When you type foods to eat while fasting 16/8 into a search bar, you’re really asking two practical questions at once: what to drink during the 16-hour fasting window so you stay in a true fast, and what to place on your plate during the eight-hour eating window so you feel satisfied, energized, and consistent. Right from the start, the answer is refreshingly simple: build every plate around protein, high-fiber carbohydrates, and healthy fats, using mostly minimally processed, Mediterranean-leaning foods. That template is easy to shop, effortless to rotate, and—crucially—sustainable. For a quick primer on that food pattern, the American Heart Association’s Mediterranean overview and the practical Oldways Mediterranean Pyramid are both excellent, real-world starting points.
What to Drink While Fasting (and Why It Matters)
During the 16-hour fast, calories count; hydration does too. Consequently, choose plain water, sparkling or mineral water, black coffee, and unsweetened tea—all of which hydrate without adding energy. You can explore our post on Homemade Electrolytes for Fasting to get more ideas on what to drink. If you like simple “how much” rules of thumb, benchmarks from the Academy of Nutrition and Dietetics are helpful, while it is important to stay hydrated, however it’s important to remind you to favor lower-sugar beverages most of the time. For a public-health reminder on swapping out sugary beverages, see CDC: water and healthier drinks.
Of course, context matters. On hot days or after workouts, a pinch of electrolytes can help without breaking your fast—as long as your drink remains unsweetened. If you prefer real-food flavors, try these refreshing Cooling Cucumber Electrolyte Quenchers or explore DIY electrolyte drink ideas and simply omit sweeteners during the fast.
A quick nuance on sweeteners: the WHO’s guideline on non-sugar sweeteners advises against relying on them for weight control. Nevertheless, some people tolerate a small amount in coffee without cravings; others do not. Test gently, observe your appetite, and use minimally.
