If you’ve ever dealt with an itchy, flaky scalp, you may have found yourself wondering: Is this seborrheic dermatitis or scalp psoriasis? You’re not alone. Thousands of people search for the difference between these two skin conditions every month, and with good reason—they often look similar, feel uncomfortable, and affect your quality of life. Yet, the causes, treatments, and long-term implications of each are very different.
In this post, we’ll explore the nuances between seborrheic dermatitis and psoriasis, especially as they appear on the scalp. Whether you’re trying to understand your symptoms or researching treatment options, this detailed guide will help you decode the key differences and know what steps to take next.
What Is Seborrheic Dermatitis?
Seborrheic dermatitis is a common, chronic skin condition characterized by red, flaky, greasy patches of skin. It’s most commonly found on areas of the body rich in oil-producing (sebaceous) glands, such as the scalp, face (especially around the nose and eyebrows), chest, and back.
Causes:
- Overgrowth of Malassezia, a type of yeast normally present on the skin
- Excess oil production
- Genetic predisposition
- Environmental factors (e.g., cold weather, stress)
Symptoms:
- Greasy or oily yellowish scales
- Red or pink base
- Itching (mild to moderate)
- Worse in winter or under stress
What Is Psoriasis?
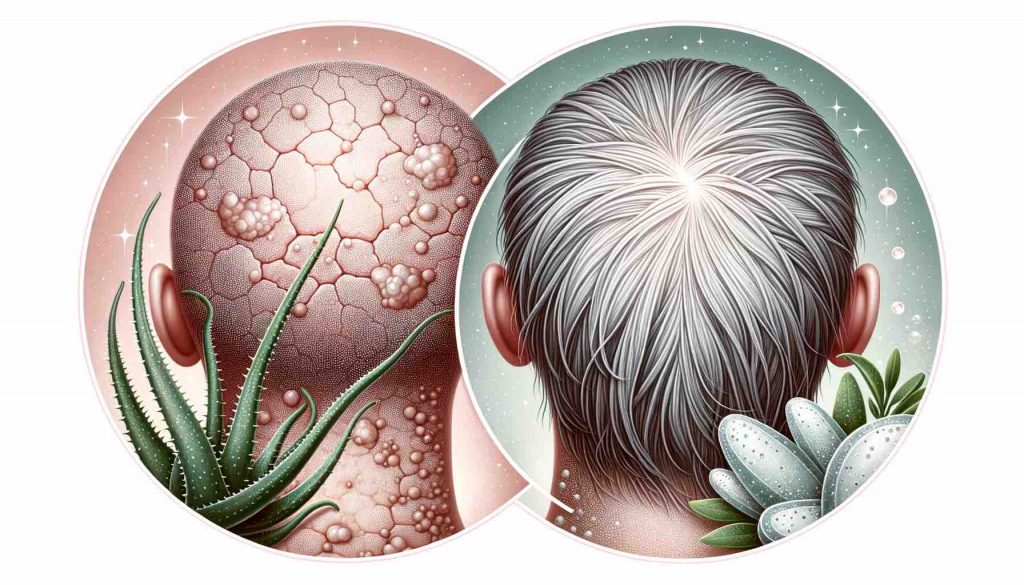
Psoriasis is a chronic autoimmune condition that causes the skin to regenerate at an abnormally fast rate, leading to the buildup of skin cells. This results in thick, scaly patches that can appear anywhere on the body, including the scalp.
