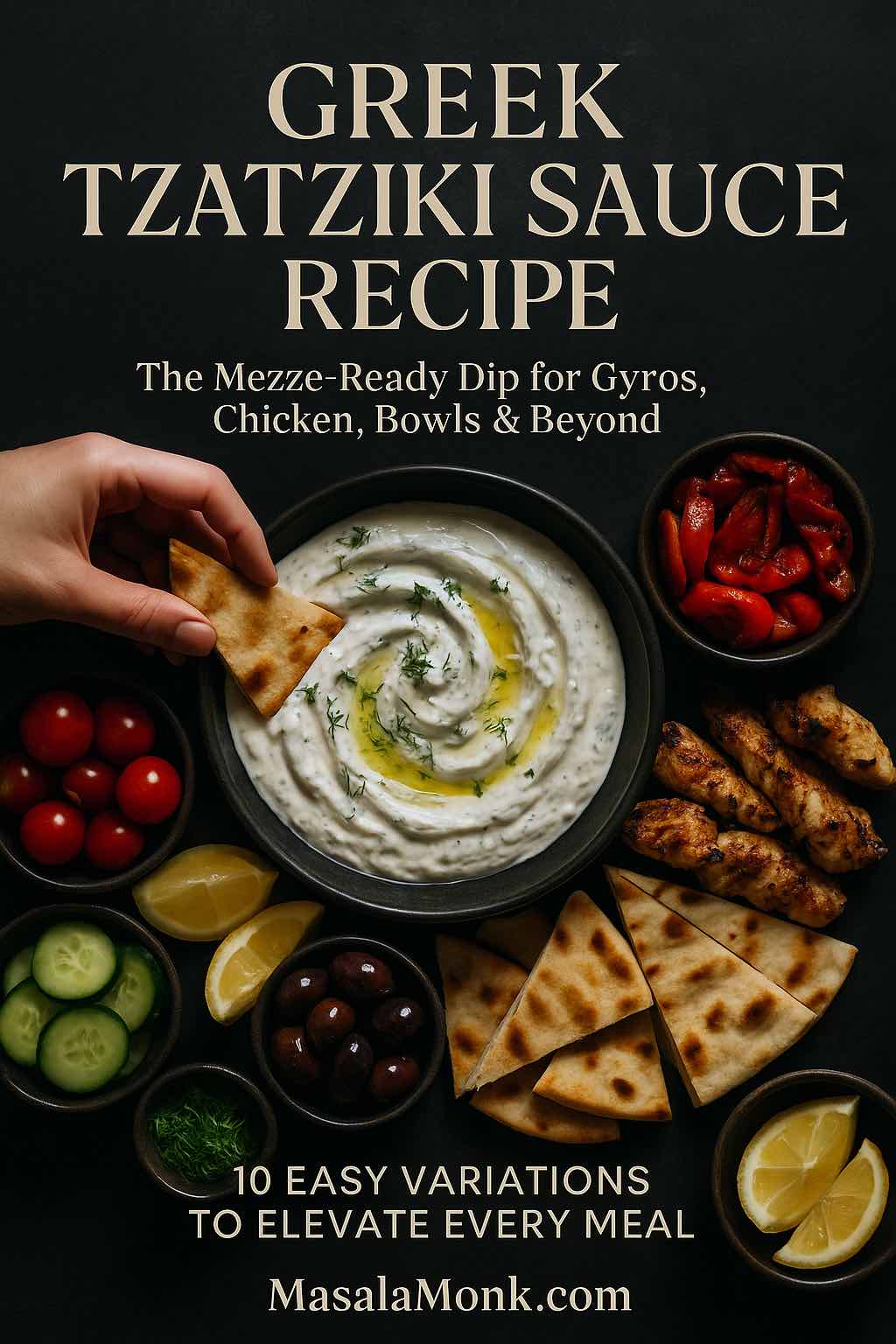
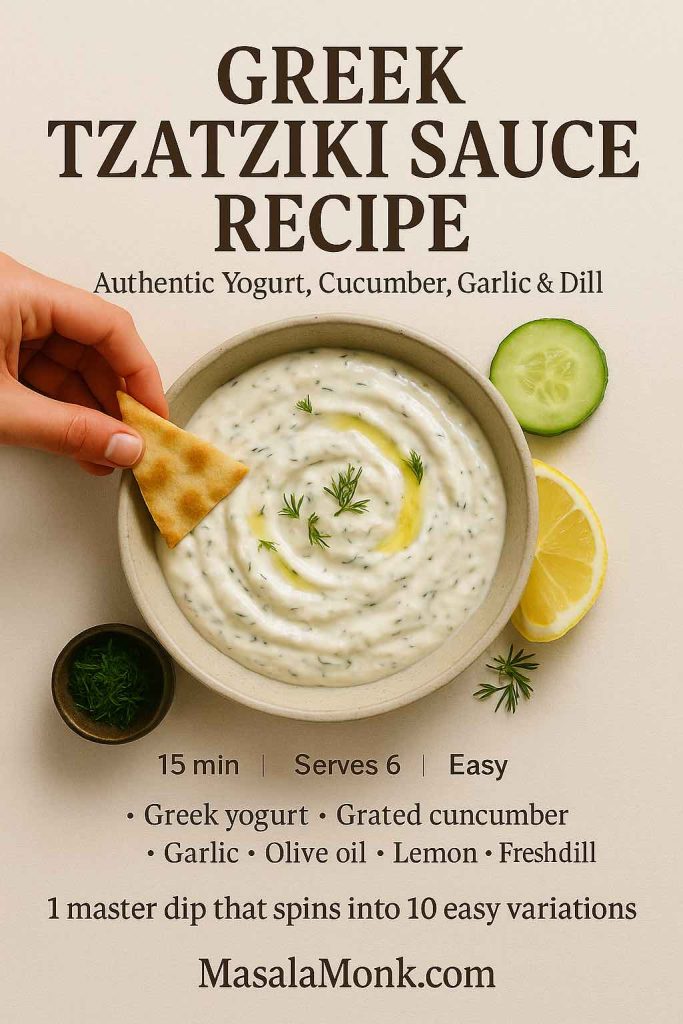
There are recipes you make once, and then there are recipes that quietly move into your weekly rhythm. A good Greek tzatziki sauce recipe almost always falls into the second category. It’s cool and creamy, yet bright and garlicky; simple to stir together, but endlessly useful. One bowl can turn raw vegetables into a snack, plain chicken into dinner, or a random collection of leftovers into a mezze-style feast.
In this long guide, you’ll walk through:
- What tzatziki actually is (and what makes it “Greek”)
- A master Greek tzatziki sauce recipe you can rely on
- Ingredient notes so your sauce tastes restaurant-good, not just “fine”
- Ten easy variations built off that master bowl
- Ideas for turning tzatziki into full meals, from mezze boards to brunch
- Practical notes on storage and making it fit a Mediterranean-style way of eating
All of it is meant to be cooked and eaten, not just admired on a screen.
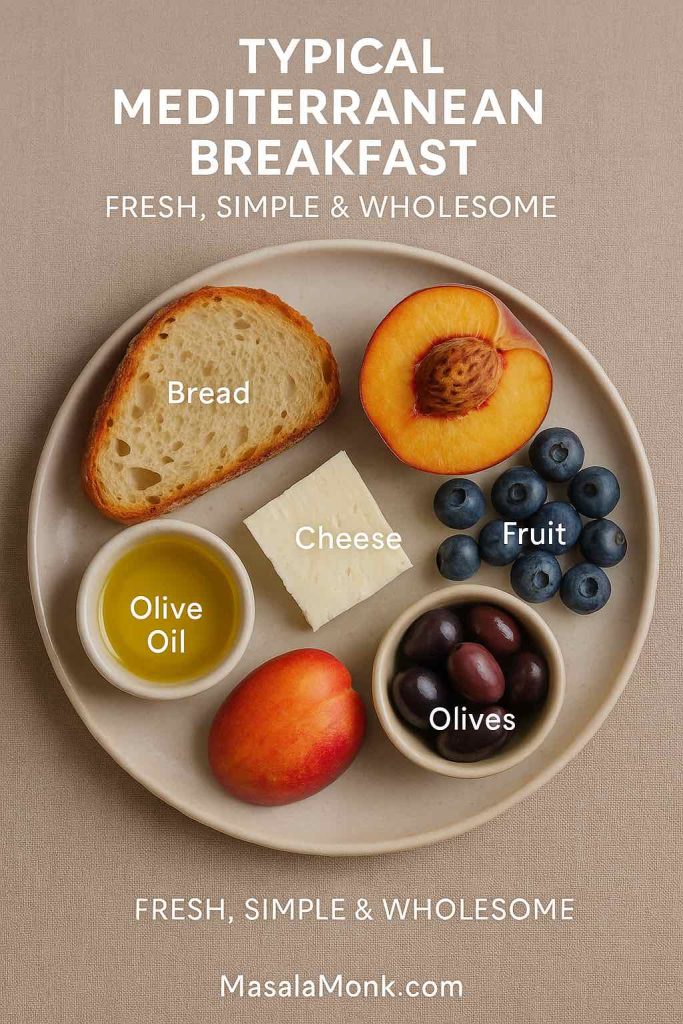
What Is Tzatziki?
