When to Take Metamucil: Morning, Night, or With Meals
If you’re bringing Metamucil into your day, you’re usually chasing one of three wins: easier, more regular bathroom trips; a little extra fullness that helps with portions; or a nudge in the right direction for LDL cholesterol. The good news is that Metamucil is simple, flexible, and forgiving. You don’t need a perfect schedule—you need a consistent one, a full glass of water, and a couple of smart guardrails around bedtime and other medicines.
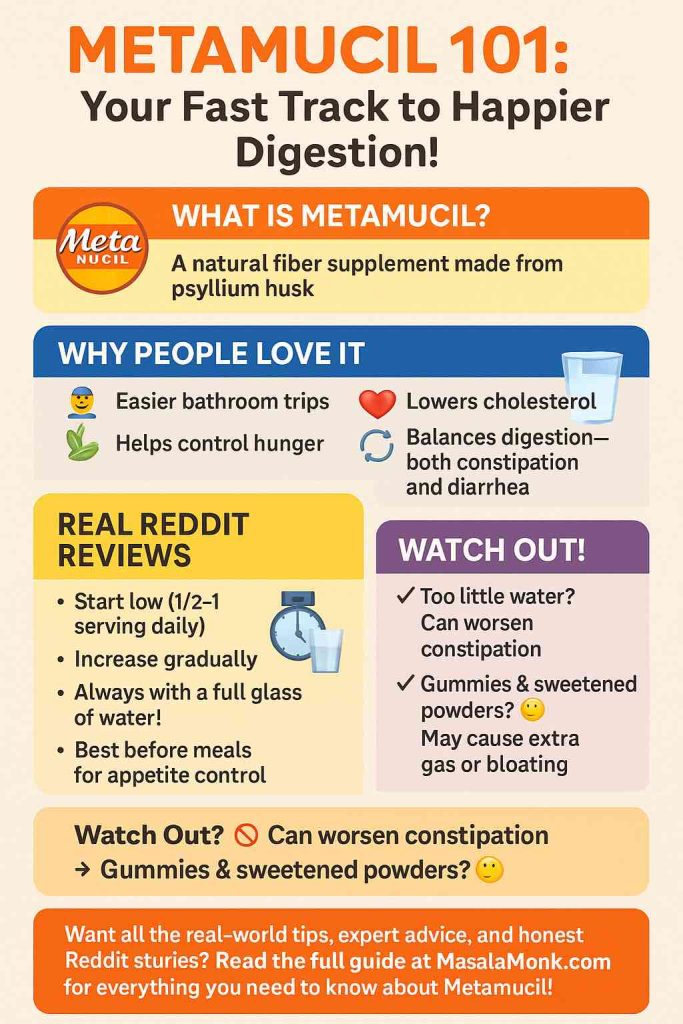
Metamucil’s active ingredient is psyllium husk (also called ispaghula), a soluble, gel-forming fiber (learn more about psyllium husk benefits and side effects; quick refresher on the health benefits of fiber, plus food examples of soluble vs insoluble fiber in foods). Mixed with enough liquid, it swells into a soft gel that helps bulk and soften stool and, with daily use, can support healthier cholesterol levels. For a neutral primer on what psyllium is and how it behaves in your gut, see MedlinePlus. For product formats and serving examples (powders, capsules, gummies), browse the brand’s pages at Metamucil.
⚠️ Disclaimer: This material is for educational and informational purposes only and not a substitute for professional medical advice, diagnosis, or treatment. Don’t ignore or delay professional care because of something you read here. Always talk with your doctor or pharmacist about whether Metamucil (psyllium) is appropriate for you, how to time it with your other medicines, and the right dose for your situation. If you think you may be experiencing a medical emergency, call your local emergency number immediately.
