Introduction
Varicose eczema, also known as venous, gravitational, or stasis eczema, is a long-term skin condition that affects the lower legs of older adults, but it can also appear in younger people and children. This condition is closely related to increased pressure in the leg veins, often manifesting in people who have varicose veins. It’s essential to delve deeply into understanding varicose eczema, unraveling its causes, symptoms, and the underlying mechanisms that contribute to its development. This comprehensive exploration aims to shed light on the various facets of varicose eczema, providing a detailed insight into managing and navigating through this challenging condition.
Understanding Varicose Eczema
Varicose eczema is a manifestation of a more significant issue related to the veins’ functionality in the legs. It is crucial to perceive this condition as a part of a broader spectrum of venous insufficiency. The skin changes that occur are due to the malfunctioning valves in the veins, which lead to blood pooling in the lower legs, causing increased pressure that affects the skin.
Symptoms and Identification
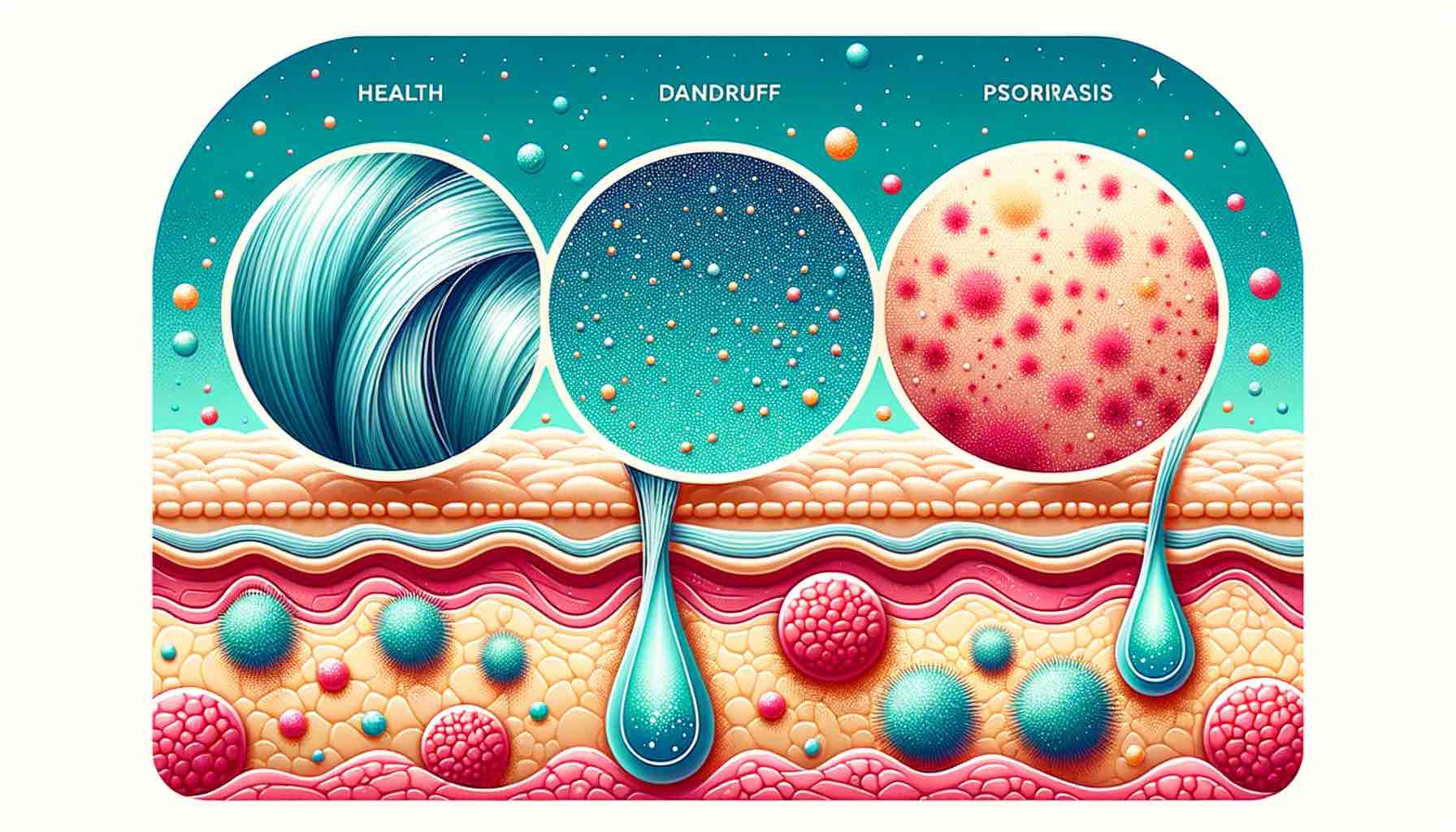
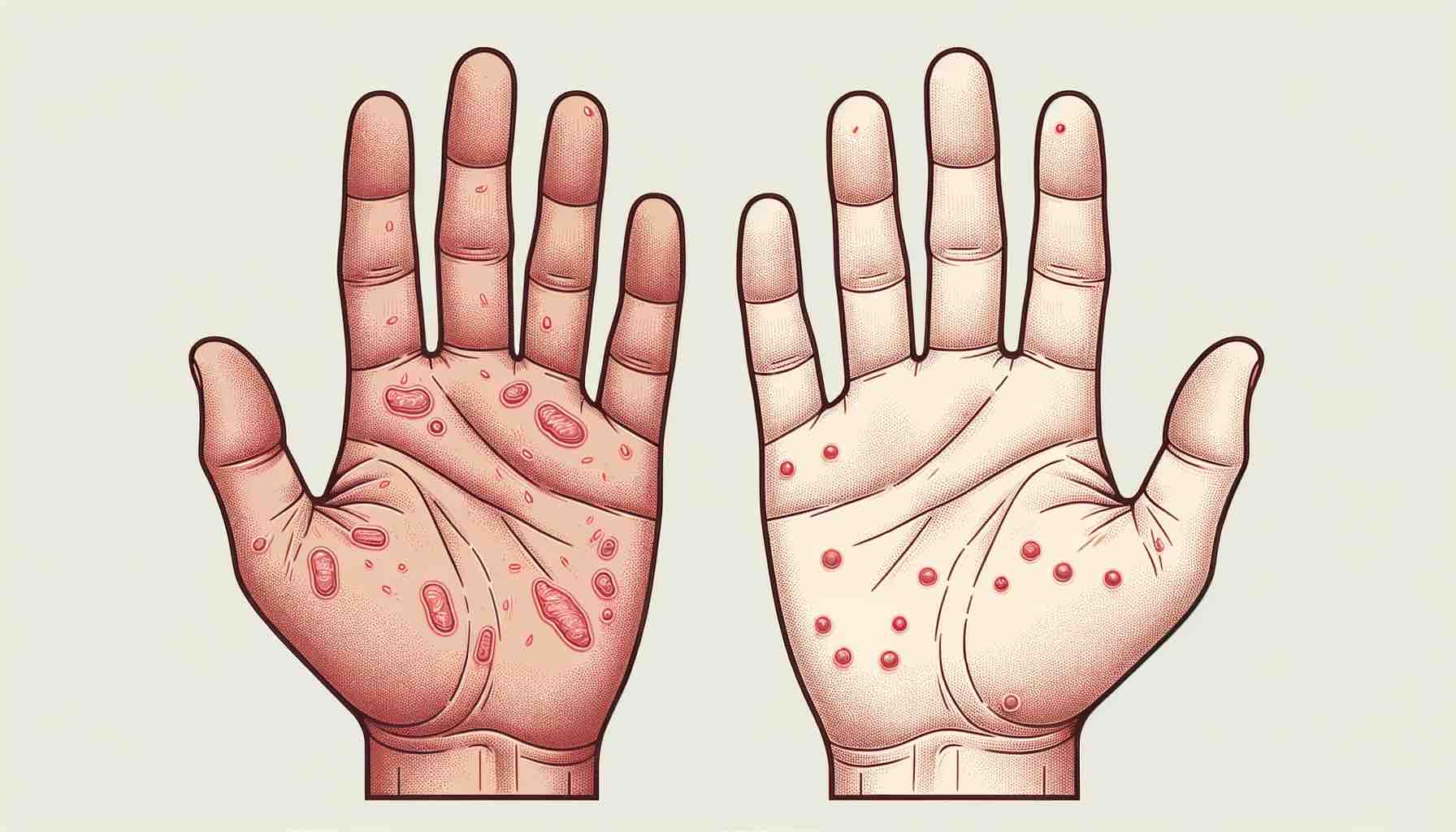
Varicose eczema presents itself in various forms, ranging from mild to severe symptoms. Initially, it may appear as areas of dry, itchy, and irritated skin around the varicose veins. As it progresses, the skin may become red, swollen, and inflamed, leading to significant discomfort.
The affected areas, primarily located around the ankles and lower legs, may become speckled with white scars and areas of dark pigmentation. In more advanced stages, the skin may become thickened and cracked, and painful ulcers may develop, posing a risk of infection.
Unveiling the Causes
The onset of varicose eczema is closely linked to the functionality of the veins in the legs. When the valves in the veins do not work effectively, it leads to venous hypertension, causing blood to pool in the veins. This increased pressure affects the skin, leading to the symptoms associated with varicose eczema.
Several factors contribute to the risk of developing this condition, such as aging, heredity, obesity, hormonal changes, and a history of deep vein thrombosis (DVT). Understanding these contributing factors is crucial in devising effective strategies for prevention and management.
Exploring Treatment Avenues
Treatment of varicose eczema aims at managing the symptoms and preventing complications such as infection. Topical treatments, including corticosteroids and emollients, play a pivotal role in managing inflammation and maintaining skin hydration.
Compression therapy is another essential component in the treatment regimen. It involves the use of compression stockings or bandages to improve blood flow in the legs, reducing the symptoms associated with venous insufficiency.