Tzatziki is a chilled yogurt and cucumber sauce that shows up all over Greek and Eastern Mediterranean tables. Read more about it on Wikipedia. At its core, it’s simply:
- Thick strained yogurt
- Grated cucumber
- Garlic
- Olive oil
- A little acid (lemon or vinegar)
- Herbs like dill or mint
- Salt and pepper
Most traditional versions of a Greek tzatziki sauce recipe follow the same pattern. You grate the cucumber, salt it and squeeze out the water; stir it into thick yogurt with garlic, olive oil and herbs; and let everything chill so the flavors settle and mellow. This basic method pops up again and again in classic Greek and Mediterranean recipes.
Although every family and restaurant has its own tweaks—some go heavy on mint, others prefer all dill, and some include a splash of red wine vinegar instead of lemon—the balance is always the same: refreshing, tangy, garlicky and creamy without being heavy.
At the same time, tzatziki sits naturally inside a broader Mediterranean way of eating. That style emphasizes vegetables, legumes, whole grains, nuts, olive oil and modest amounts of animal protein, with fermented dairy like yogurt appearing in small but regular amounts. Large reviews and long-term studies link this overall pattern with better heart health, improved blood sugar control and even longer life.
So when you stir together a bowl of tzatziki, you’re not just making “a dip for pita.” You’re putting together a flexible, lighter-feeling sauce that pairs effortlessly with vegetables, grains and lean proteins—exactly the kind of food many people are trying to eat more of anyway.
Also Read: How to Make Churros (Authentic + Easy Recipe)
Ingredients for the Master Greek Tzatziki Sauce Recipe
Before you start grating and whisking, it helps to spend a moment on the ingredients themselves. The list is short, so each piece matters.
Greek Yogurt
A true Greek tzatziki sauce recipe needs thick, strained yogurt. That’s where Greek yogurt comes in. Because it’s been strained to remove much of the whey, Greek yogurt is denser and naturally higher in protein than regular yogurt. Nutrition guides repeatedly point out that this straining concentrates protein, calcium and probiotics into each spoonful.
A few practical notes:
- Choose plain, unsweetened Greek yogurt. Any sweetness will clash with the garlic and cucumber.
- Full-fat gives the most luxurious texture, but 2% still works beautifully and feels a bit lighter.
- If you can’t find Greek yogurt, you can strain regular yogurt in a cheesecloth-lined strainer for a couple of hours in the fridge.
If Greek yogurt is already part of your routine—maybe in breakfasts like high protein overnight oats—tzatziki is simply another way to make the same staple pull double duty.
Cucumber
Cucumber brings that signature freshness and bite. You can use:
- English (seedless) cucumbers, which have thin skins and fewer seeds
- Or regular cucumbers, peeled if the skin is thick or waxed
What matters more than the variety is how you treat it. Grating releases water, and unless you squeeze that water out, your Greek tzatziki sauce recipe will start thick and end up runny. Salting and squeezing the cucumber is the small step that turns “good enough” tzatziki into the kind you keep going back to.
Garlic
Fresh garlic is non-negotiable. It’s what stops tzatziki from tasting like plain cucumber yogurt. Mince it very finely, or grate it on a microplane so there are no sharp bits. Raw garlic is strong—especially as it sits in the fridge and infuses the yogurt—so starting with a little less than you think you need is usually wise. You can always add more next time.
Olive Oil
Extra-virgin olive oil adds depth, body and that lovely sheen on top of the finished sauce. It also reminds your palate that you’re in Mediterranean territory. A couple of tablespoons are enough; you want richness, not an oil slick.
Lemon Juice or Vinegar
Acid lifts the flavor. Lemon juice is the most common choice, though wine vinegar or even a mild apple cider vinegar can be used. Add it gradually and taste as you go. You’re looking for bright and tangy, not sour.
Herbs: Dill and Mint
Fresh dill is the classic herb in a Greek tzatziki sauce recipe, although many cooks add mint or swap it in completely. Dill reads as savory and grassy; mint adds a cool, almost sweet edge. Either works. You can even use a mix, especially if you’re serving the sauce with grilled lamb, chicken or eggplant.
Salt and Pepper
Salt is what knits all these pieces together. It seasons the yogurt, pulls moisture from the cucumber and softens the sharp edges of the garlic. Freshly ground black pepper isn’t mandatory, but a small pinch adds a gentle warmth.
Also Read: Béchamel Sauce for Lasagna: Classic, Vegan & Ricotta Sauce Recipe
Master Greek Tzatziki Sauce Recipe (Step by Step)
This is the anchor recipe you can make with your eyes closed once you’ve done it a few times. Every variation later on will start from this bowl.
Ingredients (Makes About 1½ Cups)
- 1 cup full-fat plain Greek yogurt
- ½ large cucumber (or 1 small), coarsely grated
- 2–3 cloves garlic, very finely minced or grated
- 2 tbsp extra virgin olive oil
- 1–2 tbsp fresh lemon juice, to taste
- 2 tbsp finely chopped fresh dill (or 1 tbsp dill + 1 tbsp mint)
- ½ tsp fine sea salt, plus more to taste
- A pinch of freshly ground black pepper
- 1–2 tbsp cold water or reserved cucumber juice, if needed
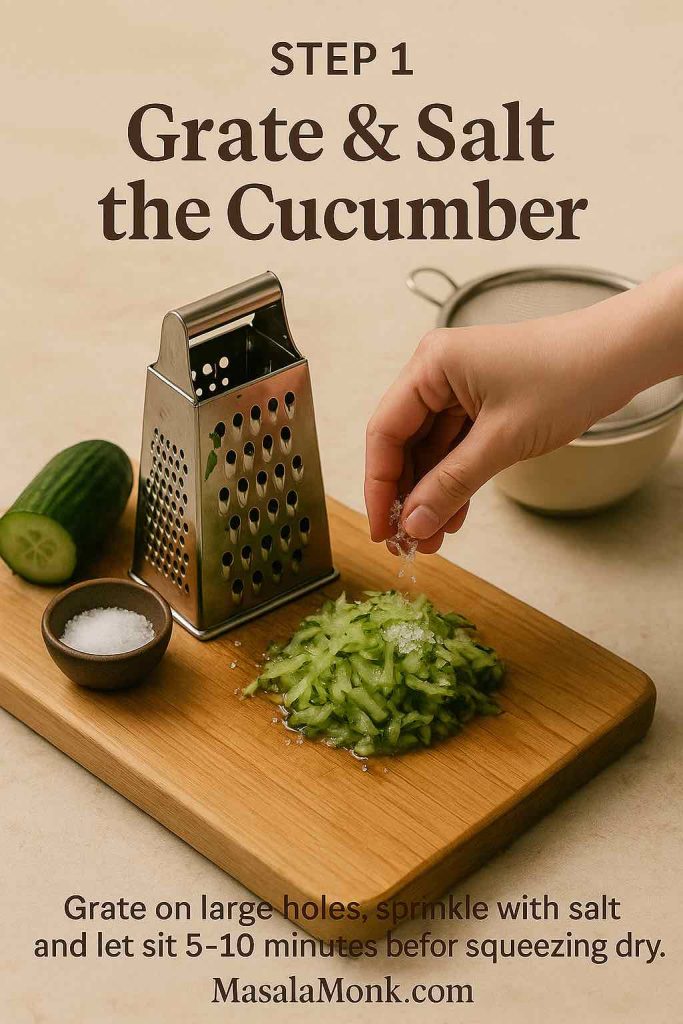
Step 1: Grate and Salt the Cucumber
Start by grating the cucumber on the large holes of a box grater. If you’re using a thick-skinned or waxed cucumber, peel it first; otherwise, leave the skin on for extra color and nutrients.
Once it’s grated:
- Toss the cucumber with a pinch of salt.
- Place it in a fine-mesh strainer over a bowl.
- Let it sit for 5–10 minutes, then squeeze it firmly with your hands or a clean towel until it feels quite dry.
It’s tempting to rush this step, but taking an extra minute here pays off later. Think of how well-drained spinach makes a better spinach dip; cucumber behaves the same way.
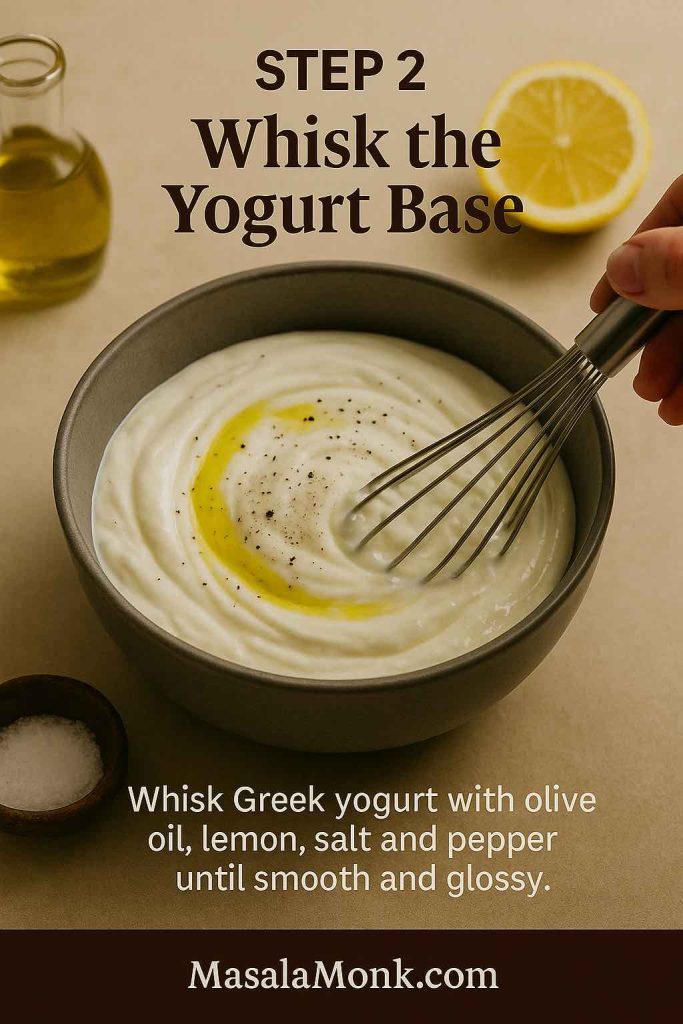
Step 2: Build the Yogurt Base
In a medium bowl, whisk together:
- The Greek yogurt
- Olive oil
- 1 tablespoon of lemon juice
- The ½ teaspoon of salt
- A pinch of black pepper
Whisk until the mixture is smooth and glossy. The olive oil will loosen the yogurt slightly and give it a silky finish.