Causes:
- Autoimmune dysfunction
- Genetic predisposition
- Triggers like infections, stress, injury to the skin, or certain medications
Symptoms:
- Thick, silvery-white scales over well-defined red plaques
- Intense itching or burning
- Nail pitting or discoloration
- Possible joint pain (psoriatic arthritis)
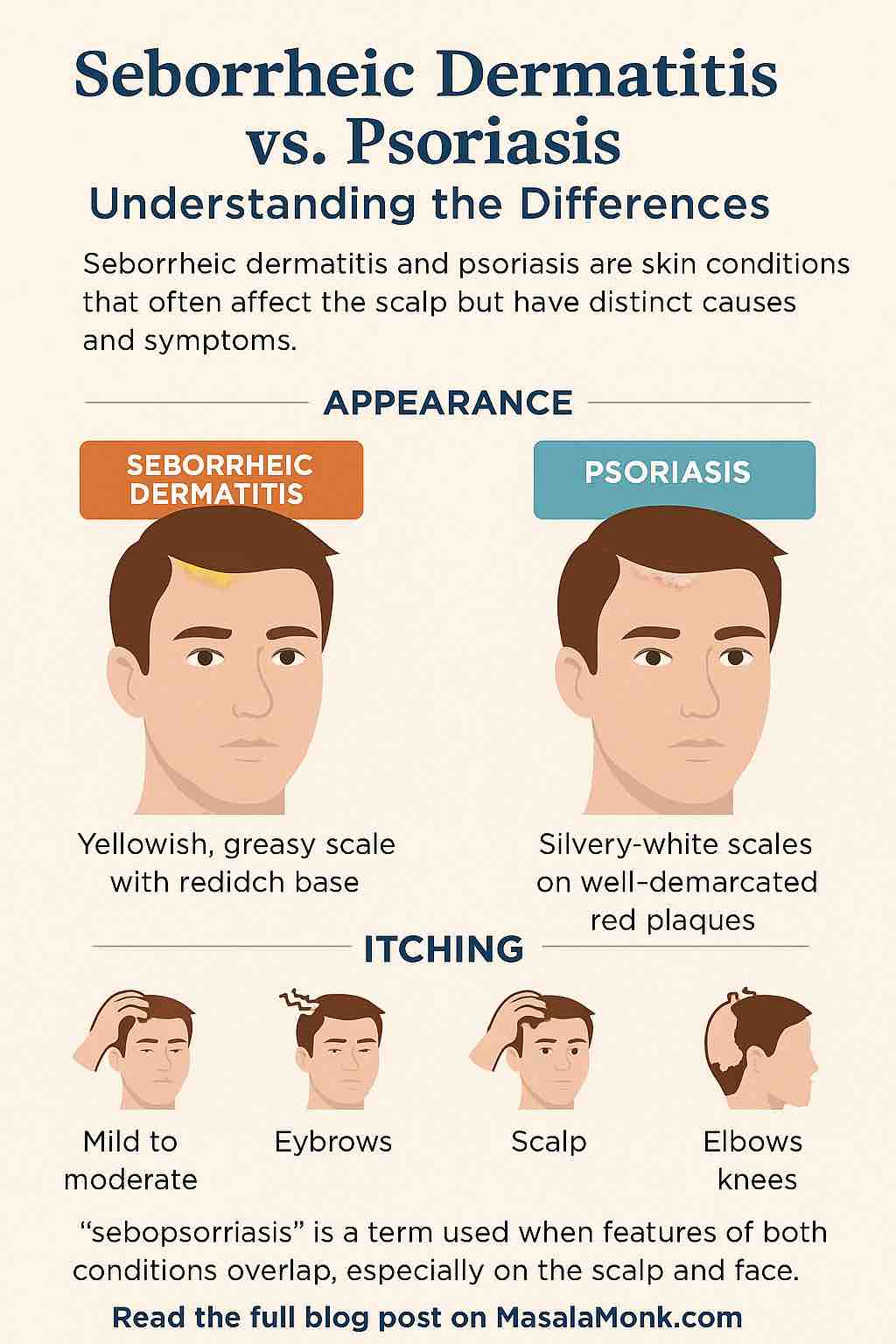
Scalp Focus: Where It Gets Confusing
Both seborrheic dermatitis and psoriasis frequently affect the scalp. This overlapping location is one of the main reasons they’re often confused. However, there are clues that can help you distinguish between them:
| Feature | Seborrheic Dermatitis | Scalp Psoriasis |
|---|---|---|
| Scale Type | Greasy, yellowish, flaky | Dry, silvery, thick |
| Redness | Mild to moderate | Often deep red |
| Demarcation | Ill-defined edges | Sharp, well-demarcated plaques |
| Itching | Mild to moderate | Moderate to severe |
| Common in | Infants (cradle cap), adults | Teenagers and adults |
| Associated Symptoms | Dandruff, oily skin | Nail pitting, joint pain |
Overlapping Condition: Sebopsoriasis
In some cases, patients may exhibit symptoms of both conditions simultaneously, especially on the scalp and face. This has led dermatologists to use the term “sebopsoriasis” to describe a hybrid presentation. Treatment here may need to combine elements of both antifungal and anti-inflammatory therapies.
