When people type “green tea erectile dysfunction” into a search bar, they’re usually after two things: a straight answer and a practical plan. Fortunately, we can offer both. In brief, green tea isn’t a stand-alone cure for ED; nevertheless, it can support the underlying physiology that erections depend on—namely, vascular health and nitric-oxide signaling. As you’ll see, the science is strongest around blood-vessel function, and, when paired with sensible lifestyle steps, a consistent green-tea habit becomes a low-friction way to help the system that powers sexual performance.
Before anything else, it helps to remember what an erection actually is: a coordinated vascular event. Arteries must dilate on cue, endothelial cells need to produce nitric oxide in the moment, and smooth muscle has to relax so blood can enter and remain. Interestingly, green tea is rich in catechins (especially EGCG) that repeatedly show benefits for endothelial function—the same system. In fact, in a controlled study of smokers, two weeks of green tea increased flow-mediated dilation (FMD), a standard ultrasound measure of how well arteries expand; that improvement doesn’t prove a direct ED fix, yet it does strengthen the biologic plausibility behind green tea for ED as supportive care (green tea reversed endothelial dysfunction in smokers).
Does green tea help erectile dysfunction—or is that wishful thinking?
Put simply: yes, as vascular support; no, as a magic bullet. Mechanistically, catechins reduce oxidative stress, calm inflammatory signaling, and enhance eNOS activity to raise nitric-oxide availability. Crucially, those aren’t just test-tube effects. In tightly designed human studies, both acute and short-term green-tea intake improved FMD in groups with impaired endothelial function—again, the same pathway erections rely on (acute FMD improvement after green tea). Consequently, while no randomized trial shows green tea single-handedly “curing” ED, the physiologic alignment is real, relevant, and actionable.
Moreover, ED rarely has a single cause. Sleep debt, chronic stress, blood pressure, and metabolic health all push in either direction. Because of that, many readers pair daytime tea with evening routines that protect rest and dial down sympathetic overdrive. For complementary, lifestyle-friendly context you can integrate gently, see our on-site pieces like clove-infused tea for erectile dysfunction and the companion guide to enhancing intimacy with clove-infused massage. Those ideas don’t replace care; nevertheless, they often make a routine more human and sustainable.
Green tea for ED: where the signal is strongest—and where we should be cautious
First, the human vascular signal is consistent: brewed green tea improves FMD in settings of endothelial dysfunction, and that matters because endothelial health is upstream of erection quality. Second, preclinical data—for example, in diabetic or aged animals—often show EGCG preserving cavernosal smooth muscle and improving erectile physiology; informative, yes, though we should avoid over-extrapolating. Third, direct ED outcomes in humans after a green-tea intervention remain under-studied; hence, we position green tea as a supportive habit, not a replacement for guideline-based therapies.
Does green tea cause erectile dysfunction?
Short answer: there’s no evidence it does. If anything, broader caffeine research points the other way. In a large U.S. dataset, men consuming roughly 170–375 mg/day of caffeine had lower odds of prevalent ED than very-low consumers after adjusting for common confounders—an association, not proof, but reassuring nonetheless (NHANES analysis on caffeine and ED). Furthermore, more recent genetic work designed to probe causality has not supported a harmful link between habitual coffee/caffeine intake and ED risk. In other words, moderate caffeine—like what you’d get from a few cups of tea spread intelligently through the day—does not appear to be an ED villain.
Naturally, personal tolerance still matters. Overshooting your own caffeine ceiling can nudge anxiety up and sleep down; paradoxically, that will worsen performance for many people. Therefore, keeping most of your tea earlier in the day, then switching to calming, caffeine-free options in the evening, tends to balance the equation.
Matcha vs brewed tea in a green tea for erectile dysfunction routine
At first glance, the choice between matcha and brewed green tea seems cosmetic; however, it meaningfully changes catechin exposure. Because matcha is powdered whole leaf whisked into water, you ingest more of the plant per cup, often translating to higher catechin intake. That’s why some readers lean on matcha when focusing closely on green tea erectile dysfunction strategies. Nevertheless, matcha also delivers more caffeine per serving, which is terrific before a midday walk or workout but not ideal late at night.