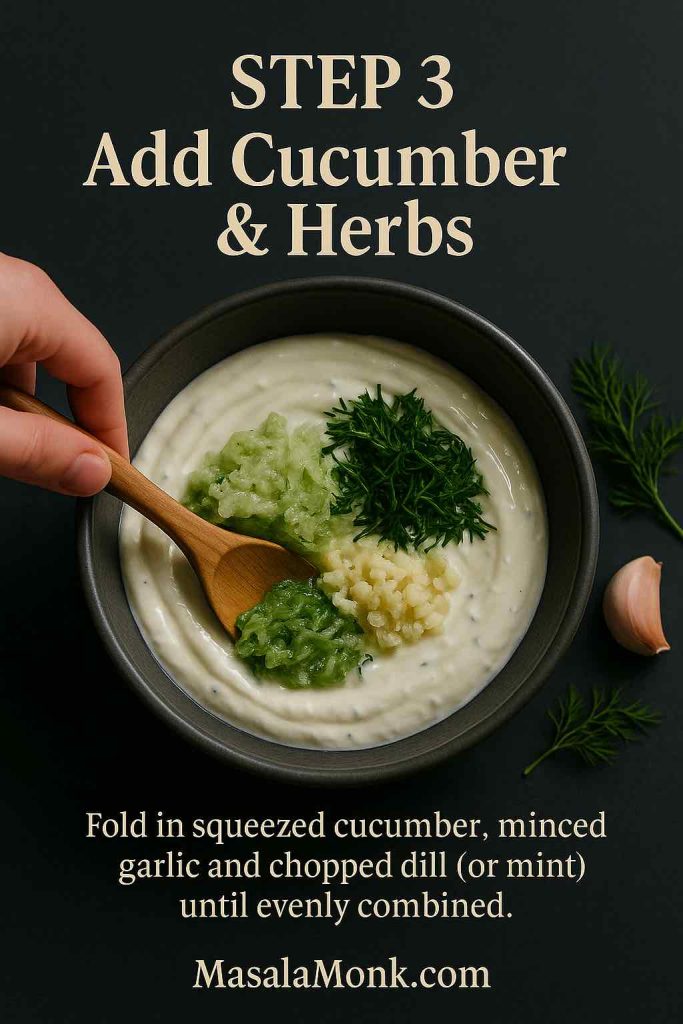
Step 3: Add Garlic, Cucumber and Herbs
Fold in:
- The squeezed, grated cucumber
- Minced or grated garlic
- Chopped dill (and mint, if using)
Stir gently until everything is evenly distributed. At this point, your Greek tzatziki sauce recipe will already smell garlicky and fresh.
Taste a small spoonful and start adjusting:
- Add more lemon juice for brightness
- Sprinkle in a little extra salt if the flavors feel muted
- Stir in another spoonful of dill if you want it more herb-forward
Raw garlic becomes more pronounced as it sits, so what tastes subtle now may taste just right after chilling.
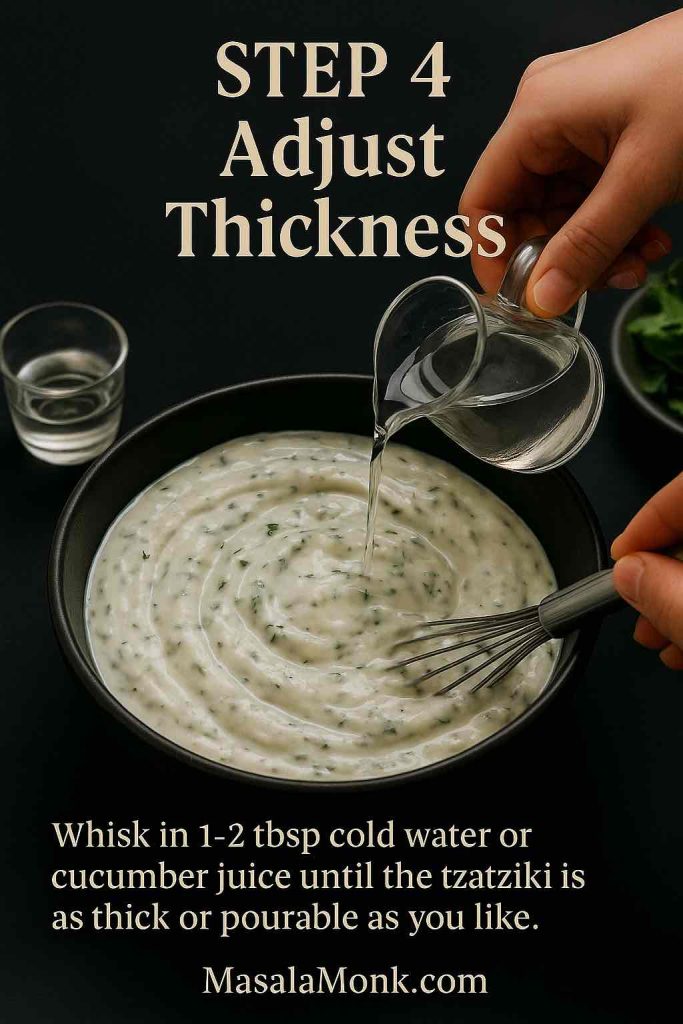
Step 4: Adjust the Thickness
Decide how you plan to use the sauce:
- For dipping and gyros, keep it thick.
- For drizzling over salads or bowls, add 1–2 tablespoons of cold water (or a little of the salty cucumber juice you squeezed out earlier) and whisk again until it flows smoothly.
The beauty of this Greek tzatziki sauce recipe is that you can shift the texture without changing the flavor.
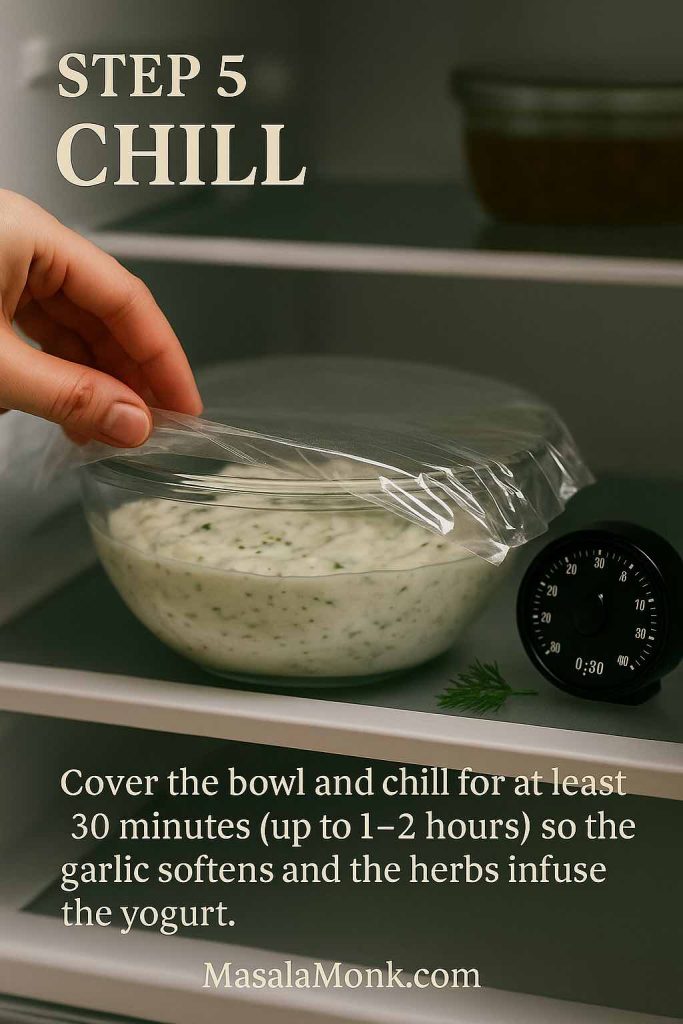
Step 5: Chill
Cover the bowl and refrigerate for at least 30 minutes, and ideally for 1–2 hours. During this time, the garlic softens, the herbs perfume the yogurt and the cucumber flavor moves from individual bits into the whole sauce.
Tzatziki eaten immediately is good; tzatziki that has rested a bit is noticeably better.
Step 6: Serve
Just before serving:
- Spoon the tzatziki into a shallow bowl.
- Swirl the surface with the back of a spoon.
- Drizzle a little extra olive oil on top.
- Scatter a pinch of chopped dill or a few tiny mint leaves over everything.

Now it’s ready to set down next to warm pita, grilled meats, roasted vegetables or simply a plate of sliced cucumber and carrots.
