Coffee is woven into the fabric of daily life for millions of women worldwide. Whether it’s a morning ritual or an afternoon pick-me-up, that cup of coffee offers a sense of comfort, alertness, and pleasure. But beneath the comforting aroma lies a complex biochemical interaction — one that’s often quite different for women compared to men.
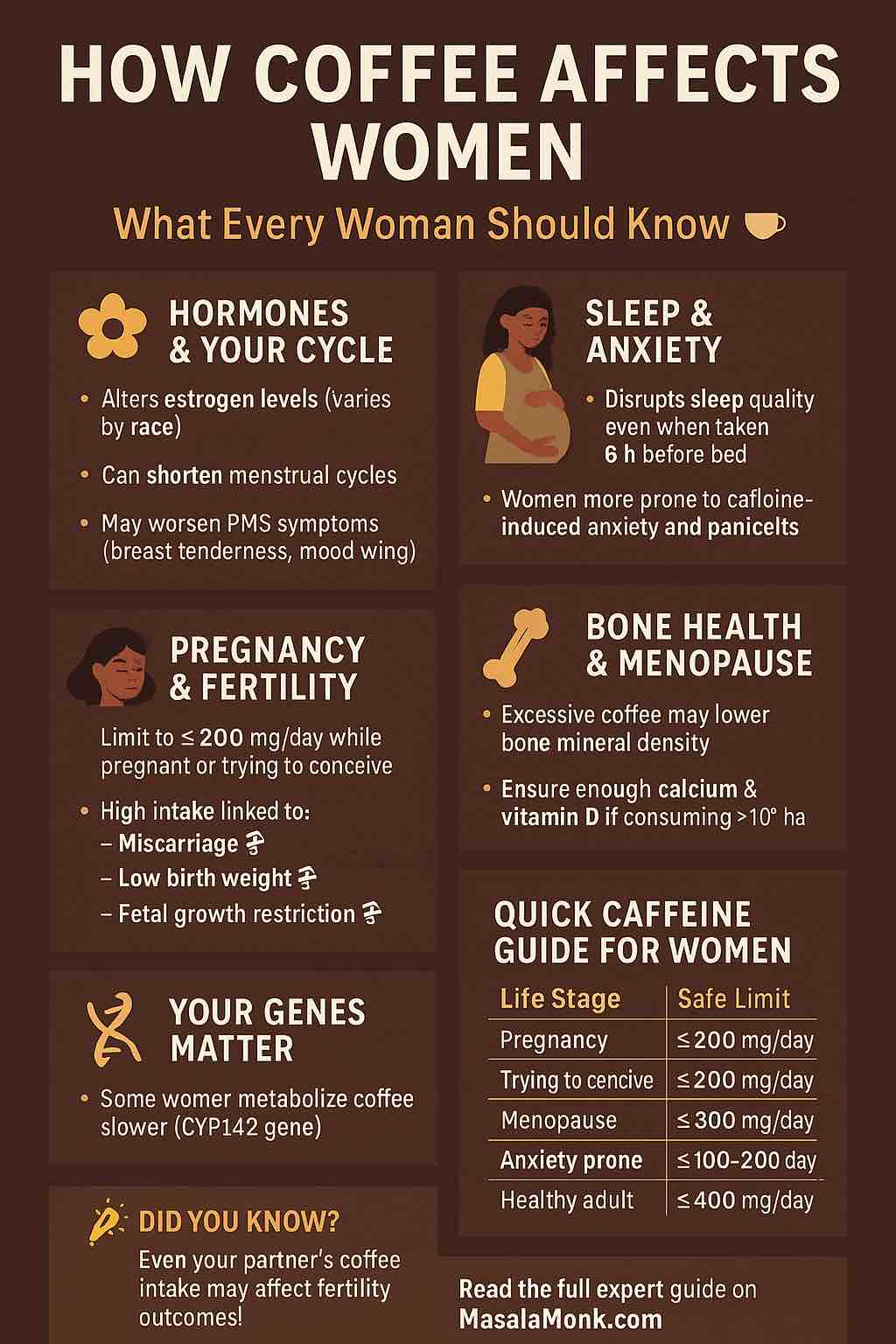
Emerging science has shown that caffeine interacts with women’s hormones, reproductive health, sleep, mental well-being, bone density, and more — sometimes in helpful ways, but sometimes not.
In this in-depth article, we’ll explore how caffeine affects women at every stage of life based on the latest available research.