Also Read: Tea and Intermittent Fasting
The Best First Plate to Break Your Fast (Start Gentle, Then Build)
Once you open your window, your first bites set the tone for the rest of the day. Therefore, begin with a gentle, balanced “first plate” that combines protein + easy-to-digest carbs + a little fat. After 45–90 minutes, follow with your main meal. For instance:
- A small bowl of lentil or vegetable soup with tofu or paneer and a slice of whole-grain bread.
- Eggs with sautéed spinach plus a thin chapati or sourdough wedge.
- Yogurt/curd (or fortified soy yogurt) with berries and a handful of nuts.
- A smoothie based on milk/curd (or fortified soy) with fruit and a spoon of nut butter.
If you enjoy browsing options, you’ll like this compact collection of gentle, protein-forward fast-breaking ideas you can rotate all week.
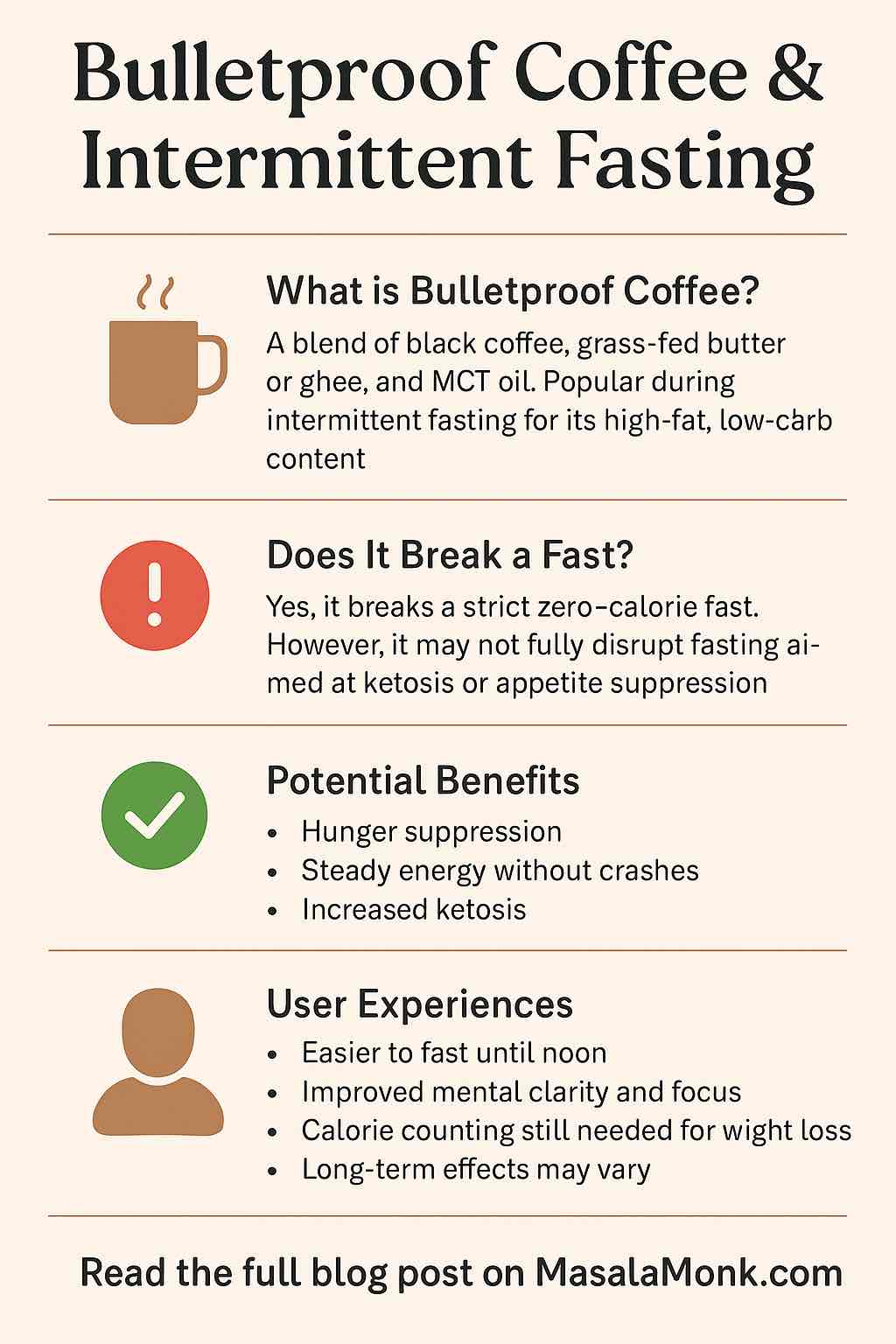
Also Read: Coffee and Fasting: All Your Questions Answered
Foods to Eat While Fasting 16/8 (Inside the Window): The Core Building Blocks
Although timing is the hallmark of intermittent fasting, food quality is what shapes energy, fullness, and results. Thus, the most practical foods to eat while fasting 16/8 (meaning during your eating window) fall into three friendly buckets:
- Protein anchors: eggs; Greek yogurt/curd; cottage cheese/paneer; fish and poultry; tofu and tempeh; dals, chickpeas, kidney beans; edamame; soy milk; nuts and seeds.
- Smart carbs (fiber-forward): oats, quinoa, brown rice, millets, whole-wheat roti, sweet potatoes, beans and lentils, and plenty of fibrous vegetables—plus fruit like berries, apples, citrus, or bananas.
- Healthy fats: extra-virgin olive oil, avocado, nuts/seeds; optionally, fatty fish if that suits your diet.
To make that even more concrete, here’s a beginner’s plate rule borrowed from public guidelines: fill half your plate with fruit/veg, and divide the other half between protein and smart carbs—a practical visual reinforced by USDA MyPlate. For specifics, the MyPlate pages for the Vegetable Group and Protein Foods Group offer quick, visual refreshers.
