If you’re wondering whether a gluten sensitivity diet could finally calm the bloating, brain fog, fatigue, or stubborn skin issues—you’re far from alone. Yet the landscape can be confusing: is it celiac disease, non-celiac gluten sensitivity (NCGS), or a wheat allergy? And once you figure that out, what exactly should you eat? This guide clears the path step by step—so you can move from guesswork to a steady routine that supports your gut, your energy, and your everyday life.
Before we dive into testing, food lists, and meal plans, a brief refresher helps. If you’re new to the topic, start with our quick primer on what gluten actually is—it’ll make everything else easier to follow.
⚠️ Disclaimer: This article is for educational purposes only and is not medical advice. It does not diagnose, treat, cure, or prevent any condition. Always consult a qualified healthcare professional for personalized guidance, especially before starting a gluten sensitivity diet, changing medications, or interpreting tests. If you have urgent or severe symptoms, seek medical care immediately.
Celiac, NCGS, or Wheat Allergy—Why Your Diagnosis Shapes the Gluten Sensitivity Diet
Although the symptoms can overlap, these conditions aren’t the same—and the plan you follow depends on which one you have.
- Celiac disease (CeD) is an autoimmune condition: gluten triggers immune damage in the small intestine. Left untreated, it can lead to nutrient deficiencies, anemia, bone loss, and more.
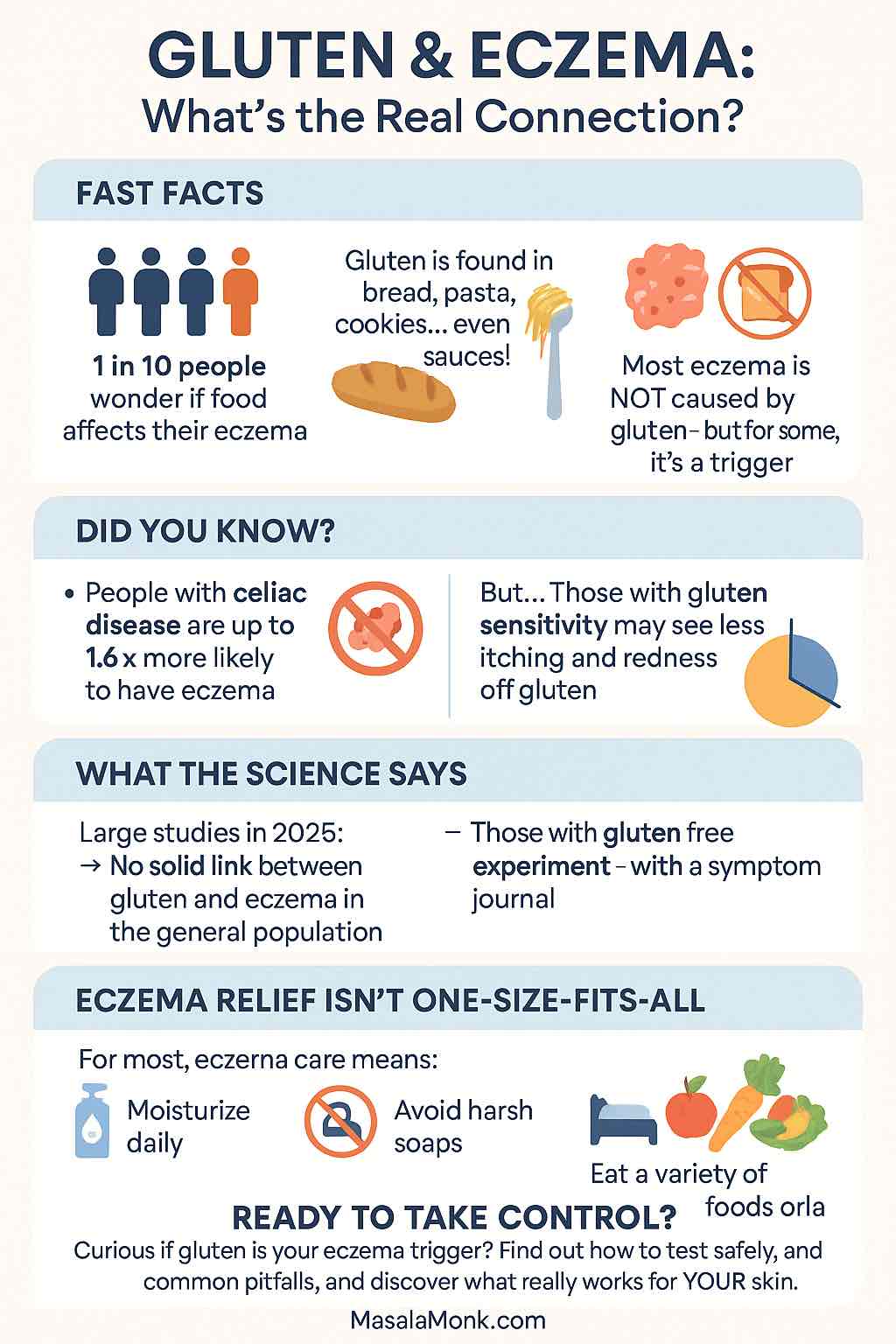
- Non-celiac gluten sensitivity (NCGS) involves gluten-related symptoms without celiac’s intestinal damage and without wheat-allergy markers. Interestingly, a subset of people with NCGS-like symptoms may actually be reacting to fructans (fermentable carbohydrates found in wheat) rather than gluten itself; Monash’s overview explains how wheat is rich in fructans, and a randomized trial explored whether fructans—not gluten—trigger symptoms in some. See Monash on wheat and fructans and the study via PubMed.