Also Read: Tres Leches – Mexican 3 Milk Cake Recipe
Why This Greek Tzatziki Sauce Recipe Fits a Mediterranean Way of Eating
Beyond taste, tzatziki has a few qualities that make it particularly useful if you’re leaning toward more Mediterranean-style meals.
First, Greek yogurt itself is a nutrient-dense ingredient. Because it’s strained, it usually carries more protein and less lactose than regular yogurt, all while keeping a good amount of calcium and live cultures. Many health-focused articles note that this combination supports satiety, bone health and gut health, especially when yogurt is eaten regularly as part of an overall balanced diet.
Second, the rest of the ingredients are simple and whole: cucumber, garlic, olive oil, herbs and lemon. These match up perfectly with the foods emphasized in Mediterranean-style patterns—lots of vegetables, herbs, quality fats and minimal processing. Long-term research has repeatedly associated those patterns with lower risk of heart disease, stroke and type 2 diabetes.
Finally, tzatziki is intense in flavor, so you only need a modest amount to make simple food appealing. A spoonful or two over a plate of grilled vegetables and lentils can be the difference between “virtuous but dull” and “I’d happily eat this again tomorrow.”
If you’re already building meals from other Mediterranean-leaning ideas—such as quinoa-based meal prep bowls or big, colorful salads inspired by a deep dive into daily salad habits—tzatziki slides right into that rhythm.
Ten Greek Tzatziki Sauce Recipes from One Master Bowl
Once you’re comfortable making the master version, small changes create a whole family of variations. You don’t need totally new recipes; you need a handful of smart tweaks.
Below are ten ways to adapt this Greek tzatziki sauce recipe, along with ideas on where each one shines.
1. Everyday Five-Minute Tzatziki
Some nights, the idea of salting, draining and squeezing cucumber is enough to send you toward bottled dressing. For those moments, a streamlined version helps.
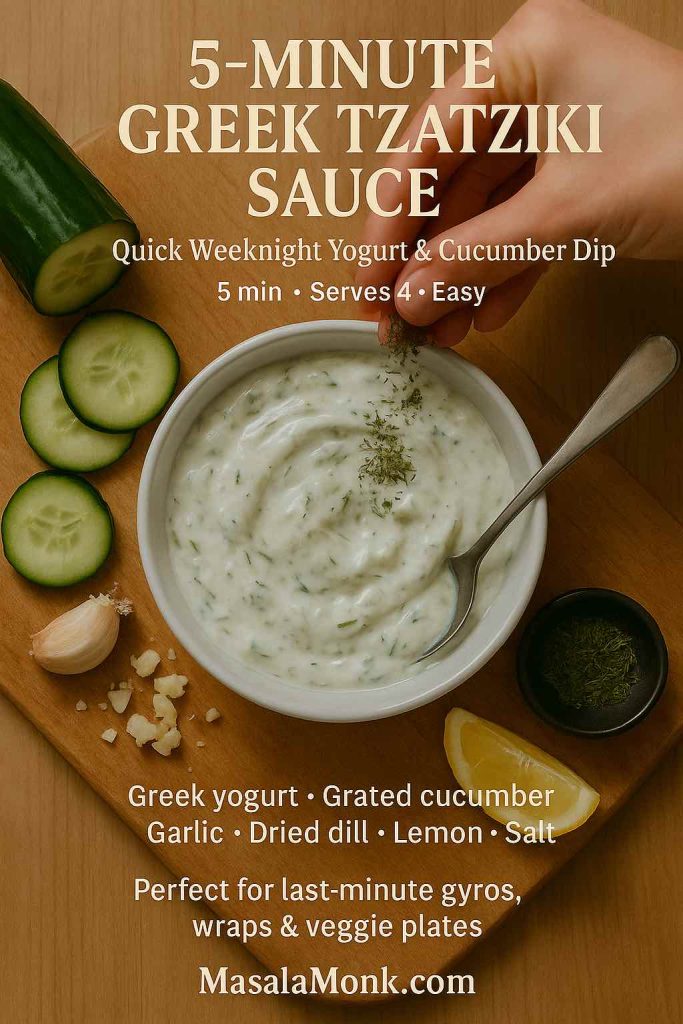
- Grate the cucumber and squeeze it gently in paper towels without salting or resting.
- Use just 1 clove of garlic plus ½ teaspoon garlic powder for an easier, less intense bite.
- Swap fresh dill for 1–2 teaspoons dried dill weed if you don’t have fresh herbs on hand.
The flavor won’t be as layered as the full version, and the sauce may loosen a little as it sits, yet it still tastes like a proper Greek tzatziki sauce recipe—cool, garlicky and satisfying. It’s perfect for quick pita sandwiches, simple grilled chicken or as a last-minute dip for vegetable sticks.
Also Read: Simple Bloody Mary Recipe – Classic, Bloody Maria, Virgin & More
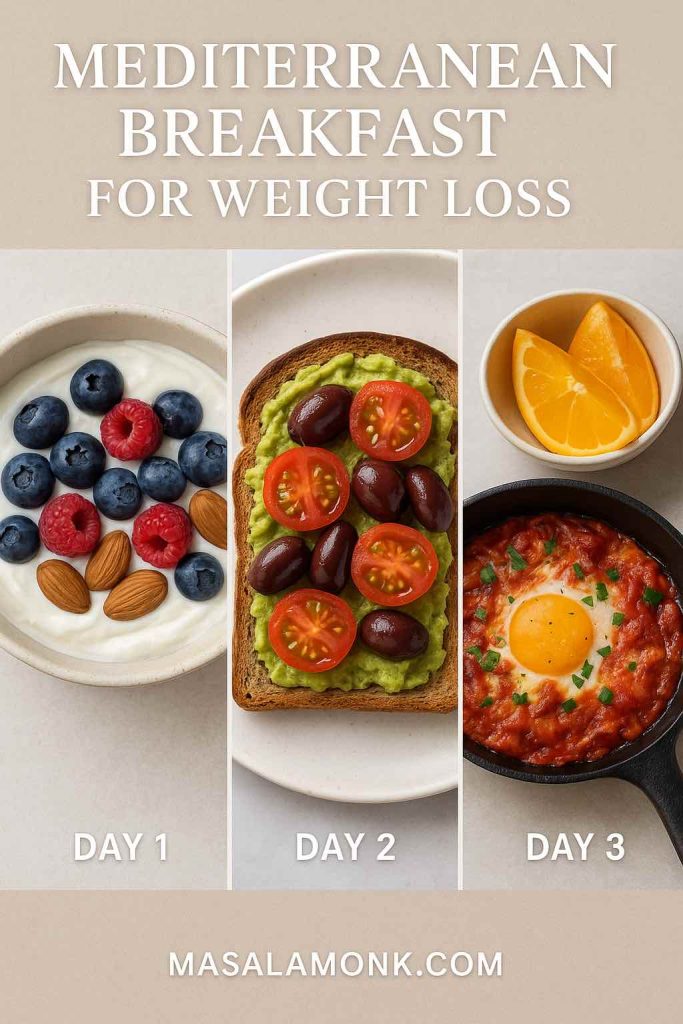
2. Recipe of Low-Calorie, High-Protein Tzatziki Greek Sauce
When you want a sauce that feels especially light but still comforting, you can nudge the recipe in that direction without losing its character.
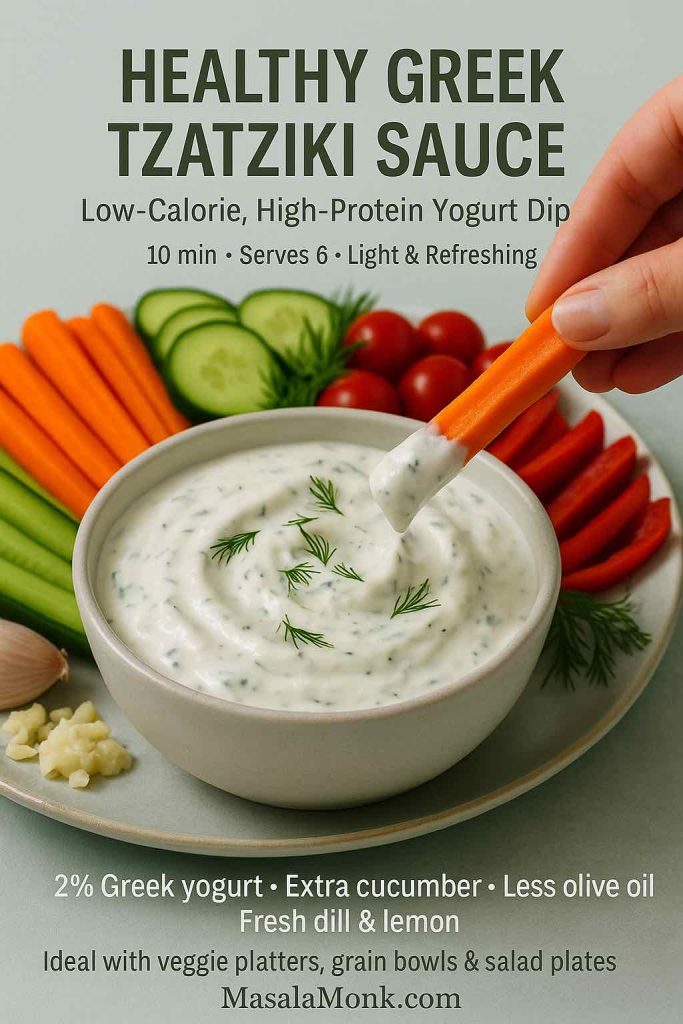
Try this approach:
- Use 2% Greek yogurt instead of full-fat.