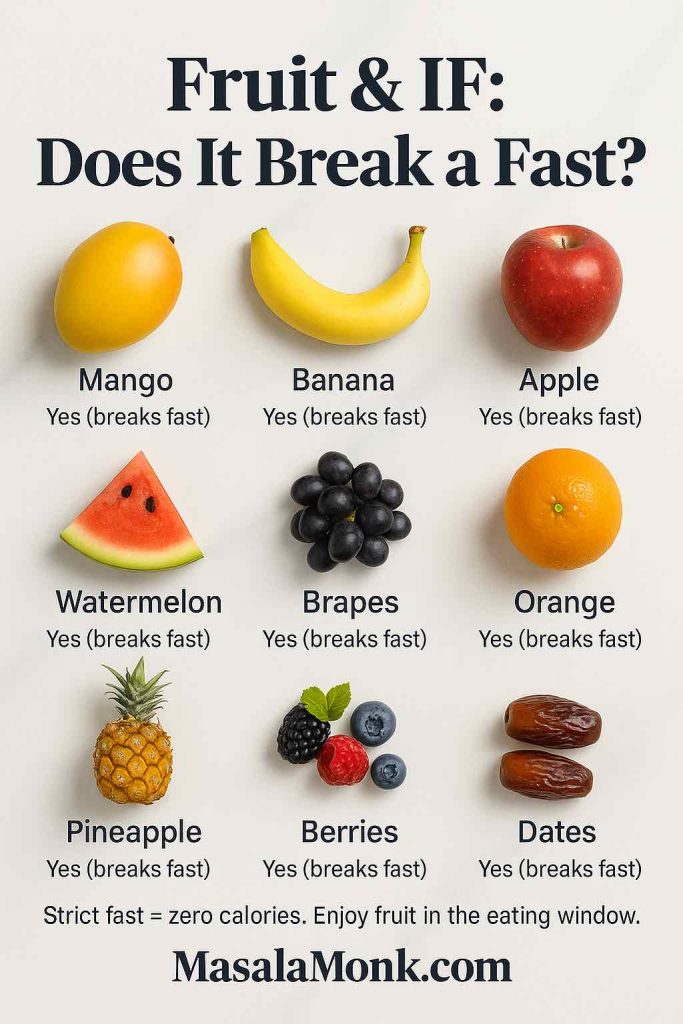
Finally, fruit definitely belongs. Pair it with protein or fat to smooth the glucose curve—think yogurt with berries, apple with peanut butter, banana with paneer or tofu. For ideas that go beyond the usual pairings, try our fruit-during-IF guide.
Also Read: Can We eats Peanuts while Intermittent Fasting?
7-Day Intermittent Fasting Meal Plan (16:8 Window Examples You Can Repeat)
Below is a complete intermittent fasting meal plan for a 12:00–8:00 pm window. Shift earlier (11–7) or later (1–9) as life demands. Each day includes a first plate to break your fast, a main meal, and a compact second plate/snack. You’ll also see vegetarian/vegan swaps and lower-carb variations so the week fits different goals. Use this as a beginner intermittent fasting meal plan, scale portions to your appetite and activity, and repeat favorites.
Portions vary by body size and training load; nevertheless, keep protein, fiber, and minimally processed ingredients at the center.
Day 1 — Mediterranean-Leaning Kickoff (foods to eat while fasting 16/8)
- 12:00 First plate: Greek yogurt/curd with berries + 1 tbsp mixed nuts.
Vegan swap: fortified soy yogurt with berries + chia. - 1:30 Main meal: Chickpea and vegetable stew in olive oil; side of quinoa; big lemony salad.
Lower-carb swap: extra veg; smaller quinoa or cauliflower “rice.” - 6:30 Second plate/snack: Grilled paneer or tofu with peppers and onions + one orange.
Helpful visual for this style of eating: the Oldways Mediterranean beginner list is clear and friendly.
Day 2 — Indian Comfort, Balanced (foods to eat while fasting 16/8)
- 12:00 First plate: Two besan chillas with curd and kachumber (or soy yogurt if vegan).
Recipe inspiration: paneer-stuffed besan chilla (use your favorite version). - 2:00 Main meal: Rajma or chole over brown rice or millets; sautéed greens.