Even so, there’s another wrinkle worth noting: several vascular studies that showed FMD improvements used brewed tea, not isolated EGCG capsules—suggesting the whole-tea matrix (minor polyphenols, L-theanine, and other constituents) may be important (overview of endothelial benefits with brewed tea). Consequently, there’s no need to chase megadoses or fancy extracts. A steady rhythm of well-brewed cups captures most of what you’re after.
Green tea in erectile dysfunction routine: timing, brewing, and iron-savvy habits
Adherence hinges on simplicity. Accordingly, try a routine that slides into ordinary life:
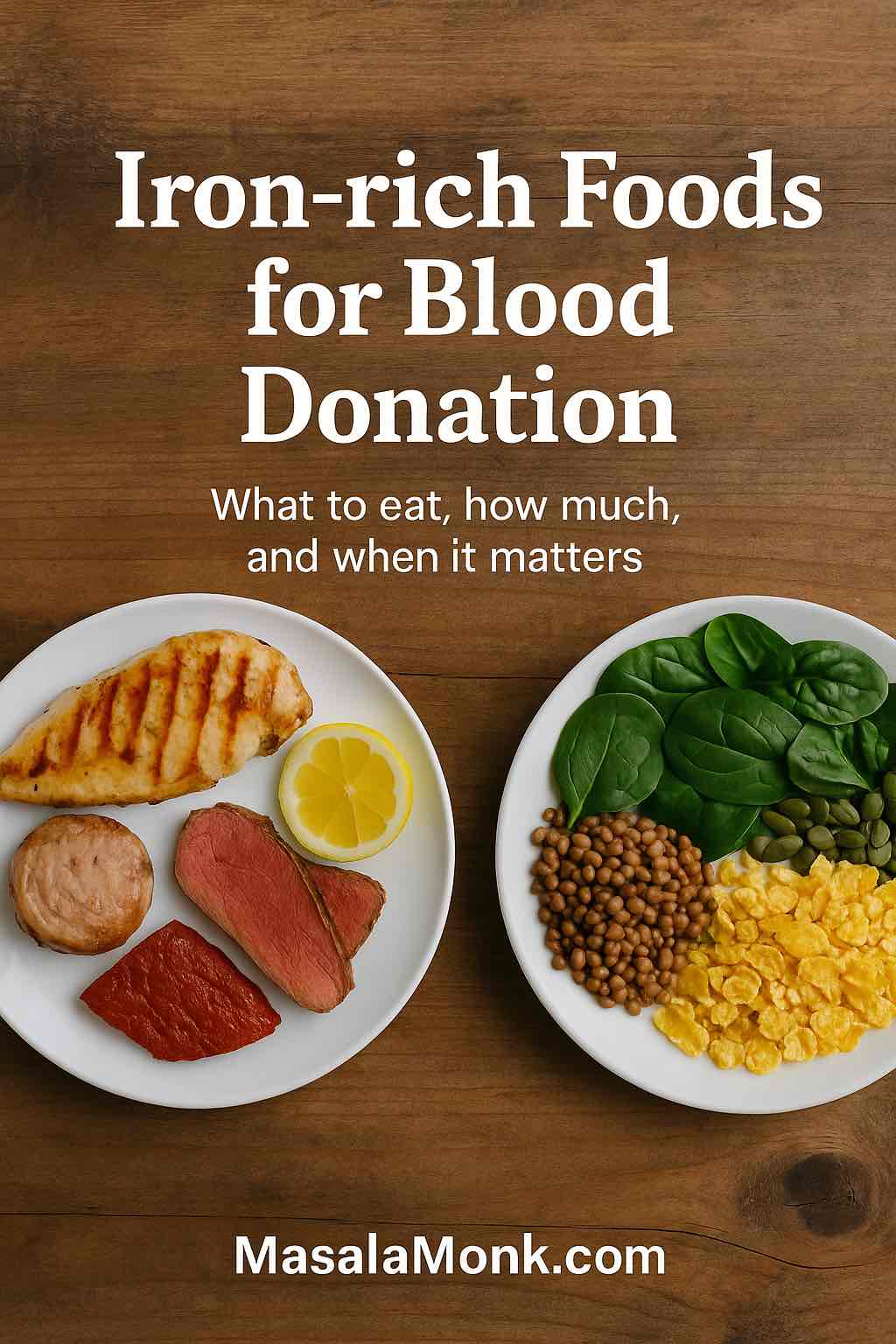
- Morning: brew one cup with water around 75–85°C; steep 2–3 minutes, then taste and remove leaves. Use roughly 2 g tea leaves (about a teaspoon) per 250 ml cup. Because tea polyphenols can blunt non-heme iron absorption, drink your cup between meals, not with an iron-rich breakfast (classic research on tea and iron absorption).