- Wheat allergy is an IgE-mediated allergy to wheat proteins (not just gluten). Reactions can include hives, wheezing, and—rarely—anaphylaxis, which clearly requires a different approach.
Because treatment and strictness differ, testing first—and only then committing to a gluten sensitivity diet—is the smartest move.
Gluten Sensitivity Symptoms: What to Watch For
If you’re considering a gluten sensitivity diet, it helps to recognize the most common gluten intolerance symptoms first. Although everyone’s experience differs, the patterns below appear consistently in clinical summaries and patient reports.
Core digestive signs of Gluten Sensitivity
To begin with, keep an eye on:
- Bloating and gas (often within hours)
- Abdominal pain or cramping
- Diarrhea, constipation, or an alternating pattern
- Nausea and early fullness
- Reflux/heartburn after wheat-heavy meals
For a clear, medical overview of GI complaints (including how they differ by age), see the NIDDK symptom summary and the Celiac Disease Foundation symptoms list.
Extra-intestinal symptoms of Gluten Sensitivity (the sneaky ones)
Meanwhile, many people notice issues outside the gut: persistent fatigue, brain fog or headaches, mood changes, joint or muscle aches, and skin flares. For accessible detail, skim Mayo Clinic’s celiac symptoms page.
Possible nutrient-deficiency clues of Gluten Sensitivity
Over time, malabsorption can show up as iron-deficiency signs (dizziness, brittle nails), mouth ulcers, or even hair thinning. Notably, dental enamel defects in kids can be an early clue—dentists are encouraged to refer when they spot tell-tale enamel patterns. Start with the NIDDK note on enamel defects and CDF’s oral-health overview.
In children (additional pointers on Gluten Sensitivity )
By contrast, kids may present with growth faltering, frequent tummy aches, loose stools, or irritability—sometimes long before anyone suspects gluten. A concise digest for families appears in CDF’s symptoms page and the NIDDK children overview.