Ground rules that never change
Water is non-negotiable. Every labeled dose should be mixed with at least 8 oz (≈240 ml) of liquid and drunk promptly. Over-the-counter Drug Facts for Metamucil and other psyllium products also note that bulk-forming laxatives typically “produce a bowel movement in 12–72 hours.” You can see those instructions on official label listings at DailyMed—for example, Metamucil “Therapy for Regularity” powder entries spell out the 8-oz mixing rule, choking warning, and expected onset window. If label jargon is new to you, here’s a plain guide on how to read nutrition labels.
Give other medicines some space. Psyllium can reduce or delay absorption of certain oral meds. The simple rule: leave a 2-hour buffer (other meds two hours before or after your Metamucil dose). Administration and interaction notes are laid out clearly on Drugs.com and the capsule monograph at Drugs.com.
Why the water rule really matters. A safety bulletin described a fatal choking incident when psyllium was taken with applesauce instead of a full glass of liquid—an avoidable tragedy that underlines why we always use enough fluid and drink right after mixing. See ISMP Canada and the consumer explainer at ISMP Canada.
Also Read: Side Effects of Taking Metamucil Every Day: What You Should Know
Quick orientation: match timing to your goal
- Regularity (constipation, travel, everyday rhythm): pick any time you’ll remember and stay consistent. Expect effects in 12–72 hours as per label language compiled on DailyMed.
- Satiety/portion control (weight-management helper): take Metamucil 15–30 minutes before meals so the gel forms before food arrives. Practical around-mealtime framing appears in Harvard Health.
- Cholesterol (LDL): the clock matters less than your daily total. Aim for roughly ~10 g/day of psyllium (from your Metamucil servings) for 3+ weeks. Evidence summaries are outlined at Harvard Health and Harvard Health. The authorized U.S. health claim for soluble fiber from psyllium husk sits in 21 CFR §101.81.
We’ll unpack each of these in detail next.
For bigger-picture meal planning, pairing fiber with protein can help—see our posts on high-protein, high-fiber for weight management and food-first options like soluble vs insoluble fiber in foods.
Metamucil for regularity: consistency beats the clock
Your gut loves rhythm. If your aim is smoother, more predictable bathroom habits, there’s no “magic hour”—there’s the hour you won’t forget. Some people like their first big glass of water in the morning; others prefer late afternoon or early evening. Stick to one slot for a few days before you judge results. Bulk-forming fibers typically “work” in 12–72 hours—that’s why day one doesn’t tell you much, but day three usually does. Those expectations and directions are set out on DailyMed.
Make it stick (real-world tips):
- Pour water first, dose second. It’s a tiny ritual that prevents dry scoops and half-sips.
- Pair it with a habit. Kettle on → mix → drink → brew tea.
- Start low, go slow. Gas/bloating usually settle if you build up gradually and split doses.
- Prefer food-first adds on top of your supplement? Consider easy extras like flax seeds for digestion and regularity or even fruit options such as kiwi for constipation relief.
Metamucil before meals: a head start for fullness
If you’re using Metamucil as a satiety helper, timing it 15–30 minutes before meals gives the fiber a head start to gel in your stomach. That often means you feel “that’s enough” a bit sooner and naturally rein in portions without much effort. Many people choose lunch and dinner (the meals where portions creep). This practical around-mealtime approach is discussed at Harvard Health. For a dietary combo that plays nicely with this routine, see high-protein, high-fiber for weight management, and consider fiber-rich staples like millets for fiber and weight loss.
A simple routine that works: set a quiet reminder 20 minutes before the meal you tend to overeat, mix your Metamucil with a full glass of water, drink, then plate your food. If you’re brand-new to fiber supplements, try one pre-meal dose daily for a week, then add the second once your gut gives the thumbs-up.