- Reduce olive oil to 1 tablespoon.
- Increase the grated cucumber slightly and add a bit more fresh dill for volume and freshness.
Because Greek yogurt is naturally higher in protein than regular yogurt, this variation still feels substantial. Comparison articles and nutrition breakdowns point out that Greek yogurt often delivers nearly double the protein of traditional yogurt per cup.
This version works beautifully on top of grilled fish, baked chicken, roasted vegetables or as a dressing for grain bowls. It also pairs nicely with lighter mains like a ladle of crock pot lasagna soup or a square of cottage cheese lasagna when you want a mixture of cozy and fresh on the same plate.
3. Dairy-Free / Vegan Recipe for Greek Tzatziki-Style Sauce
For guests who avoid dairy—or for days when you’re simply experimenting with plant-based cooking—you can mimic the feel of tzatziki with a few swaps.
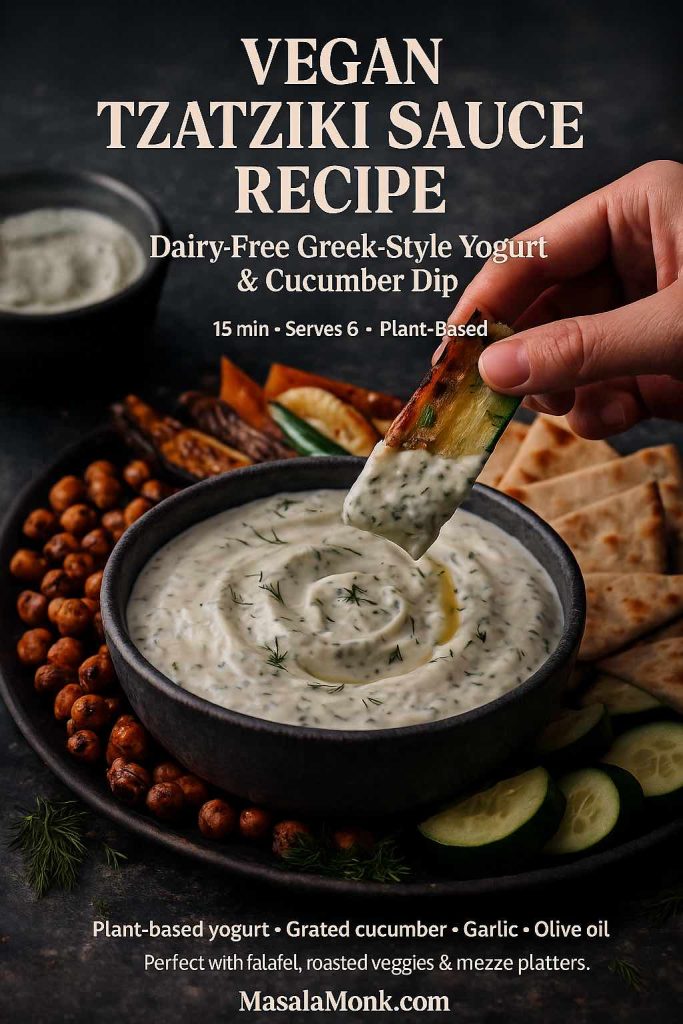
Use this pattern:
- Choose a thick, unsweetened plant-based yogurt made from soy, coconut or almonds.
- Add 1 extra tablespoon of olive oil to bring back some of the richness you’d get from full-fat dairy.
- Keep the garlic, lemon and dill generous to ensure a bright, savory flavor.
This dairy-free twist is lovely with roasted vegetables, falafel, lentil patties or Mediterranean-style quinoa bowls similar to those in plant-based meal prep ideas.
You can also thin it down a little and use it as a sauce over roasted chickpeas, baked sweet potato wedges or stuffed peppers.
4. Recipe for Thick Greek Tzatziki Sauce for Gyros
When the sauce needs to stay tucked into bread, it should lean thicker and punchier.
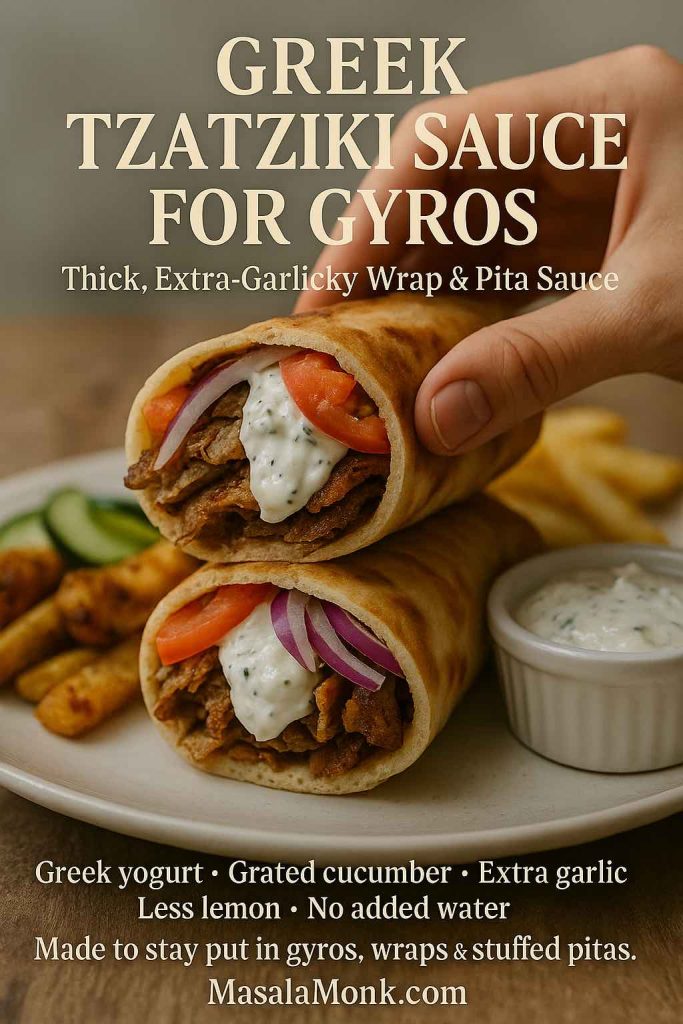
Make these adjustments:
- Squeeze the cucumber extra thoroughly so almost no liquid remains.
- Skip adding water entirely; let the sauce stay dense.
- Use the full 3 cloves of garlic and keep lemon to the lower end (around 1 tablespoon) so it doesn’t get runny.
Spread this thick tzatziki down the center of warm pita, add slices of grilled or roasted meat, tuck in tomatoes and onions, then fold everything up. It’s the sauce that ties the sandwich together and keeps it moist, much like the role sauces play in the best chicken sandwich recipes.
You can also use this version as a spread inside flatbread wraps, shawarma-style sandwiches or even on burgers topped with feta and grilled vegetables.
5. Chicken Gyro Bowls with Tzatziki
Instead of wrapping everything in bread, you can turn the same components into a bowl that’s easier to portion and reheat.
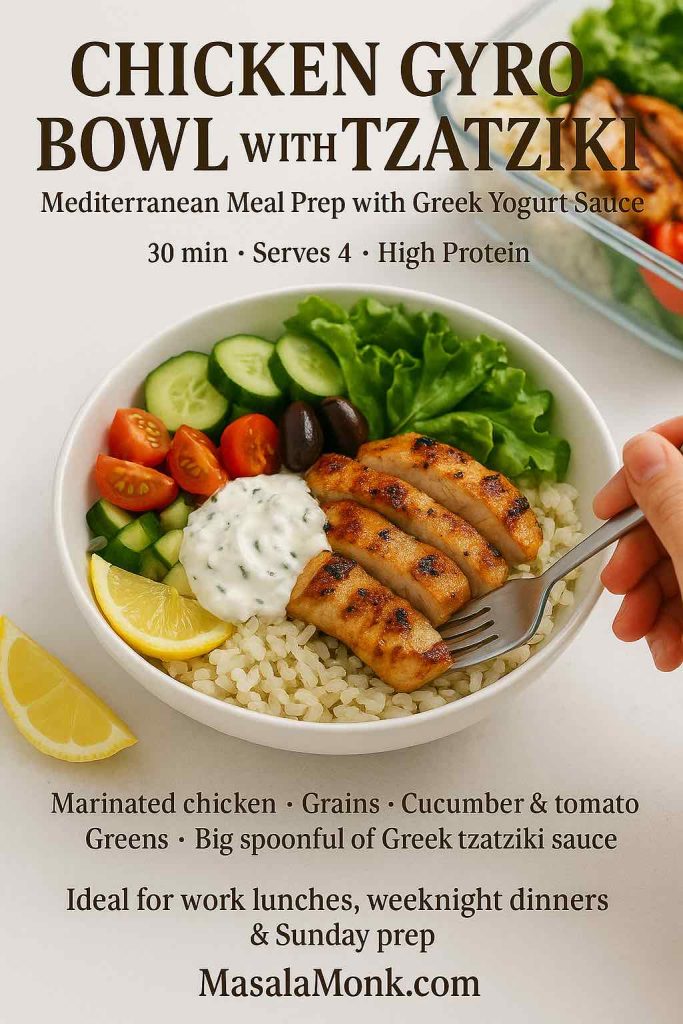
Here’s one way to do it:
- Marinate chicken thighs or breast strips in olive oil, lemon juice, crushed garlic, dried oregano, salt and pepper.
- Grill or roast until the edges are charred and the center is juicy.
- Build bowls with a base of rice, quinoa or bulgur, then add chopped cucumber, tomato, red onion, lettuce and olives.