Lower-carb swap: halve rice, double greens and cucumber salad. - 7:30 Second plate/snack: Fruit bowl (berries/papaya/banana) + almonds or walnuts.
Day 3 — High-Protein Emphasis (foods to eat while fasting 16/8)
- 12:00 First plate: Eggs (omelette or boiled) with sautéed spinach + a thin sourdough wedge.
Vegan swap: chickpea “omelette” (besan) with spinach. - 2:00 Main meal: Tandoori chicken or paneer/tofu tikka; roasted vegetables; small portion of brown rice or a roti.
Lower-carb swap: skip grain, double vegetables; add avocado. - 6:45 Second plate/snack: Cottage cheese/paneer or tofu cubes with cherry tomatoes and olives.
Also Read: Best Nuts for Intermittent Fasting: Maximizing Satiety and Nutritional Benefits
Day 4 — Power Bowls (foods to eat while fasting 16/8)
- 12:00 First plate: Smoothie bowl—milk/curd (or fortified soy), banana/berries, flax or peanut butter; sprinkle seeds.
Lower-carb tweak: more berries, less banana; tofu on the side. - 1:45 Main meal: Lentil-quinoa bowl with roasted cauliflower/carrots; tahini-lemon dressing.
Vegan/veg by default. - 7:00 Second plate/snack: Mixed sprouts chaat with tomato, onion, coriander, lemon, and a dash of chaat masala.
How-to: sprouted moong overnight—step by step.
Day 5 — Fish or Tofu Friday (foods to eat while fasting 16/8)
- 12:00 First plate: Miso soup with tofu and greens; small fruit.
- 2:00 Main meal: Grilled fish with olive oil, herbed potatoes, and a large salad; or tofu steaks if plant-based.
Lower-carb swap: roasted zucchini/broccoli in place of potatoes. - 7:15 Second plate/snack: Greek yogurt/curd parfait with apple and cinnamon; or soy yogurt for vegan.
Day 6 — Comfort Curry, Light Finish (foods to eat while fasting 16/8)
- 12:00 First plate: Small bowl of moong dal + steamed veggies + lemon.
- 2:00 Main meal: Coconut-milk vegetable curry (or chicken curry) over brown rice/millets; cucumber-tomato salad.
Lower-carb swap: less rice, extra salad; add olives or avocado. - 6:30 Second plate/snack: Peanut chaat or roasted chana; sliced guava or pear.
Day 7 — Social Sunday, Still Smart (foods to eat while fasting 16/8)
- 12:00 First plate: Yogurt/curd + low-sugar granola + berries.
Vegan swap: soy yogurt + homemade nut-seed granola. - 2:00 Main meal: Pizza-style whole-grain flatbread with tomato, mushrooms, peppers, olives, mozzarella (or tofu ricotta), olive oil; side salad.
Lower-carb swap: portobello “pizza” caps or eggplant slices. - 7:00 Second plate/snack: Paneer/tofu stir-fry with sesame and greens; or a small hummus plate with crudités.
How to rotate and prep: batch-cook two proteins (dal/chana and tofu/paneer or chicken/fish), one smart carb (quinoa, brown rice, or millets), and a tray of roasted vegetables every 3–4 days. If you need variety within the carb bucket, have a look at Quinoa for Weight Loss: Benefits, Nutrition, and How to Cook Ideas.
Vegetarian, Vegan, and Low-Carb Tracks (Fast Customization, Same Principles)
To craft a vegetarian intermittent fasting meal plan, anchor each eating occasion with paneer/cottage cheese, yogurt/curd, eggs (if you eat them), and legumes (chana, rajma, dal). Layer olive oil, nuts, and seeds for healthy fats. To build a vegan intermittent fasting meal plan, swap dairy for fortified soy yogurt/milk, use tofu or tempeh as daily proteins, and rotate edamame and beans. If you’re curious about tempeh’s texture and flavor, this quick primer on tempeh as a versatile vegan protein will help you get started.