Diagnosis: How Doctors Tell Them Apart
Diagnosing these conditions usually involves a physical examination, but in uncertain cases, a dermatologist may perform a skin biopsy. Other diagnostic clues include:
- Response to treatment: Rapid improvement with antifungal shampoo often suggests seborrheic dermatitis.
- Location: Elbows, knees, and lower back involvement typically points to psoriasis.
- Other signs: Nail changes and joint symptoms are much more indicative of psoriasis.
Treatment Comparison
| Treatment | Seborrheic Dermatitis | Psoriasis |
| Topical Antifungals | Often effective (e.g., ketoconazole) | Not effective |
| Topical Steroids | Used in flare-ups | Often used, more potent versions needed |
| Vitamin D Analogues | Rarely used | Common (e.g., calcipotriol) |
| Coal Tar | Sometimes helpful | Sometimes helpful |
| Biologics/Systemic Meds | Not used | Common for moderate to severe cases |
When to See a Dermatologist
If you’re unsure what you’re dealing with, it’s time to consult a dermatologist. Prompt diagnosis can lead to more effective management and prevent unnecessary frustration or worsening symptoms.
Seek professional advice if:
- Your scalp symptoms persist despite OTC treatments
- You notice symptoms in other areas like elbows, knees, or nails
- You experience joint pain or stiffness
- The condition is affecting your self-esteem or quality of life
Final Thoughts
Both seborrheic dermatitis and psoriasis can be chronic and recurring, but understanding the difference is key to finding relief. Seborrheic dermatitis is typically driven by yeast and oil, while psoriasis is an immune-mediated condition. Though they can look similar, especially on the scalp, there are distinct clues to help tell them apart.
Accurate diagnosis and personalized treatment can dramatically improve your symptoms. If in doubt, seek medical advice—your scalp will thank you.
Have questions or experiences to share? Drop them in the comments below or connect with a dermatologist near you.
✅ Frequently Asked Questions (FAQs)
- How can I tell if my flaky scalp is psoriasis or seborrheic dermatitis?
Look at the scale and redness: seborrheic dermatitis causes greasy, yellowish flakes with mild redness, while psoriasis causes thick, silvery-white scales over sharply defined red patches. If the itching is intense and you’re noticing symptoms on elbows, knees, or nails, psoriasis is more likely. - Can I have both psoriasis and seborrheic dermatitis at the same time?
Yes. This overlapping presentation is known as sebopsoriasis, especially common on the scalp and face. Treatment may need to combine antifungal and anti-inflammatory approaches. - Does dandruff mean I have seborrheic dermatitis?
Not necessarily, but dandruff is considered a mild form of seborrheic dermatitis. If flakes are greasy and you have red, irritated skin in oily areas, it may be seborrheic dermatitis. - Can stress trigger scalp psoriasis or seborrheic dermatitis?
Yes, stress is a common trigger for both conditions. It can cause flare-ups and worsen existing symptoms by impacting immune or oil gland function. - What’s the best shampoo for seborrheic dermatitis?
Look for shampoos with ketoconazole, selenium sulfide, or zinc pyrithione. These antifungal agents help reduce yeast on the scalp, which is a key factor in seborrheic dermatitis. - Is psoriasis contagious?
No, psoriasis is not contagious. It’s an autoimmune condition, not an infection, so it can’t be passed from person to person. - Does seborrheic dermatitis go away permanently?
It often improves with treatment but may return, especially during stress, seasonal changes, or if not managed well. It’s a chronic condition that can be controlled but not cured. - Will scalp psoriasis cause hair loss?
Psoriasis doesn’t directly cause permanent hair loss, but excessive scratching or harsh treatments may lead to temporary shedding. Treating the inflammation helps reduce this risk. - Can diet help with psoriasis or seborrheic dermatitis?
Diet plays a supporting role. In psoriasis, anti-inflammatory diets may help some people. For seborrheic dermatitis, limiting sugar and processed foods might help reduce yeast overgrowth, although evidence is limited. - When should I see a doctor for scalp issues?
If OTC treatments don’t help within a few weeks, or you notice symptoms spreading, worsening, or involving nails or joints, consult a dermatologist for a proper diagnosis and personalized treatment plan.