- Finish with a generous spoonful of the master Greek tzatziki sauce recipe on top.
Between the yogurt sauce and the chicken, you get a protein-rich meal that still feels fresh. This style of bowl sits in the same category as high protein overnight oats—different time of day, same idea of using yogurt to make food more filling without feeling heavy.
These bowls also pack well for lunch: keep the warm elements and the tzatziki separate, then combine them when you’re ready to eat.
6. Greek Tzatziki Salad Dressing
Sometimes salads need more than a vinaigrette to feel satisfying. That’s where a pourable version of tzatziki comes in.
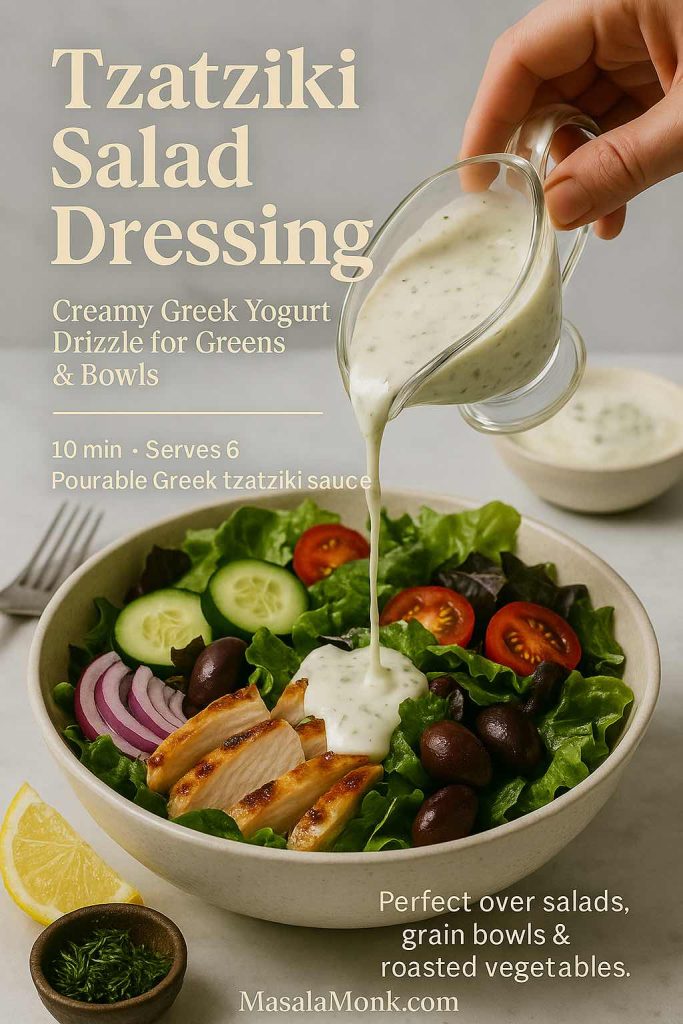
To turn your sauce into a dressing:
- Whisk 2–4 tablespoons of cold water into 1 cup of tzatziki until it reaches a smooth, drizzly consistency.
- Add an extra teaspoon or two of lemon juice.
- Taste and adjust salt; greens can handle slightly stronger seasoning than raw vegetables served alone.
This dressing is excellent over chopped cucumber–tomato salads, crunchy romaine, simple mixed greens or roasted vegetable platters. It fits neatly with the kind of salads encouraged in a comprehensive look at daily salad habits, where the emphasis is on making vegetables truly enjoyable, not a chore.
You can also drizzle this thinner Greek tzatziki sauce recipe over grain bowls, roasted potatoes or even leftover roasted vegetables to give them new life.
7. Chunky Mezze Tzatziki
When you’re assembling a mezze-style spread for guests, a chunkier, more textural tzatziki feels especially inviting on the table.

To create that version:
- Prepare the master recipe as usual, keeping it fairly thick.
- Dice an extra handful of cucumber into tiny cubes and fold them in after chilling.
- Increase dill and mint slightly for a more herb-packed bite.
- Finish the surface with olive oil and a dusting of sumac or smoked paprika.
Serve this bowl alongside warm pita, crunchy vegetables and one or two companion dips inspired by spinach dip recipes.
For extra protein and variety, add air fryer hard-boiled eggs to the board. They’re easy to peel and make a satisfying combination with cool tzatziki and warm bread.
8. Sour-Cream-Enriched Tzatziki (or No-Cucumber Version)
On some days, you might find a tub of sour cream in the fridge and no cucumber in sight. Even then, you can produce something in the spirit of this Greek tzatziki sauce recipe.
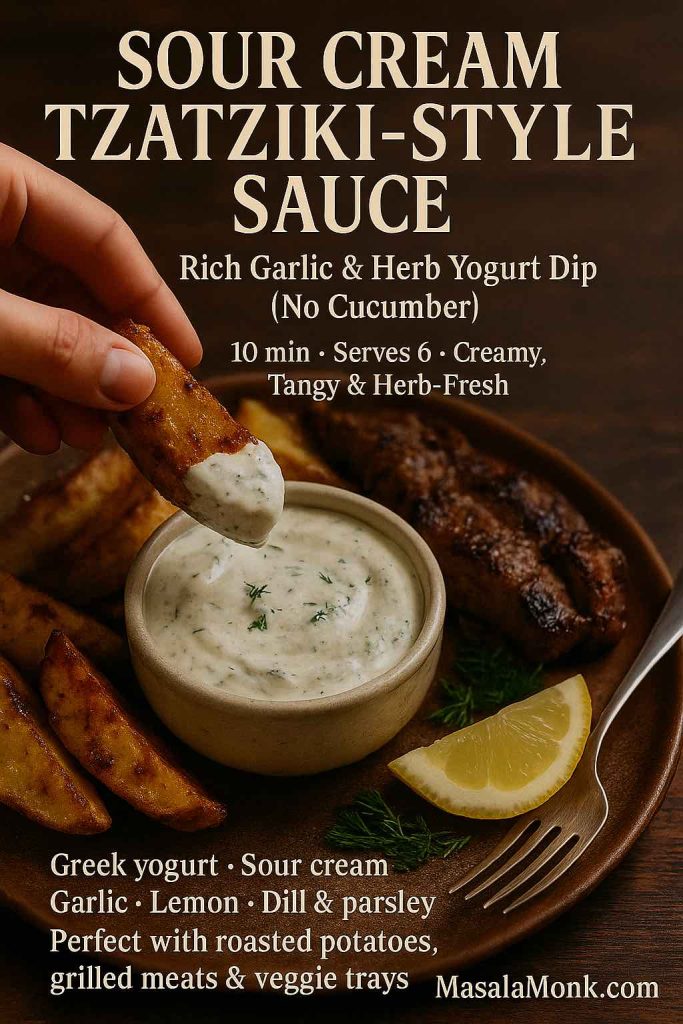
Try this variation:
- Use ½ cup Greek yogurt and ½ cup sour cream.
- Skip the cucumber or replace it with a small handful of finely chopped, seeded tomato for freshness.
- Keep garlic, lemon and herbs generous so the sauce stays bright instead of heavy.
The result is more like a garlicky herb cream, yet it plays a similar role on the plate. Spoon it over roasted potatoes, grilled steak, baked salmon, steamed vegetables or even next to a cozy dish like green bean casserole when you want something cool and tangy on the side.
9. Salmon with Greek Tzatziki Sauce Recipe
Fish and yogurt might not sound like an obvious pairing at first, but the combination works beautifully—especially with oily fish like salmon.
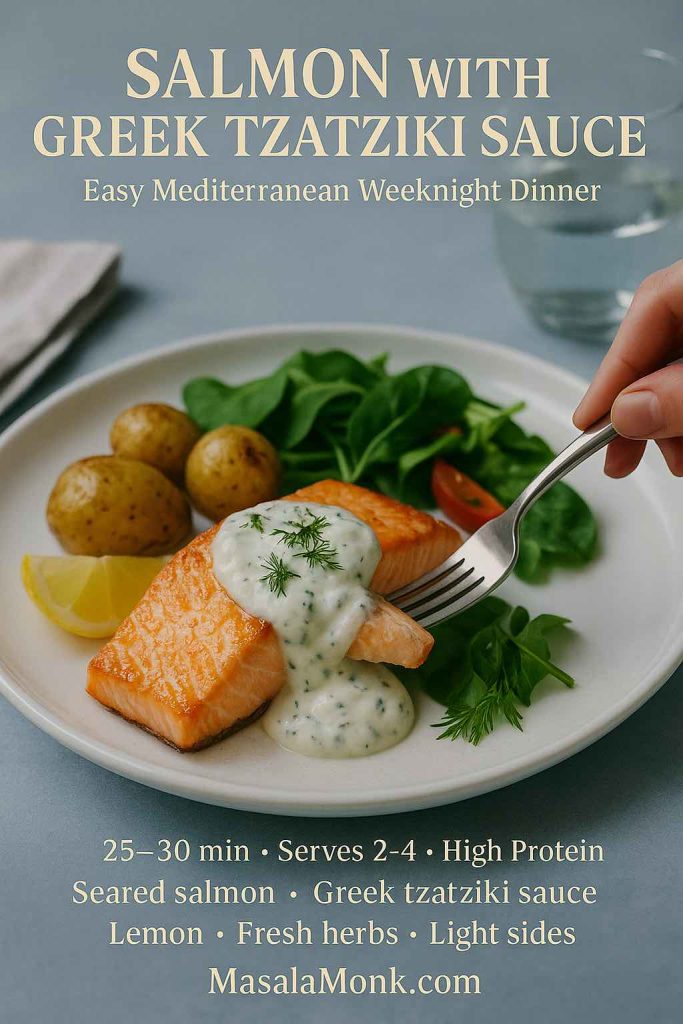
A simple way to bring them together:
- Rub salmon fillets with olive oil, salt, pepper and a squeeze of lemon.