For a low-carb intermittent fasting plan, there’s no need for extremes. Emphasize non-starchy vegetables, lean or plant proteins, olive oil/avocado/nuts, and smaller portions of grains or starchy veg. That plant-forward approach is still compatible with the Mediterranean pattern and, frankly, more livable than strict keto for most people. If you want a broader view of how to begin this style of eating, Cleveland Clinic’s Mediterranean food list and starter plan is grounded and usable.
Also Read: Yogic Meal Plan and Intermittent Fasting – Insights from Sadhguru
What to Eat While Intermittent Fasting for Weight Loss (Tactics That Compound)
Because many readers pursue 16:8 for fat loss, it helps to connect the dots between intermittent fasting and diet quality. To that end, use this checklist inside the window:
- Front-load protein at every eating occasion—yogurt/curd, eggs, tofu/tempeh, dal or chana, fish or poultry, plus nuts/seeds.
- Fill half your plate with plants—non-starchy vegetables plus fruit. The plate visual from USDA MyPlate keeps this effortless.
- Choose slow carbs most of the time: oats, quinoa, brown rice, whole-wheat roti, sweet potato, legumes.
- Use fats intentionally: extra-virgin olive oil, avocado, nuts, seeds. Measure pours and handfuls.
- Drink during the fast: water, coffee, and tea. For a simple refresher, see the Cleveland Clinic drinks guide.
- Break the fast gently: see the first-plate ideas above or browse fast-breaking suggestions.
- Batch-cook so your defaults are strong: try high-protein vegetarian meal prep or vegan meal prep ideas to save time during the week.
For a sane, evidence-aware perspective on weight and diet quality (and why extremes backfire), the British Dietetic Association’s plate guidance for weight loss and notes on fad diets are both sensible and easy to skim.
Foods to Avoid (or Save for Occasional Treats)
Even within a flexible intermittent fasting food plan, certain choices make timing harder rather than easier:
- Sugary beverages and ultra-processed snacks—they spike appetite and can trigger rebound eating.
- Very high-fat “first meals” right after fasting—greasy, heavy foods often feel rough on the stomach and push you toward grazing later.
- Mindless nibbling in the window—if your plate lacks protein and fiber, you’ll snack soon after.
By contrast, treating richer items as occasional—and positioning them inside a complete meal with protein and vegetables—preserves the rhythm that makes 16:8 work. For a quick, friendly reminder on lower-sugar beverage choices, visit Nutrition.gov’s hydration and beverage tips.
Troubleshooting Your 16:8 Schedule (Common Hurdles, Easy Fixes)
- If hunger hits hard mid-morning: sip water or unsweetened tea first; if you still feel low, shift your window earlier (e.g., 11–7) for a week.
- If you crash after your first plate: increase protein (yogurt + nuts, eggs, tofu) and choose easy digesting carbs (fruit, soup with pulses) before your main meal.
- If evenings get snacky: make dinner more substantial—double vegetables, keep protein steady, and add a measured spoon of olive oil or a quarter avocado for satisfaction.
- If weekends derail you: keep timing flexible (e.g., 14:10 on social days) and return to 16:8 on Monday—consistency beats rigidity.
- If coffee jitters you on an empty stomach: consider delaying coffee by an hour and keep it plain; the nuance around stimulants and stress is covered here: Coffee + cortisol.
Foods to Eat While Fasting 16/8: Shopping Lists You Can Copy
Because shopping clarity makes or breaks adherence, these condensed lists keep decisions simple:
Proteins to rotate: eggs; Greek yogurt/curd; cottage cheese/paneer; tofu/tempeh; chicken/fish; dals, chickpeas, kidney beans; edamame; soy milk; nuts and seeds.
Smart carbs to prefer: oats; quinoa; brown rice; millets; whole-wheat roti; sweet potatoes; legumes; fruit; plus loads of leafy, cruciferous, and colorful vegetables.