- Early afternoon: enjoy a second brewed cup—or whisk a small bowl of matcha—especially before a brisk walk or short resistance session. The slight stimulation often improves mood and training adherence, both of which indirectly benefit sexual health.
- Evening: pivot to caffeine-free comfort so sleep can do its quiet work. For ideas that connect relaxation, scent, and touch (without stimulants), have a look at enhancing intimacy with clove-infused massage and the companion clove-infused tea piece. Both are gentle, sensory ways to reduce tension—the sort of context erections actually appreciate.
Just as importantly, build iron awareness into your habit. If you’re vegetarian, an endurance athlete, or someone with marginal ferritin, separate tea and main meals by an hour or two. When convenient, pair plant-based iron sources with vitamin C (think lemon over greens or a citrusy salad) to offset tea’s inhibitory effect. These small timing tweaks allow you to keep your green tea for ED routine without nudging iron status the wrong way.
Also Read: Iron Deficiency Anemia Symptoms: 15 Signs You Are Iron Deficient
Safety first: the nadolol interaction, plainly explained
Most people tolerate green tea well; still, one clinically documented interaction deserves a spotlight. In a carefully executed study, repeated green-tea intake caused an approximately 80% reduction in nadolol exposure, likely by inhibiting OATP1A2 transport in the gut—an effect that can blunt the drug’s blood-pressure benefits. If you take nadolol for hypertension or heart rhythm, don’t guess; speak with your clinician about tea timing and total intake to avoid under-treating your condition (green tea markedly lowers nadolol exposure). This is not theoretical; it’s been measured.
Beyond that, common-sense cautions apply: if caffeinated tea worsens reflux or sleep, dial the timing earlier; if you’re iron-deficient, prioritize recovery first, then re-introduce tea with smart spacing; and if you live with complex medical issues, a brief conversation with your care team is never wasted.
Green tea for erectile dysfunction meets the rest of your life: stacking gentle companions
Because ED is usually a multifactorial pattern rather than a single-switch problem, readers often stack tea with other low-risk, context-wise choices. We’ve written several practical, non-gimmicky pieces you can thread into your evenings or weekends:
- For a warm, aromatic option that feels winter-friendly and ritual-rich, read our guide to clove-infused tea for erectile dysfunction.
- To bring touch and presence back into the mix—without numbing creams or edgy supplements—try the step-by-step clove-infused massage for erectile dysfunction relief.
- If you’re curious about botanicals with a longer cultural history, our roundup on saffron as an aphrodisiac explores dosing ranges used in research and, importantly, sets realistic expectations.
- Meanwhile, for men who enjoy culinary-to-intimacy crossovers, the explainer on cardamom benefits for men connects circulation-leaning spices with daily habits in a balanced, non-hyped way.
- And because sensual context matters as much as chemistry, our practical overview of best oils for erectile dysfunction (ED) translates scent, warmth, and massage into routines that couples actually keep—no unrealistic promises, just simple practices that lower friction and build momentum.
None of these are “musts.” Nevertheless, they make it easier to keep a routine going, which is usually what separates good intentions from tangible change.
Green tea erectile dysfunction: what about stamina, libido, and energy?
Here’s where nuance helps. People sometimes expect a single beverage to change stamina on contact. Realistically, indirect pathways matter more. Moderate caffeine can heighten alertness, smooth effort during workouts, and improve subjective energy—effects that compound across weeks into better mood, better fitness, and better blood-pressure control. Those are all upstream of better erections. At the same time, overshooting your personal tolerance invites a different story: racing thoughts, restless nights, and next-day irritability, none of which help. Thus, a smart green tea for ED pattern spreads cups earlier, keeps evenings quiet, and protects sleep as the ultimate performance enhancer.
