietitian before changing a child’s diet.
7. What are the risks of going gluten-free unnecessarily?
Unnecessary gluten elimination can lead to nutritional deficiencies, reduced fiber intake, higher food costs, and unnecessary stress—especially if not planned carefully.
8. What are other common food triggers for eczema?
Common triggers include cow’s milk, eggs, soy, peanuts, and certain preservatives. Food triggers are individual, so not everyone with eczema is affected by the same foods.
9. How can I test if gluten is affecting my eczema?
Keep a detailed food and symptom diary. Try a gluten-free diet for 2–4 weeks under professional guidance, then reintroduce gluten and observe any changes.
10. Is it okay to do a gluten elimination diet on my own?
It’s best to consult a healthcare provider or dietitian before making major dietary changes, to ensure you’re meeting nutritional needs and to properly evaluate your response.