Metamucil for cholesterol: daily grams and consistency win
When LDL is the goal, dose + streak matter far more than the hands on the clock. Summaries pooling dozens of trials report that around 10 g/day of psyllium (from Metamucil servings) taken for at least ~3 weeks lowers LDL cholesterol. You’ll see that dose-plus-consistency theme across multiple articles at Harvard Health and Harvard Health. A classic meta-analysis of controlled trials reported reductions in total and LDL cholesterol with psyllium added to a heart-healthy diet: American Journal of Clinical Nutrition (Anderson et al.). And if you’re wondering whether morning vs evening changes the cholesterol result, one randomized trial found no meaningful time-of-day effect: BMC (Van Rosendaal et al.).
Two easy ways to hit the target without overthinking it:
- Split doses (e.g., 5 g with breakfast + 5 g with dinner).
- One larger dose if your product allows and your gut is comfortable—at the meal you never skip.
For the regulatory backdrop on heart-health language around psyllium, see 21 CFR §101.81.
A simple food partner to psyllium is oats—rich in beta-glucan—see our post on healthy oat protein bars for easy ways to get them in.
⚠️ This page provides general education about Metamucil (psyllium). It isn’t medical advice, diagnosis, or treatment. Always consult your doctor or pharmacist about timing, dose, and potential interactions.
Morning or night? Either—just avoid right before bed
Morning is convenient and pairs naturally with your first big glass of water. Night can work too—with one caution: avoid taking Metamucil right before bed. UK patient guidance recommends leaving about an hour before lying down and, as always, drinking a full glass of water; your gut naturally slows overnight, and a thickening gel plus not-enough fluid isn’t a combo you want. You’ll see that advice in the NHS guide and a practical UK hospital leaflet – for fybogel, another ispaghula husk brand & make, not much different from Metamucil.
Comfortable evening routine: after dinner and dishes, mix your Metamucil with a full glass of water while you prep tomorrow’s lunch. By the time you’re winding down, you’ve left a healthy buffer before sleep. (If you’d rather lean on foods in the evening, fiber-forward grains like millets for fiber and weight loss can help round out dinner.)
Before or after meals?
Match timing to the job you want Metamucil to do:
- Before meals (15–30 minutes) when the priority is satiety/portion control—you want the gel “in place” before the food arrives. (Mealtime framing at Harvard Health.)
- With meals when consistency is the main challenge or when you’re targeting cholesterol and simply need to hit your daily grams. (Evidence overview at Harvard Health.)
- Any consistent time for regularity, with adequate fluid. The onset window is 12–72 hours, reflected on label directions compiled at DailyMed.
Across all three, the golden rule is the same: mix with at least 8 oz of liquid and drink promptly so it doesn’t set up in the glass. That instruction lives on the Drug Facts labels at DailyMed. For brand-specific serving formats and flavors, check Metamucil.
How long does Metamucil take to work?
Let’s set expectations so you don’t quit too early.

- For regularity: bulk-forming laxatives generally “produce a bowel movement in 12–72 hours,” according to label language compiled at DailyMed.
- For cholesterol: think in weeks, not days. Summaries at Harvard Health describe meaningful LDL changes after ~3 or more weeks of steady daily intake—often pegged around 10 g/day. The legal framing of the heart-health claim around psyllium is in 21 CFR §101.81.
A friendly shorthand: bowel effects in days, cholesterol effects in weeks.
⚠️ Educational content, not medical advice. If you have a condition, take prescription medicines, or are pregnant/breastfeeding, ask your clinician or pharmacist before using fiber supplements.
Exactly how to take Metamucil (powder, capsules, gummies)
Formats vary, but a few principles make any version work better.
Powder
- Mixing: put the labeled serving in an empty glass, add ≥ 8 oz water (or permitted liquid), stir briskly, and drink right away—it thickens quickly.
- Frequency: most OTC labels allow adults to take it up to three times daily as needed.
- Why the hurry? You want the gel forming in you, not in the glass. These instructions are standard on Drug Facts at DailyMed. For flavor/format specifics, see Metamucil.
Comfort tips: colder water goes down easier; a shaker bottle avoids clumps; unflavored powder into lightly flavored water works if you dislike sweetness.