Additionally, green tea’s L-theanine likely softens the feel of caffeine, producing a calmer focus than coffee for many people. That qualitative difference is hard to quantify in trials, but countless readers notice it. From a practical standpoint, if your mornings feel smoother on tea than coffee, lean into the thing you’ll actually sustain.
Brewing for benefits without getting precious
Although catechins deserve attention, brew method quietly decides whether you will enjoy your cup enough to drink it daily. Fortunately, you don’t need gadgets. Heat water just below a boil, aiming for 75–85°C; measure roughly 2 g of leaves per 250 ml cup; steep 2–3 minutes and taste. If you prefer matcha, whisk 1–2 g into hot (not boiling) water until lightly frothy, then sit for a moment—literally—before sipping. The brief pause isn’t fluff; slowing down cues your parasympathetic system, which blends seamlessly with the intimacy-supporting direction of everything else we’ve discussed.
As for timing, keep your iron guardrails in mind. Drinking tea between meals usually solves the absorption issue for most people, while a squeeze of lemon over greens or beans at lunch helps your body capture more plant-based iron despite tea’s polyphenols. With those small adjustments, your green tea erectile dysfunction routine becomes both safe and pleasantly habitual.
Bringing it all together—so you know exactly what to do next
Taken as a whole, the evidence points toward a grounded, hopeful conclusion: green tea supports the vascular foundation of erectile function, even though it does not—and should not be sold as—a cure for ED. Therefore, the smartest approach is both modest and consistent:
- Adopt a daily rhythm of 1–2 brewed cups earlier in the day; add a small matcha serving when you want an extra nudge.
- Brew well, not long: 75–85°C water, 2–3 minutes, then remove the leaves.
- Mind iron by separating tea from meals, especially if you’re vegetarian or have borderline ferritin.
- Protect sleep by switching to caffeine-free, sensory routines in the evening; for ideas that combine warmth, scent, and touch, explore clove-infused tea and clove-guided massage.
- Check medications, particularly nadolol, with your clinician so tea doesn’t undermine treatment (green tea–nadolol interaction explained).
- Give it weeks, not days; meanwhile, address the basics—movement, blood pressure, stress, and intimacy cues—because erections follow the health of your cardiovascular system.
Lastly, if you want to widen the lens without spinning into hype, our on-site resources round out the picture gracefully: browse the thoughtfully skeptical best oils for ED guide, skim the culinary-meets-intimacy angle in cardamom benefits for men, or, when you feel curious, dip into saffron as an aphrodisiac for a balanced take on a classic botanical. None of these pieces promise miracles; instead, they offer workable layers that play nicely with a daily green tea erectile dysfunction habit—precisely the sort of ecological approach that tends to produce steady, real-world gains.
FAQs
1) Does green tea help erectile dysfunction?
In brief, green tea can support erectile function by improving blood-vessel health and nitric-oxide availability; however, it isn’t a stand-alone ED cure. For most readers, making green tea for ED a steady habit works best alongside sleep, exercise, and medical advice when needed.
2) Is green tea good for ED on a daily basis?
On balance, yes—daily green tea for ED is reasonable. Moderate intake (2–3 cups earlier in the day) tends to aid vascular tone while keeping caffeine side effects in check.
3) Can green tea cause erectile dysfunction?
For clarity, there’s no solid evidence that green tea causes ED. Typically, moderate tea intake fits comfortably within a heart-healthy routine that supports erection pathways rather than harming them.
4) Does green tea make you last longer in bed?
In reality, no direct trials prove stamina benefits. Still, many find that better vascular function, improved mood, and consistent training—habits often paired with a green tea erectile dysfunction routine—can indirectly help performance.
5) Which tea is good for erectile dysfunction besides green tea?
Notably, some choose ginseng tea or pomegranate/hibiscus infusions as adjuncts. Even so, green tea for ED remains the most researched option for vascular support, so start there and layer others cautiously.
6) What’s the best way to brew green tea for ED benefits?
Importantly, use water around 75–85°C, steep 2–3 minutes, and taste before over-extracting. This preserves catechins while keeping bitterness low—making a green tea erectile dysfunction habit easier to sustain.