- Roast or pan-sear until just cooked through and beginning to flake.
- Serve with a generous spoonful of chilled tzatziki either on top or alongside.
- Add a green salad, roasted vegetables or simple potatoes to round out the plate.
This kind of meal—fish, vegetables, olive oil and a small amount of fermented dairy—mirrors classic Mediterranean patterns that many studies highlight as beneficial for long-term heart health.
You can easily swap in cod, haddock or trout; just adjust cooking times and keep the serving of tzatziki the same.
Also Read: Whiskey Sour Recipe: Classic Cocktail, Best Whiskey & Easy Twists
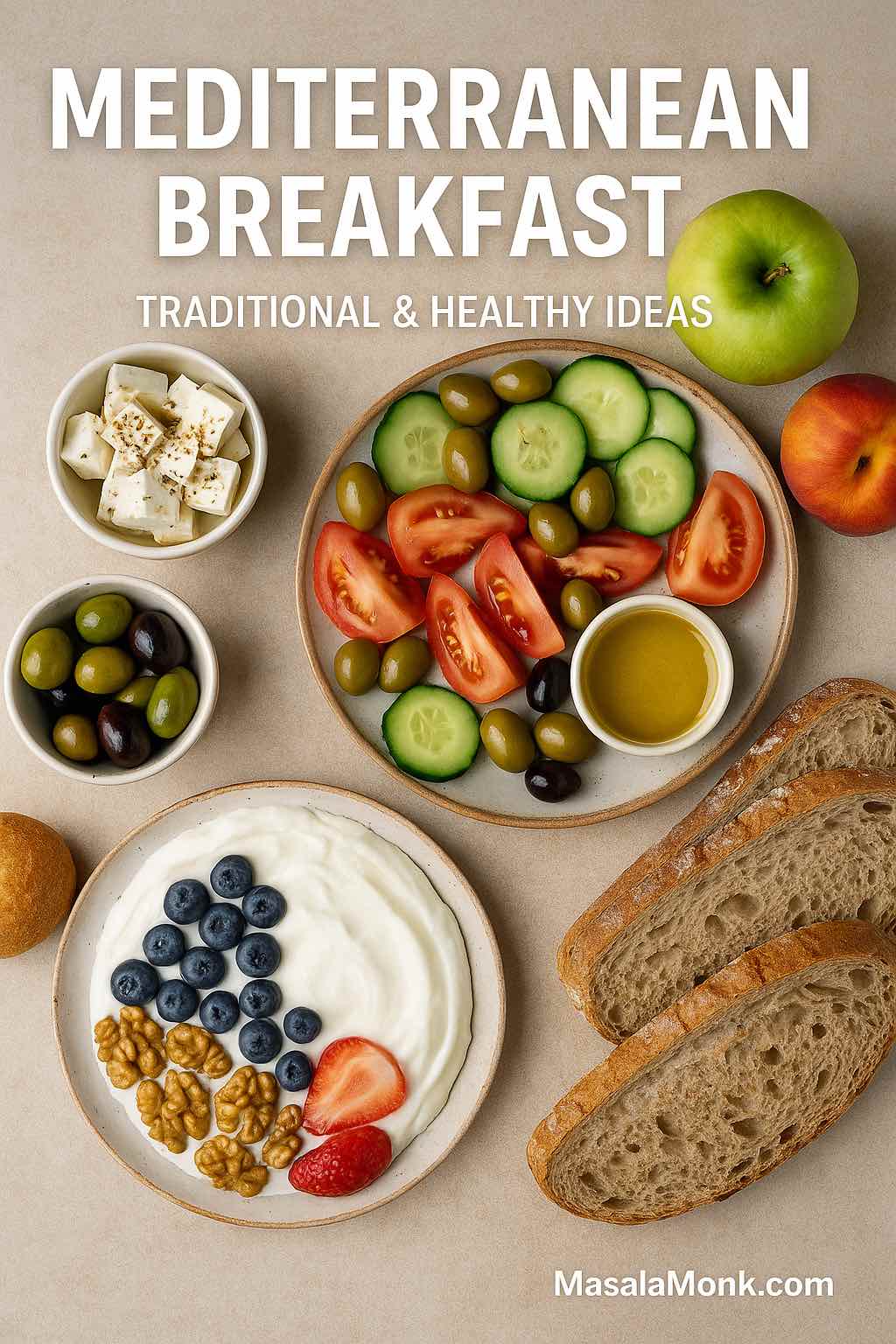
10. Brunch and Breakfast with Tzatziki
Finally, tzatziki doesn’t need to stay confined to lunch and dinner. It also has a comfortable place in brunch spreads and weekend breakfasts, especially for people who enjoy savory options.
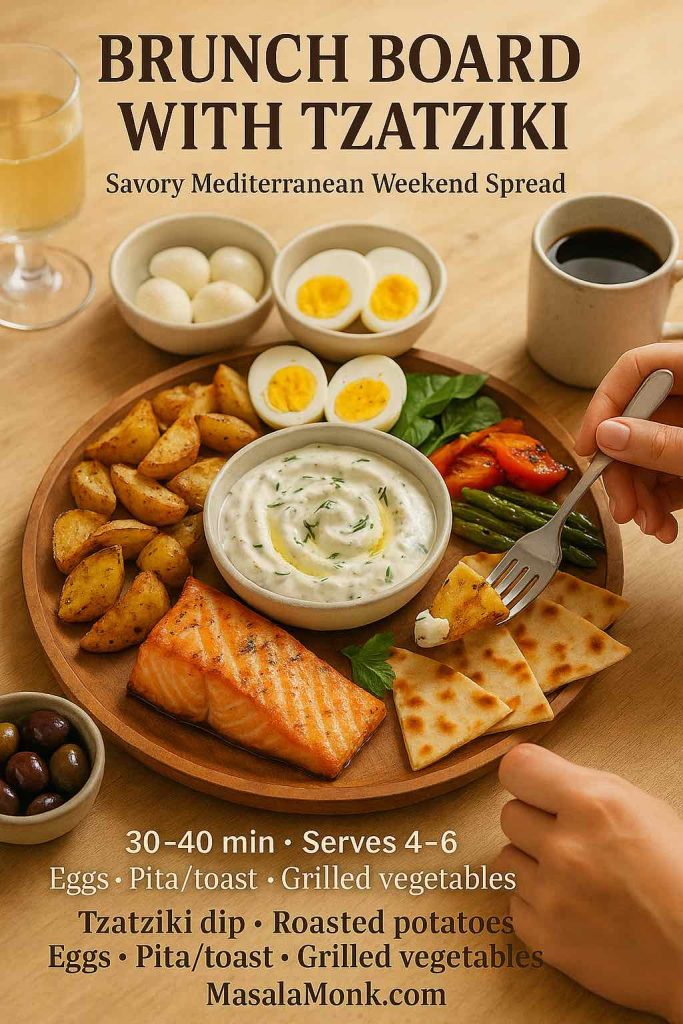
Consider a few ideas:
- Put together a savory brunch board with roasted potatoes, grilled vegetables, olives, slices of cheese, air fryer hard-boiled eggs and a big bowl of tzatziki in the center for dipping.
- Balance a sweet tray of pancakes or French toast sticks with a plate of warm pita, tomatoes, cucumbers and tzatziki so guests can build both sweet and savory bites.
- Offer both tzatziki and high protein overnight oats so Greek yogurt shows up in two completely different forms at the same meal.
If you enjoy brunch cocktails, a light, bubbly drink such as a French 75 or one of the twists from a mimosa recipe collection pairs nicely without overwhelming the herbs and garlic.
Building Meals Around Tzatziki
Once there’s a bowl of tzatziki in your fridge, the way you think about meals starts to shift. Instead of beginning with a complicated main dish, you can start with the sauce and assemble around it.
Mezze Nights
One of the easiest ways to use a Greek tzatziki sauce recipe is in a mezze-style spread—essentially a table filled with small plates so everyone can pick and choose. For instance, you might set out:
- Tzatziki and one or two other dips, perhaps a spinach-based dip inspired by spinach dip recipes
- Warm pita or flatbreads
- Sliced cucumbers, carrots, radishes and bell peppers
- A simple tomato and onion salad
- Olives, pickled peppers and small cubes of cheese
- A plate of air fryer hard-boiled eggs or grilled chicken pieces for protein
Everyone can build little bites: a piece of bread with tzatziki and tomato, a slice of egg dipped into the sauce, or raw vegetables dragged through a small puddle of yogurt and herbs. It feels relaxed, social and abundant without requiring hours at the stove.
Comfort Main + Fresh Sauce
On cooler evenings, you might crave something heartier—lasagna, rich soups or baked casseroles. Tzatziki can still play a role there, not as the star, but as the fresh sidekick.
Imagine:
- A bowl of crock pot lasagna soup with a green salad and a small dish of tzatziki nearby so people can add a spoonful to their bowls if they like.
- A slice of cottage cheese lasagna alongside a cold, crisp cucumber salad dressed with a thinner Greek tzatziki sauce recipe.
- A holiday-style plate with green bean casserole, roasted potatoes and grilled chicken, brightened with a spoonful of tzatziki instead of another heavy gravy.