Capsules
- How to take: swallow the labeled number one at a time with a full glass of cool water—don’t dry-swallow and don’t try to gulp a handful with a sip.
- Why so specific? Capsules still swell; you want enough liquid to help them slide down and disperse safely. Administration and spacing advice are laid out at Drugs.com. For capsule product details, see Metamucil.
Gummies
- How to take: follow your pack’s serving and hydrate afterward. They’re convenient for taste/texture, but water still matters for a comfortable transit.
Give your other medicines some space
Psyllium can bind or slow the absorption of certain medicines and supplements. Unless your prescriber says otherwise, keep a 2-hour buffer—other oral meds two hours before or after your Metamucil dose. The spacing rule (along with “full glass of cool water” and “swallow capsules one at a time”) is spelled out at Drugs.com and the capsule monograph Drugs.com.
If you take time-sensitive meds (e.g., certain thyroid drugs or diabetes medicines), ask your pharmacist to sanity-check your plan. The buffer is usually enough—but a quick chat prevents guesswork.
For basics readers often ask about, here’s our post on probiotics and gut health.
⚠️ Informational only. Psyllium can affect absorption of other medicines. Confirm timing and spacing with your doctor or pharmacist, especially for time-sensitive drugs (e.g., thyroid or diabetes meds).
Safety, side effects, and sensible precautions
Most people tolerate Metamucil well. Early on, gas or mild bloating can show up as your gut microbes adjust to the extra fermentable fiber. That usually settles if you build up gradually, split the daily amount into smaller servings, and keep fluids generous.
Non-negotiables to keep it safe and comfortable:
- Always mix with at least 8 oz of liquid and drink promptly. Those aren’t suggestions; they’re label directions on DailyMed.
- Avoid right-before-bed dosing. Leave about an hour before lying down and hydrate well, per the NHS and this UK hospital leaflet – (for fybogel, another ispaghula husk brand).
- Keep a 2-hour gap from other oral medicines, per Drugs.com.
- Know why water matters. Safety alerts from ISMP Canada are a clear reminder to use a full glass of liquid, not thick purees.
- Want more context from our site? See side effects of taking Metamucil every day and a broader look at side effects of Metamucil.
Who should check with a clinician first?
Anyone with difficulty swallowing, a history of strictures or bowel obstruction, or complex medication schedules that can’t easily be spaced from fiber. If you’re pregnant, bulk-forming fibers have minimal systemic absorption and are generally considered compatible; still, confirm your plan with your own provider. For a neutral overview, see MedlinePlus.
⚠️ Educational content. Bulk-forming fibers are generally considered compatible in pregnancy, but confirm with your clinician if you’re pregnant, planning pregnancy, or breastfeeding.
Troubleshooting (so you don’t quit on day three)
“I feel bloated.”
Check two basics first: how much water you’re using and how fast you ramped up. Mix with a full 8–12 oz, sip a little extra water afterwards, and split your total into two smaller servings at different times. The “full glass + prompt drinking” instruction is straight from Drug Facts on DailyMed.
“It’s not doing anything.”
Bulk-forming fibers aren’t instant. The expected window for a bowel movement is 12–72 hours. If nothing’s happening, make sure your day includes adequate fluids, a bit of movement, and consistent dosing. That 72-hour window is pulled from label directions on DailyMed. If loose stools show up as you tweak routines, these are helpful electrolytes for diarrhea: best natural drinks & remedies.
“The texture makes me gag.”
Try colder water, use a shaker, and drink right after mixing before it thickens. If powder still isn’t your friend, capsules are an option—just remember the full glass of cool water and the “one at a time” rule at Drugs.com.
“Can I take it at night?”
Yes—just not right before bed. Leave about an hour, hydrate, and you’re fine. That buffer is the exact patient advice in the NHS guide and reiterated in a UK hospital leaflet.
“I’m on several medications.”