Healthy fats to include: extra-virgin olive oil; avocado; almonds, walnuts, pistachios, peanuts; seeds like flax, chia, sesame, and sunflower.
To make legumes especially appealing, remember that pulses are naturally rich in fiber and nutrients—reasons the UN’s Food and Agriculture Organization highlights in their notes on the nutritional benefits of pulses and this broader 2025 celebration of the power of pulses. Consequently, dals, chana, and rajma deserve a regular place on your table.
Also Read: Are Lentils Good for Weight Loss? Benefits, Recipes, and Science Explained
Intermittent Fasting Diet Plan for Beginners (Routine That Fits Real Life)
To live with the 16:8 rhythm comfortably, set up a routine that survives busy weeks:
- Pick a consistent window most days (e.g., 12–8). Flex for social plans; return to baseline the next day.
- Prep “fast-breakers” you enjoy: soup portions in the freezer, yogurt/curd cups, chopped fruit, roasted nuts.
- Keep two fallback plates on standby: eggs + veg + toast; or tofu/paneer tikka + salad + one roti.
- Hydrate preemptively—first thing in the morning and mid-afternoon—even before you feel thirsty. When you want variety, revisit cooling cucumber electrolytes and DIY hydration recipes for unsweetened options during the fast and low-sugar ideas during the window.
- Meal prep smartly: for plant-forward weeks, browse high-protein vegetarian meal prep or vegan meal prep ideas; for omnivore weeks, batch-roast chicken/fish and tray-bake vegetables for effortless mix-and-match plates.
If you like evidence windows, it’s worth noting that time-restricted eating research continues to evolve. For a balanced perspective, you can read a randomized trial in the New England Journal of Medicine comparing calorie restriction with/without TRE (summary here), or a more applied brief from the NIH on TRE in metabolic syndrome. Nevertheless, regardless of study headlines, diet quality and routine are the levers you actually control each day.
Special Notes for Women, PCOS, Menopause & Diabetes
Some readers do better with 14:10 or even 12:12 during demanding phases. Women navigating perimenopause, anyone with PCOS, and readers with diabetes (particularly those on glucose-lowering medication) should tailor fasting and meal timing with their clinician. All the same, the meal fundamentals in this guide—protein at each eating occasion, plant-rich plates, slow carbs, and measured healthy fats—remain widely applicable. If you want a gentle on-ramp, glance at vegan meal prep ideas or high-protein vegetarian prep to see how easy it is to keep protein and fiber high without complex rules.
Example Day Revisited: Foods to Eat While Fasting 16/8 (Vegetarian Window)
To connect everything, here’s a compact vegetarian day that mirrors the template:
- 12:00 — Yogurt/curd with berries and crushed nuts (or fortified soy yogurt with chia).
- 3:00 — Fruit + almonds (apple with almonds, banana with peanut butter, or berries with paneer/tofu cubes).
- 7:30 — Paneer tikka or chole with quinoa or whole-wheat roti; mixed salad with olive oil.
Notice how every moment includes protein, plants, and a bit of fat—a simple combination that makes the difference between a plan you can follow and a plan that unravels when life gets busy.
Also Read: The Science of Protein: Maximizing Muscle Growth and Recovery
What to Eat During Intermittent Fasting 16/8: The Weekly Rhythm in One Line
At this point, it should be clear that foods to eat while fasting 16/8 are not about restriction; they’re about focus. Protein first, plants plentiful, fats thoughtful, carbs mostly slow. Rotate different legumes, swap in seasonal vegetables, choose grains you enjoy, and keep fruit in the mix. As a result, you’ll feel fuller on fewer calories, stabilize energy, and make the plan feel less like a “diet” and more like a habit.
And if you ever need a quick nudge, open a friendly visual like the Oldways Mediterranean Pyramid or a basic plate reminder such as USDA MyPlate. They’re simple for a reason: when your defaults are this good, 16:8 becomes far easier to keep—meal after meal, week after week.