7) How much green tea should I drink for erectile function?
As a rule, 2–3 cups per day is a practical target. All told, consistency matters more than chasing high doses; let your body’s caffeine tolerance guide timing.
8) Is matcha better than regular green tea for ED?
By contrast, matcha often delivers more catechins per serving, which some people prefer for a focused matcha green tea erectile dysfunction plan. At the same time, matcha also contains more caffeine, so keep it earlier in the day.
9) Does green tea boost libido directly?
Ultimately, libido is multifactorial. Green tea for ED mainly supports circulation and may steady energy and mood; it doesn’t act as a classic aphrodisiac for everyone.
10) Can I drink green tea at night if I have ED?
For most, evening caffeine can disrupt sleep—an ED antagonist. Therefore, keep green tea erectile dysfunction cups earlier, and choose caffeine-free options later to protect recovery.
11) Will green tea interact with ED medications or heart drugs?
Crucially, green tea can reduce absorption of nadolol, a beta-blocker; discuss timing with your clinician. As needed, review all meds with a professional before locking in a green tea for ED routine.
12) Does green tea affect testosterone?
Meanwhile, typical intakes show no meaningful testosterone changes in healthy adults. The benefit of green tea for ED comes from vascular effects rather than hormone boosts.
13) Can green tea improve blood flow to help erections quickly?
Sometimes, yes—acute improvements in endothelial function have been observed after tea intake. Still, green tea erectile dysfunction routines work best over weeks, not hours.
14) What about side effects of green tea for ED?
Altogether, side effects are uncommon at moderate doses. That said, sensitive individuals may notice jitters, reflux, or sleep disruption; adjust timing—or choose lower-caffeine varieties—while keeping the green tea for ED plan intact.
15) Does tea reduce iron absorption and affect ED indirectly?
Indeed, polyphenols can inhibit non-heme iron absorption. To stay safe, drink green tea for ED between meals, particularly if you’re vegetarian or have low ferritin.
16) Is decaf green tea useful for erectile dysfunction?
Even without much caffeine, decaf green tea retains many catechins. Consequently, it can still complement a green tea erectile dysfunction approach—especially for evening cups.
17) How long until I notice benefits from a green tea ED routine?
Typically, readers report subtle changes within a few weeks as overall cardiovascular habits improve. Nevertheless, persistent ED warrants medical evaluation—tea is a helper, not a replacement.
18) Can I combine green tea for ED with exercise and weight management?
Absolutely. In practice, green tea erectile dysfunction strategies pair well with brisk walks, resistance training, and blood-pressure control—each reinforcing the others for better outcomes.
19) Are there specific foods to pair or avoid with green tea for ED?
Preferably, separate tea from iron-rich meals by an hour or two. Conversely, pair plant-based iron with vitamin C at mealtimes, then enjoy green tea for ED mid-morning or mid-afternoon.
20) What if anxiety contributes to my ED—will green tea help?
At times, yes: many find tea’s gentler caffeine-theanine profile less jangly than coffee. However, if anxiety remains high, shift green tea erectile dysfunction cups earlier and emphasize relaxation practices at night.
21) Is “tea for ED” different from “green tea for ED”?
Functionally, tea for ED is a broad phrase; nonetheless, green tea for ED is specific to catechin-rich Camellia sinensis. Start there, then evaluate other teas as supportive extras, not substitutes.
22) Can green tea improve morning erections?
Possibly, over time. As cardiovascular health settles, some notice stronger green tea and erection patterns in the morning. Even so, individual responses vary; keep expectations realistic.
23) Will switching from coffee to green tea help my ED?
Often, yes. Some feel steadier energy and better sleep quality after switching, which indirectly benefits erections. Try replacing one coffee with green tea for ED first, then reassess.
24) Is there a best time to drink green tea for ED results?
Preferably, earlier in the day—morning and early afternoon—so you gain vascular support without disturbing sleep. That timing keeps a green tea erectile dysfunction plan sustainable.
25) Should I choose loose-leaf or tea bags for ED support?
Either works if quality is high. Nevertheless, loose-leaf often tastes better and encourages proper brewing—making a green tea for ED habit easier to maintain day after day.