Use the 2-hour spacing rule by default and ask your pharmacist to double-check any special cases. The interaction overview is easy to scan at Drugs.com.
Two ready-to-use daily plans (pick the one that fits your life)
Plan A — The “Before Meals” routine (satiety + cholesterol friendly)
- Lunch: set a reminder 20 minutes before; mix Metamucil with a full glass of water, drink, then plate your food.
- Dinner: repeat the same pattern.
- Weekly check-in: are portions a bit smaller? Any gas? If yes, split the amounts or add an extra half-cup of water. Practical mealtime timing appears in Harvard Health.
Plan B — The “With Meals” routine (cholesterol + consistency)
- Breakfast: first serving with your meal.
- Dinner: second serving with your meal.
- Target: make sure your day adds up to ~10 g psyllium (from your Metamucil servings), since Harvard Health reviews show LDL benefits after ~3+ weeks at that total. The authorized claim framework sits in 21 CFR §101.81.
Also Read: Top 10 Foods for Gut Health.
The bottom line
- Regularity: take Metamucil whenever you’ll remember, with a full 8-oz glass of liquid, and give it 12–72 hours—the plain-English, label-level guidance compiled on DailyMed.
- Satiety: go 15–30 minutes before meals so the gel’s ready when the food arrives—see the mealtime framing at Harvard Health.
- Cholesterol: aim for ~10 g/day for 3+ weeks; consistency beats clock time—summarized at Harvard Health and supported by pooled data in the American Journal of Clinical Nutrition; time-of-day differences aren’t meaningful per BMC.
- Safety: avoid right-before-bed dosing, keep a 2-hour buffer from other oral meds, and always use enough water—patient guidance via the NHS (for fybogel, another ispaghula husk brand), administration/interaction details at Drugs.com, safety alerts from ISMP Canada, and product context from Metamucil.
Choose your goal, pick a time you’ll stick with, pour your water first, and let Metamucil be quietly good to you.
⚠️ Disclaimer: This material is for educational and informational purposes only and not a substitute for professional medical advice, diagnosis, or treatment. Don’t ignore or delay professional care because of something you read here. Always talk with your doctor or pharmacist about whether Metamucil (psyllium) is appropriate for you, how to time it with your other medicines, and the right dose for your situation. If you think you may be experiencing a medical emergency, call your local emergency number immediately.
FAQs
1) What’s the best time to take Metamucil?
First, remember that consistency beats the clock. For regularity, take it at the time of day you’ll actually remember; then, give it 12–72 hours to show up in your routine (as covered earlier). Finally, stick with one slot for a few days before judging results.
2) Morning or night—does it actually matter?
In general, both can work. However, if you take it in the evening, leave about an hour before lying down and drink a full glass of water (as explained above). Meanwhile, mornings pair naturally with that first big glass of water.
3) Is it bad to take Metamucil right before bed?
Short answer: not ideal. Because your gut slows overnight and the fiber gels, it’s smarter to leave about an hour before you lie down. That way, you stay comfortable and still reap the benefits.
4) Should I take Metamucil before or after meals?
It depends on the job you want it to do. For satiety/portion control, take it 15–30 minutes before meals so the gel forms first; for cholesterol or general regularity, taking it with meals often makes consistency easier (as noted above). In short, match timing to your goal.
5) How long does Metamucil take to work?
Typically, bathroom regularity improves within 12–72 hours. For cholesterol, however, think in weeks—steady daily intake over ~3+ weeks is the realistic horizon we outlined earlier. So, be patient and keep the routine.
6) What’s the best time to take Metamucil for weight loss or appetite control?
For fullness, take it 15–30 minutes before the meals where you tend to overeat. That way, the gel is “ready” when food arrives. Also, start with one pre-meal dose daily, then add a second once your gut feels settled.
7) Can I take Metamucil every day?dl
Yes—daily use is common. That said, always follow your product’s serving directions, mix with a full 8 oz (≈240 ml) of liquid, and ramp up gradually if you’re new to fiber (as the label guidance above emphasizes). Over time, your gut usually adapts.