Navigating Through Self-Care and Preventive Strategies
Self-care plays a crucial role in managing varicose eczema and preventing its recurrence. Incorporating specific practices and lifestyle modifications can make a significant difference in managing the condition effectively.
- Elevation of the Legs: Regularly elevating the legs above the heart level helps reduce pressure in the leg veins, promoting better blood flow and alleviating symptoms.
- Exercise: Engaging in exercises like walking can improve blood circulation in the legs, aiding in the management of varicose eczema.
- Skin Care: Keeping the skin clean and moisturized is essential. Using emollients can prevent the skin from drying and cracking, reducing the risk of infection.
- Avoiding Irritants: It’s advisable to avoid substances that may irritate the skin, such as harsh soaps and detergents. Opting for hypoallergenic products can be beneficial.
Medical Interventions and Advanced Treatments
In cases where varicose eczema is persistent or severe, more advanced medical interventions may be necessary. Treatments such as endothermal ablation, sclerotherapy, and ligation and stripping may be considered to manage the underlying venous insufficiency.
Complications and Challenges
Varicose eczema can lead to complications such as skin infections and leg ulcers if not adequately managed. Understanding the potential risks and being proactive in seeking timely intervention is crucial to prevent adverse outcomes.
Conclusion
Varicose eczema is a multifaceted condition that requires a comprehensive approach to management. By amalgamating medical treatments with self-care strategies, it is possible to navigate through the challenges posed by this condition effectively, enhancing the quality of life.
Further Reading
- Approaches to Scrotal Eczema Treatment
- Alcohol and Eczema: What is the Connection?
- Challenges of Eczema on the Neck
Exploring these resources will provide a broader perspective on managing various aspects of eczema, offering insights into holistic approaches and targeted strategies for effective management and relief.
FAQs
- What causes varicose eczema? Varicose eczema is primarily caused by poor circulation in the legs, often due to issues like varicose veins where the valves in the veins don’t function correctly, causing blood to pool in the lower legs.
- How is varicose eczema different from other types of eczema? Varicose eczema is specifically linked to venous insufficiency and primarily affects the lower legs, whereas other types of eczema might not have a direct link to circulatory issues and can affect various parts of the body.
- Can varicose eczema lead to more severe skin conditions? Yes, if left untreated, varicose eczema can lead to complications such as skin infections and leg ulcers, emphasizing the importance of early and effective management.
- What are the common symptoms of varicose eczema? Symptoms include itchy, swollen, and red skin, and in more severe cases, the skin may become crusty, scaly, or develop blisters.
- Are there any natural remedies effective against varicose eczema? Natural remedies like keeping the skin moisturized and using compression stockings can be beneficial alongside medical treatments. However, it’s essential to consult a healthcare professional for a personalized approach.
- How can one prevent the recurrence of varicose eczema? Regular leg elevation, exercise, and wearing compression stockings are preventive strategies that can help manage the condition and reduce recurrence chances.
- Is varicose eczema contagious? No, varicose eczema is not contagious. It is related to internal factors like poor blood circulation in the legs.
- What types of medical specialists should one consult for varicose eczema? Dermatologists and vascular specialists are key healthcare professionals who can provide comprehensive care and treatment options for varicose eczema.
- Can diet and nutrition impact varicose eczema? While there isn’t a direct link, a healthy diet promoting good vascular health might indirectly benefit individuals with varicose eczema.
- Are there any specific risks associated with the medical treatments for varicose eczema? Risks depend on the specific type of treatment. For surgical interventions, there might be risks like infection or scarring, so discussing with a healthcare professional is crucial for informed decision-making.
Learn More about Eczema
For a more comprehensive understanding of eczema and various approaches to manage and treat it, consider exploring the following articles. These resources are meticulously curated to provide a wealth of information, insights, and practical advice on dealing with different aspects of eczema.
- Tea Tree Oil and Eczema: A Natural Remedy Explored: Dive into the therapeutic potentials of tea tree oil as a natural remedy in managing eczema symptoms, and discover how to utilize it effectively.
- Apple Cider Vinegar and Eczema: Explore the role of apple cider vinegar in soothing eczema symptoms, and learn how to incorporate it into your skincare routine for better management of eczema.
- Side Effects of Steroid Creams for Eczema: Gain insights into the potential side effects of using steroid creams for eczema treatment, and understand how to use them safely.
- Biologics for Eczema: A New Era of Eczema Treatment: Explore the revolutionary role of biologics in eczema treatment, offering a new perspective and approach in managing severe eczema cases.
- Healing Eczema Naturally: Discover various natural strategies and remedies that can be employed to manage and alleviate the symptoms of eczema effectively.
Each of these articles offers a unique perspective and valuable information on managing eczema, helping you to navigate through the complexities of this skin condition with greater confidence and understanding.
Blog Tags varicose eczema, venous eczema, eczema treatment, skin care, vascular health, natural remedies for eczema, leg eczema, eczema complications, eczema prevention, dermatology