Also Read: What is the Mediterranean Diet? Free PDF Meal Plan Inside
FAQs
1) What are the best foods to eat while fasting 16/8 during the eating window?
Build plates around lean or plant proteins (eggs, curd/yogurt, paneer/tofu/tempeh, fish or chicken, dals/beans), high-fiber carbs (oats, quinoa, brown rice, whole-wheat roti, lentils, sweet potato, fruit), and healthy fats (olive oil, avocado, nuts, seeds). This simple mix keeps you full, supports weight loss, and makes foods to eat while fasting 16/8 easy to repeat.
2) What can I eat during intermittent fasting 16/8 as a beginner?
Start with a gentle first meal (yogurt + berries + nuts; eggs + fruit; dal soup + roti) and one main plate (protein + veggies + smart carbs). Add one small snack if needed (paneer/tofu pieces; fruit + almonds). This beginner intermittent fasting meal plan is fuss-free and sustainable.
3) What can I drink while fasting (no calories)?
Stick to water (still or sparkling), black coffee, and unsweetened tea. Zero-calorie electrolytes are fine if truly unsweetened. Save milky coffee, juice, smoothies, and shakes for the eating window.
4) What can you eat during the 8 hours of intermittent fasting?
Prioritize protein at every eating occasion, fill half the plate with vegetables and fruit, and choose slow-digesting carbs. Consequently, your foods to eat while fasting 16/8 list becomes: protein + plants + measured fats.
5) What is the best food to break a fast?
Go gentle: protein + easy carbs + a little fat. Examples: lentil/veg soup with tofu or paneer; eggs with a slice of whole-grain; yogurt/curd with berries and nuts; or a milk/curd + fruit smoothie with nut butter. Then, after 45–90 minutes, eat your main meal.
6) Which foods should I avoid while intermittent fasting?
Limit sugary drinks, ultra-processed snacks, and very greasy “first meals” right after fasting. These can spike hunger and derail your window.
7) Can I eat fruit during intermittent fasting 16/8?
Yes—inside the 8-hour window. Pair fruit with protein or fat (yogurt + berries, apple + peanut butter, banana + paneer/tofu) to improve satiety.
8) Does bone broth break a fast?
Yes. Bone broth contains calories and protein; therefore, it breaks the strict fasting period. Use it inside your eating window.
9) What can you consume during intermittent fasting if you’re hungry?
Hydrate first (water, black coffee, plain tea). If hunger persists daily, shift your window earlier, increase protein at the first meal, and ensure enough fiber and volume from vegetables.
10) Is there a simple intermittent fasting food list I can follow?
Absolutely:
- Protein: eggs, yogurt/curd, paneer/tofu/tempeh, chicken/fish, dals/beans, edamame, nuts/seeds.
- Carbs (fiber-forward): oats, quinoa, brown rice, whole-wheat roti, millets, lentils, sweet potato, fruit, veg.
- Fats: olive oil, avocado, nuts/seeds.
11) What to eat during intermittent fasting 16/8 for weight loss?
Emphasize protein (at every meal), large servings of vegetables, and mostly slow carbs; measure fats. As a result, your calorie deficit becomes easier without strict tracking.
12) What to eat during intermittent fasting 16/8 for vegetarians?
Anchor meals with paneer, curd/yogurt, dals/chana/rajma, tofu/tempeh, eggs (if you eat them), plus whole grains and vegetables. Hence, foods to eat while fasting 16/8 stay protein-rich and plant-forward.
13) What to eat during intermittent fasting 16/8 for vegans?
Rely on tofu/tempeh, edamame/soy milk, legumes (dal, chana, rajma), nuts/seeds, and whole grains. Add plenty of vegetables and fruit for fiber and micronutrients.
14) Can I combine keto with intermittent fasting (keto + 16/8)?
You can, yet it’s optional. A low-carb intermittent fasting plan—with lots of non-starchy veg, olive oil/avocado/nuts, and steady protein—often feels more livable than strict keto while still supporting fat loss.
15) What is a high-protein, low-carb 16/8 day?