8) How many times a day can I take it?
Most labels allow up to three times daily as needed. Even so, begin low and go slow; then, increase only if you still need more support. Ultimately, let comfort guide the frequency.
9) How much should I take per day?
Serving sizes vary by product (powder, capsules, gummies). Start with the labeled serving, observe how you feel for a few days, and then—if LDL support is your target—work toward ~10 g/day (often split), as summarized earlier. Meanwhile, keep hydration steady.
10) Can I take Metamucil with my other medications?
Usually yes—just keep a 2-hour buffer (other meds two hours before or after your dose). This spacing helps avoid absorption issues mentioned above. When in doubt, ask your pharmacist.
11) Is Metamucil safe to take at night?
Yes—simply avoid right before bed. Leave about an hour, hydrate well, and you’re good. In practice, an after-dinner routine works nicely.
12) Does Metamucil help with diarrhea as well as constipation?
Interestingly, yes. Because it’s bulk-forming, it absorbs water and helps normalize stool consistency both ways (as the overview earlier explains). Therefore, it can be useful on either side of irregularity.
13) What if Metamucil makes me bloated or gassy?
Early on, that can happen. However, easing in, splitting the total into two smaller servings, and drinking extra water usually fixes it within a few days. If not, step back the dose and build again slowly.
14) Can I take Metamucil with vitamins or probiotics?
Generally, yes—just keep the 2-hour spacing to be safe. Moreover, if you take time-sensitive meds (like certain thyroid or diabetes drugs), confirm timing with your clinician or pharmacist. Better safe than sorry.
15) What’s the best way to take capsules?
Swallow them one at a time with a full glass of cool water. Otherwise, gulping a handful with a tiny sip risks discomfort. So, slow and steady wins here.
16) Can I mix Metamucil into yogurt, applesauce, or smoothies?
Prefer drinkable fluids you can consume right away. Because psyllium swells, thick foods aren’t ideal; plus, you want the gel forming in you, not in the cup. Therefore, mix, drink promptly, and then carry on.
17) How long should I keep taking Metamucil?
For regularity, use it as long as it helps and feels comfortable. For cholesterol, give it at least 3+ weeks of steady daily intake before you judge results. After that, reassess with your clinician if needed.
18) Does the time of day change Metamucil’s cholesterol effect?
Not meaningfully in available research. Instead, dose and consistency matter most. Consequently, pick times that ensure you actually hit your daily grams.
19) Is Metamucil safe in pregnancy?
Bulk-forming fibers have minimal systemic absorption and are generally considered compatible; nevertheless, confirm your plan with your own clinician. As always, your personal context matters.
20) What’s the best time to drink Metamucil for constipation?
Whenever you’ll remember—consistency beats the clock. To that end, pair it with a daily habit, drink at least 8 oz of liquid, and allow 12–72 hours (per the label guidance already covered).
21) Does Metamucil expire?
Yes—check the expiration date and store it as directed. And if you’re unsure, follow the packaging instructions you’ve already seen referenced.
22) Can I take Metamucil twice a day? Three times?
If your label allows, yes—many products permit up to three times daily. That said, don’t chase speed; instead, build gently and listen to your gut.
23) Is it okay to take Metamucil before bed if I drink extra water?
Even with extra water, it’s still wiser to leave about an hour before lying down. In the end, that small buffer keeps things comfortable and aligns with the bedtime caution above.
24) How soon before a meal should I take it for fullness but not discomfort?
A sweet spot for most people is about 20 minutes before eating. It’s long enough for the gel to start forming, but not so long that it thickens uncomfortably. Plus, it’s easy to remember.
25) If I miss a dose, should I double the next one?
No—just take the next scheduled dose. Doubling up isn’t necessary and can feel uncomfortable; instead, prioritize getting back to your normal rhythm.