This mix of cozy and fresh keeps comfort food from feeling one-note.
Quick Weeknight Plates
On busy nights, tzatziki can turn very simple components into a complete-feeling meal:
- Roast a tray of chicken pieces and potatoes with olive oil, salt and herbs. Serve everything with a bowl of tzatziki and a quick side salad.
- Pan-fry or bake fish fillets, add lemon, then spoon tzatziki on top right at the table.
- Warm pita or flatbreads, stuff them with leftover roasted vegetables or meat, and slather tzatziki inside as the main sauce.
Because the sauce is already waiting in the fridge, these meals feel fast without reading as “thrown together.”
Also Read: Peanut Butter Cookies (Classic Recipe & 3 Variations)
Storing and Making Ahead Greek Tzatziki Sauce Recipe
A fresh Greek tzatziki sauce recipe keeps nicely in the fridge, though it does change subtly over time.
Here are a few practical points:
- Container: A clean, lidded glass or plastic container keeps the flavors focused and prevents stray fridge smells from sneaking in.
- Timeframe: For the best texture and flavor, try to eat tzatziki within 3–4 days. After that, the cucumber can soften a bit too much and the garlic may become a little sharper.
- Separation: If a bit of liquid pools on top, just stir it back in. If it seems a little thin, folding in a spoonful of fresh Greek yogurt right before serving can restore some body.
- Serving hygiene: If you’re putting tzatziki out for a gathering, spoon a portion into a smaller bowl instead of letting everyone dip directly into the storage container. That way, any double-dipping or stray crumbs don’t affect the whole batch.
For especially busy weeks, one useful trick is to make the base ahead—yogurt, olive oil, garlic, lemon, salt and herbs—then grate and squeeze the cucumber on the day you want to serve. That gives the yogurt time to develop flavor while keeping the cucumber at its freshest and crispest.
Freezing isn’t recommended; the texture of yogurt and cucumber suffers too much after thawing.
Also Read: Homemade Hot Chocolate with Cocoa Powder Recipe
Tzatziki, the greek sauce recipe in a bigger picture
It’s easy to think of tzatziki as “just a sauce.” Yet looked at another way, a reliable Greek tzatziki sauce recipe is a quiet tool for shaping how you cook and eat:
- It gives raw vegetables a destination besides plain hummus or ranch.
- It gives leftover grains, beans or roasted vegetables an easy way to feel new again.
- It provides a creamy element for meals that still lean on vegetables, legumes, whole grains and fish—exactly the kind of pattern associated with the Mediterranean diet and its long list of possible health benefits.
You don’t have to change everything at once. Simply get comfortable making this sauce, keep a bowl in your fridge when you can, and see where it naturally ends up: next to roasted vegetables, on top of salmon, tucked into sandwiches, or drizzled onto salads. Over time, you may notice that your plates look a little more colorful, a bit more vegetable-forward and—perhaps most importantly—much more fun to eat.
FAQs on Greek Tzatziki Sauce Recipe
1. What is a classic Greek tzatziki sauce recipe made of?
A classic Greek tzatziki sauce recipe usually includes thick Greek yogurt, grated and well-squeezed cucumber, fresh garlic, extra virgin olive oil, lemon juice (or a mild vinegar), salt, black pepper and plenty of fresh dill or a mix of dill and mint. Altogether, these ingredients create a cool, tangy and garlicky cucumber yogurt sauce that works as both a dip and a dressing. For the best texture, the yogurt should be strained and the cucumber should be salted and squeezed so the sauce stays thick and creamy instead of watery.
2. How do I make an easy Greek tzatziki sauce recipe for beginners?
For a simple version, start with plain Greek yogurt in a bowl, then stir in finely grated cucumber (pressed dry in a paper towel), minced garlic, a spoon of olive oil, a squeeze of lemon, salt, pepper and dried or fresh dill. Mix everything until smooth and taste to adjust the lemon and salt. Even though the sauce improves after resting in the fridge, it still tastes delicious right away, which makes this easy tzatziki sauce a great option for busy weeknights or last-minute guests.
3. Which yogurt is best for a Greek tzatziki sauce recipe: Greek or regular?
Generally, Greek yogurt is preferred because it is thicker and richer than regular yogurt, so the tzatziki holds its shape and clings nicely to bread, meat and vegetables. Regular yogurt contains more whey, so it tends to be runnier and can make the sauce feel thin. However, if regular yogurt is all you have, you can strain it through a fine cloth or coffee filter for a couple of hours in the fridge; once it thickens, it behaves much more like Greek yogurt in a tzatziki sauce recipe.
4. Can I make a Greek tzatziki sauce recipe without cucumber?
Yes, you can still prepare a tasty garlic yogurt sauce even if you have no cucumber. In that case, simply leave the cucumber out and increase the herbs, garlic and lemon slightly so the flavor stays bright. Alternatively, very finely chopped, seeded tomatoes or a small amount of grated zucchini can bring a bit of freshness and texture. While it won’t be a textbook tzatziki, this no-cucumber version still works wonderfully as a dip for vegetables, a topping for grilled meats or a spread for wraps.
5. Is a Greek tzatziki sauce recipe healthy?
Most of the time, tzatziki is considered a lighter, nutrient-dense sauce. It is built on strained yogurt, which typically provides protein, calcium and live cultures, along with cucumber, olive oil, garlic, herbs and lemon. Compared with many cream-based or mayonnaise-heavy sauces, a Greek tzatziki sauce recipe usually contains less saturated fat and often more protein per spoonful. Naturally, the overall healthiness still depends on what you eat it with and how large the portions are, but as a way to make vegetables and lean proteins more appealing, tzatziki fits very comfortably into a balanced pattern of eating.
6. How can I make a low-calorie or low-fat Greek tzatziki sauce recipe?
To lighten the sauce, try using 2% or low-fat Greek yogurt instead of full-fat, keep the olive oil to a tablespoon or less, and add extra cucumber and herbs for volume. In addition, you can skip any extra oil drizzled on top when serving. The texture remains creamy because Greek yogurt is naturally thick, while the cucumber and dill keep the flavor refreshing. This kind of healthier tzatziki works especially well with grilled chicken, baked fish, grain bowls and big salads where you want a creamy element that doesn’t overshadow the rest of the meal.
7. Can I make a dairy-free or vegan Greek tzatziki sauce recipe?
Absolutely. For a dairy-free or vegan tzatziki, use a thick, unsweetened plant-based yogurt made from soy, coconut, almond or oat instead of Greek yogurt. Then add grated, squeezed cucumber, garlic, herbs, olive oil, lemon, salt and pepper just as you would in a traditional recipe. Because some non-dairy yogurts can be quite mild, you may want a little extra lemon and garlic to keep the flavor bright. This vegan tzatziki is excellent with falafel, roasted vegetables, grain bowls and wraps, and it fills the same role as a classic Greek tzatziki sauce recipe on the plate.
8. What is the difference between tzatziki and gyro sauce?
In many cases, they are essentially the same thing: a thick Greek tzatziki sauce recipe used as the sauce for gyros. However, gyro sauce is often made a little thicker and more garlicky so it stays inside the pita and stands up to heavily seasoned meat and onions. Sometimes, restaurants use a sour-cream-based garlic sauce or a yogurt-mayo mix and still call it “gyro sauce.” If you specifically want the Greek cucumber yogurt sauce, choose a tzatziki recipe built on Greek yogurt, cucumber, garlic, olive oil, lemon and dill, and then simply keep it extra thick for gyros.
9. Can I use sour cream instead of Greek yogurt in a Greek tzatziki sauce recipe?
You can, although the result will be slightly richer and tangier. Sour cream is thicker than regular yogurt but usually a bit looser than Greek yogurt, so the sauce may turn out softer unless you reduce other liquids. One popular option is to use half Greek yogurt and half sour cream to get the best of both: protein and density from the yogurt, plus silkier texture from the sour cream. This hybrid works nicely for baked potatoes, roasted vegetables and grilled meats, particularly when you want a more indulgent twist on standard tzatziki.
10. How long does homemade Greek tzatziki sauce last in the fridge?
Generally, homemade tzatziki keeps well for about 3 to 4 days in a sealed container in the refrigerator. Over time, the cucumber softens and releases a little extra liquid, and the garlic flavor can intensify. If a bit of liquid collects on top, simply stir it back in; if the sauce becomes too thin for your liking, you can fold in a spoonful of fresh Greek yogurt to thicken it again. Once it smells or tastes off, or if the surface looks discolored, it’s best to discard it and make a fresh batch.
11. Can I freeze a Greek tzatziki sauce recipe?
Freezing isn’t recommended. When yogurt and cucumber thaw, the texture often turns grainy and watery, and the fresh, clean flavor that makes tzatziki so appealing is mostly lost. The cucumber can become mushy, and the yogurt may separate. Instead of freezing, it’s better to make smaller batches more often or prepare the yogurt base ahead of time without cucumber, then stir in freshly grated, squeezed cucumber on the day you plan to serve the sauce.
12. How can I turn a Greek tzatziki sauce recipe into a salad dressing?
Turning tzatziki into a salad dressing is straightforward. Start with the sauce in a bowl, then whisk in cold water, milk or a little extra lemon juice a tablespoon at a time until it reaches a pourable consistency. Taste and add a pinch more salt or herbs if the flavor feels diluted. This thinner version works wonderfully over chopped cucumber-tomato salads, mixed greens, roasted vegetable bowls and even grain-based salads. In this way, one Greek tzatziki sauce recipe can cover both dips and dressings, making it an especially versatile staple to keep in your kitchen.