☕ Caffeine 101: How It Works
Caffeine is a natural stimulant that primarily works by blocking adenosine receptors in the brain, which prevents drowsiness and promotes alertness. It also stimulates the central nervous system, increasing levels of dopamine, norepinephrine, cortisol, and adrenaline.
While caffeine metabolism occurs mainly in the liver via the CYP1A2 enzyme, not everyone processes it the same way. Factors such as sex hormones, genetics, pregnancy, contraceptive use, and racial differences significantly alter how caffeine is metabolized in women.
🌸 Hormonal Fluctuations & the Menstrual Cycle
Estrogen Interactions
- Caffeine’s relationship with estrogen is complex and ethnicity-dependent.
- White women may see a slight decrease in estrogen levels with caffeine consumption.
- Asian women may experience increased estrogen levels.
- These hormonal shifts can affect menstrual regularity, PMS symptoms, and even long-term reproductive health.
Menstrual Cycle Length and Symptoms
- High caffeine intake has been linked to:
- Shorter cycle lengths (fewer than 24 days).
- Possible reduced duration of menstrual bleeding.
- Exacerbation of PMS symptoms, such as breast tenderness, mood swings, and irritability.
- Increased likelihood of dysmenorrhea (painful periods) in some women.
Luteal Phase Sensitivity
- In the second half of the menstrual cycle (luteal phase), caffeine clearance may slow due to progesterone dominance.
- This can make women more sensitive to the stimulant effects of caffeine just before menstruation.
🤰 Fertility & Pregnancy
Trying to Conceive
- High caffeine intake (>300 mg/day) may:
- Prolong the time it takes to conceive.
- Potentially increase the risk of early pregnancy loss.
- Emerging data even suggests that male partners’ caffeine intake may affect miscarriage risk.
Pregnancy Risks
- Caffeine freely crosses the placenta.
- The fetus has limited ability to metabolize caffeine.
- Studies consistently show increased risks for:
- Miscarriage (with dose-dependent risk escalation).
- Fetal growth restriction and low birth weight.
- Stillbirth at very high caffeine intakes.
- The consensus recommendation:
➔ Limit caffeine to ≤200 mg/day during pregnancy.
😴 Caffeine, Sleep, and Anxiety
Women are often more vulnerable to the sleep-disrupting and anxiety-provoking effects of caffeine due to biological and hormonal differences.
Sleep Disturbance
- Caffeine can reduce total sleep time, diminish deep (slow-wave) sleep, and fragment REM sleep.
- Even when consumed up to 6 hours before bedtime, caffeine can delay sleep onset and reduce sleep quality.
- These effects may be amplified during PMS, pregnancy, and menopause when hormonal shifts alter sleep patterns.
Anxiety
- Women have higher rates of caffeine-induced anxiety and panic attacks, particularly at doses over 300 mg/day.
- Those with pre-existing generalized anxiety disorder or panic disorder are especially prone to caffeine-related exacerbations.
🦴 Bone Health and Osteoporosis
Postmenopausal women face increased risks for osteoporosis, and caffeine may worsen bone loss through:
- Reduced calcium absorption.
- Increased urinary calcium excretion.
- Accelerated bone demineralization at very high intakes.
However, moderate caffeine consumption (up to 300 mg/day) poses minimal risk if adequate calcium intake is maintained.
🧬 Genetic Differences in Caffeine Metabolism
Genetic variations in the CYP1A2 gene influence how quickly caffeine is metabolized:
- Fast metabolizers may tolerate higher intakes without adverse effects.
- Slow metabolizers retain caffeine longer, increasing risks for:
- Palpitations
- Anxiety
- Insomnia
- Hypertension
Women using oral contraceptives or hormone replacement therapy (HRT) also experience slower caffeine clearance, as estrogen suppresses CYP1A2 activity.
🩸 Caffeine and Chronic Female Conditions
Polycystic Ovary Syndrome (PCOS)
- Limited and conflicting data:
- Some studies suggest caffeine may improve insulin sensitivity (a benefit for PCOS).
- Others suggest it may worsen anxiety and hormonal imbalances.
Endometriosis
- Some observational data suggest high caffeine intake might worsen endometriosis symptoms, likely through hormonal dysregulation and increased inflammation.
Fibrocystic Breast Disease
- Caffeine can aggravate breast pain and tenderness in women with fibrocystic breast changes.
🩺 Cardiovascular Considerations
- Moderate coffee intake is generally not associated with increased cardiovascular disease risk.