First plate: eggs or tofu + sautéed veg.
Main meal: paneer/tofu/chicken/fish + big salad + small portion of quinoa or none.
Snack: yogurt/curd or soy yogurt with nuts.
This structure keeps foods to eat while fasting 16/8 focused on protein and fiber.
16) What to eat during intermittent fasting 16/8 for PCOS?
Prioritize protein at each meal, fiber-rich carbs (legumes, whole grains, vegetables, fruit), and healthy fats; keep sugary drinks minimal. Consider a consistent window and balanced plates to support appetite and energy.
17) What is the best intermittent fasting for menopause or perimenopause?
Many feel better with 14:10 or flexible 16:8. Regardless, protein at every meal, vegetables and fruit at half the plate, and slow carbs with healthy fats often help with steadier energy and satiety.
18) What to eat during intermittent fasting for diabetes?
Coordinate with your clinician. Generally, prioritize protein, vegetables, pulses, and slow carbs while spacing meals in the 8-hour window. Monitor blood glucose closely when adjusting timing.
19) What to eat in the 16/8 window if I work out?
Around training, keep the first plate light but protein-anchored (yogurt + fruit + nuts, or tofu/egg scramble). Post-workout, add slow carbs (quinoa, brown rice, millets, sweet potato) with lean protein and vegetables.
20) What is the best intermittent fasting schedule and meal plan for beginners?
Choose a stable window (12–8 or 11–7). Break the fast gently, eat one main balanced plate, and add one small protein-rich snack if needed. Repeat a few favorite meals so foods to eat while fasting 16/8 become automatic.
21) What can you eat and drink while fasting if you get headaches?
First, hydrate with water or plain tea; consider unsweetened electrolytes. Then, during the eating window, emphasize protein, vegetables, and slow carbs to stabilize energy.
22) Do zero-calorie sweeteners break a fast?
Most are effectively non-caloric, yet they may increase cravings for some. If you use them, keep amounts small during the fasting period and assess your personal response.
23) What’s the best food to break a fast for sensitive stomachs?
Start with soup (dal/veg) or yogurt/curd with fruit and a few nuts; after that, move to your main plate. This gentler sequence helps digestion.
24) Can I follow OMAD instead of 16/8?
You could, but many people find 16/8 easier for performance, digestion, and sustainability. If trying OMAD, ensure the one meal still covers protein, plants, and slow carbs.
25) What’s the difference between 16/8 and 5:2?
16/8 limits when you eat daily; 5:2 limits how much on two days per week. Either can work, though foods to eat while fasting 16/8 typically emphasize daily routine and balanced plates.
26) Does coffee with milk break a fast?
Yes—milk adds calories and breaks a strict fast. Therefore, save lattes/capuccinos for the eating window; keep coffee black while fasting.
27) What should I eat during intermittent fasting 16/8 if I’m frequently hungry?
Increase protein at the first plate, add more vegetables for volume, and choose slow carbs. Additionally, check sleep, stress, and hydration; consistency often fixes mid-window hunger.
28) What is a simple intermittent fasting meal plan free of complicated recipes?
Use a three-part template:
- First plate: yogurt/curd + fruit + nuts or eggs/tofu + veg.
- Main plate: protein + big salad/veg + slow carb.
- Snack (optional): cottage cheese/paneer, soy yogurt, tofu/paneer cubes, or fruit + almonds.
29) What are “16/8 diet power foods” I should stock weekly?
Eggs; Greek yogurt/curd; paneer/tofu/tempeh; dals/chana/rajma; leafy and colorful vegetables; oats/quinoa/brown rice/millets; olive oil/avocado; mixed nuts and seeds; berries/apples/bananas. These are the backbone of foods to eat while fasting 16/8.
30) How do I stay in a calorie deficit while fasting?
Keep protein high, pack plates with vegetables, pick mostly slow carbs, and measure fats. Batch-cook basics and repeat meals you like; the combination quietly maintains a modest deficit without micromanaging.