- High caffeine intake can temporarily raise blood pressure and trigger palpitations, especially in sensitive women or those with pre-existing hypertension.
💡 The Ideal Caffeine Intake for Women (by Life Stage)
| Life Stage or Condition | Safe Upper Limit | Notes |
|---|---|---|
| General Adult Women | ≤ 400 mg/day | ~3-4 cups |
| Trying to Conceive | ≤ 200 mg/day | May benefit fertility |
| Pregnancy | ≤ 200 mg/day | Reduce miscarriage, stillbirth, growth restriction risk |
| Postmenopausal Women | ≤ 300 mg/day | Ensure adequate calcium intake |
| Anxiety Disorders | ≤ 100–200 mg/day | Minimize risk of anxiety/panic |
| Sleep Disorders | Avoid caffeine after noon | Prevent insomnia |
| PCOS / Endometriosis | Individualized | Consult healthcare provider |
🔬 Areas Where More Research Is Needed
While much is known, important research gaps remain:
- How caffeine interacts with racial and genetic differences.
- The precise effects on fertility and conception rates.
- Long-term effects on bone health and menopause.
- Deeper understanding of caffeine’s role in PCOS and endometriosis.
- Impacts of paternal caffeine intake on pregnancy outcomes.
✅ Bottom Line
Caffeine can absolutely be part of a woman’s healthy lifestyle — but context matters greatly. Hormonal status, life stage, personal sensitivity, and overall health conditions all influence how caffeine behaves in the female body.
For most women, moderation remains key:
- Pregnant or trying-to-conceive? Keep it under 200 mg/day.
- Menopausal? Stay aware of bone health and calcium.
- Struggle with anxiety or sleep? Consider lowering caffeine intake.
- Otherwise healthy? Most can enjoy 200–300 mg/day safely.
Being mindful of your individual response — and adjusting intake accordingly — allows you to enjoy your coffee without compromising your health.
Always speak to your healthcare provider for personalized advice, especially during pregnancy or while managing chronic conditions.
10 FAQs About Coffee and Women’s Health
1️⃣ Is coffee safe for women to drink daily?
Yes, for most healthy adult women, moderate coffee consumption (200–300 mg caffeine per day, about 2–3 cups) is considered safe. Individual tolerance varies based on genetics, hormones, and health conditions.
2️⃣ Does caffeine affect women’s hormones?
Yes. Caffeine may influence estrogen levels, menstrual cycle length, PMS symptoms, and hormonal fluctuations. The effect can differ by ethnicity and life stage, with some studies showing elevated estrogen levels in Asian women and slightly decreased levels in White women.
3️⃣ Can coffee affect fertility or the ability to get pregnant?
High caffeine intake (>300 mg/day) may prolong time to conception and slightly increase the risk of miscarriage. Both partners may benefit from limiting caffeine to ≤200 mg/day while trying to conceive.
4️⃣ How much coffee is safe during pregnancy?
Most guidelines recommend pregnant women limit caffeine to 200 mg per day or less to minimize risks of miscarriage, low birth weight, and fetal growth issues.
5️⃣ Does caffeine worsen PMS symptoms?
For some women, yes. Caffeine may exacerbate PMS symptoms like breast tenderness, irritability, and mood swings, particularly in sensitive individuals or at higher doses.
6️⃣ Can caffeine cause anxiety in women?
Yes. Women tend to be more sensitive to caffeine-induced anxiety and panic attacks, especially when consuming over 300 mg/day. Those with pre-existing anxiety disorders should monitor intake closely.
7️⃣ Is caffeine harmful for women in menopause?
Postmenopausal women can generally consume caffeine safely, but high intake may contribute to reduced bone mineral density. Adequate calcium and vitamin D intake can help mitigate bone loss risks.
8️⃣ Does caffeine interact with birth control or hormone replacement therapy (HRT)?
Yes. Estrogen from birth control or HRT slows caffeine metabolism, making its effects last longer. Women on these medications may experience prolonged stimulation from typical caffeine doses.
9️⃣ Is coffee helpful or harmful for women with PCOS?
Research is mixed. Some studies suggest caffeine may improve insulin sensitivity (beneficial for PCOS), while others note potential drawbacks like increased anxiety and hormonal fluctuations. Individual response should guide intake.
🔟 When should women avoid caffeine entirely?
Women may benefit from avoiding caffeine:
- Late in pregnancy
- If experiencing insomnia or sleep issues
- If prone to severe anxiety
- If advised by a healthcare provider for specific medical conditions