Timing, dose, and patterns
Just as important, symptoms can spike within 30 minutes up to 48 hours after eating gluten. Some people notice a dose–response (bigger portions → bigger flares). Others discover that wheat’s fructans—a FODMAP, not gluten—drive bloating and gas; in that case, a short low-FODMAP strategy (not lifelong strict GF) may help. For context, read Monash on avoiding wheat during the low-FODMAP phase and their brief fructan/oligos explainer.
When to seek care (don’t DIY this part)
However, certain red flags need prompt medical evaluation rather than diet trials: unintentional weight loss, blood in stool, persistent vomiting, fever, severe dehydration, or night sweats. A reliable, plain-English checklist appears in Mayo Clinic’s guidance.
Quick self-audit before you change everything
Before you overhaul your routine, keep a 3–5 day food & symptom log (time eaten, portion, symptoms 0–10). Note oats, sauces/spice blends, and possible cross-contact (shared fryers, toasters, or boards). Bring the log to your appointment; clinicians can then decide on testing first—and only afterward a tailored gluten sensitivity diet. For accuracy, remember you should be on gluten before serology; the rationale is laid out in the NIDDK provider handout.
Testing First (Then Diet): How to Avoid False Negatives and Frustration
Here’s the crucial rule many people miss: don’t remove gluten before screening, or blood tests can turn falsely negative.
- First-line bloodwork typically includes tissue transglutaminase IgA (tTG-IgA) with a total IgA to check for IgA deficiency. Some clinicians add deamidated gliadin (DGP) antibodies, particularly in younger children. For approachable, trustworthy guidance, see the American College of Gastroenterology’s celiac disease overview and the NIDDK’s clear explainer for clinicians and patients on celiac testing.
- Confirmation: when screens are positive, specialists usually confirm celiac disease with an endoscopy and small-bowel biopsies.
- Why “stay on gluten” matters: the NIDDK’s provider handout is explicit—patients should be consuming gluten before testing to ensure accuracy. Skipping this step risks months of confusion. See the NIDDK PDF guidance: Provider Points—Celiac Disease.
Once you’re properly screened, you can commit to the right path—be it a strict celiac protocol or a carefully structured gluten sensitivity diet for non-celiac cases.
⚠️ Disclaimer: This article is for educational purposes only and is not medical advice. It does not diagnose, treat, cure, or prevent any condition. Always consult a qualified healthcare professional for personalized guidance, especially before starting a gluten sensitivity diet, changing medications, or interpreting tests. If you have urgent or severe symptoms, seek medical care immediately.
“Is It Gluten-Free?”—Clear Answers You Can Trust (So Labels Don’t Drive You Mad)
Label reading gets overwhelming quickly; nevertheless, a few rules of thumb dramatically reduce stress.
- Oats / Oatmeal: Oats are naturally gluten-free, but they’re frequently contaminated with wheat, barley, or rye during harvesting and processing. Choose certified gluten-free oats and introduce them gradually if you’re sensitive; a small subset of people reacts to avenin (the oat protein). For a balanced overview, see the Celiac Disease Foundation’s explainer on oats and contamination. Meanwhile, the FDA clarifies that gluten-free claims generally mean <20 ppm gluten—use their resources to understand labels: FDA gluten & food labeling and the consumer piece, Gluten-Free Means What It Says.
For kitchen-level practicality, compare our quick primers on rolled vs old-fashioned oats and quick vs instant oats. - Sourdough bread: Despite the buzz, regular wheat sourdough is not gluten-free or celiac-safe. Only sourdough made entirely with gluten-free grains and a gluten-free starter is safe. For clarity, see Beyond Celiac—Is sourdough bread gluten-free?.
- Quinoa: Naturally gluten-free, higher in protein than most grains, and fantastic for pulao, upma, bowls, and salads.
- Coffee: Plain black coffee is gluten-free; flavored products may vary—check labels.
- Ezekiel bread: The classic sprouted version contains wheat; it’s not gluten-free. If you love the texture, look specifically for GF-labeled sprouted breads.
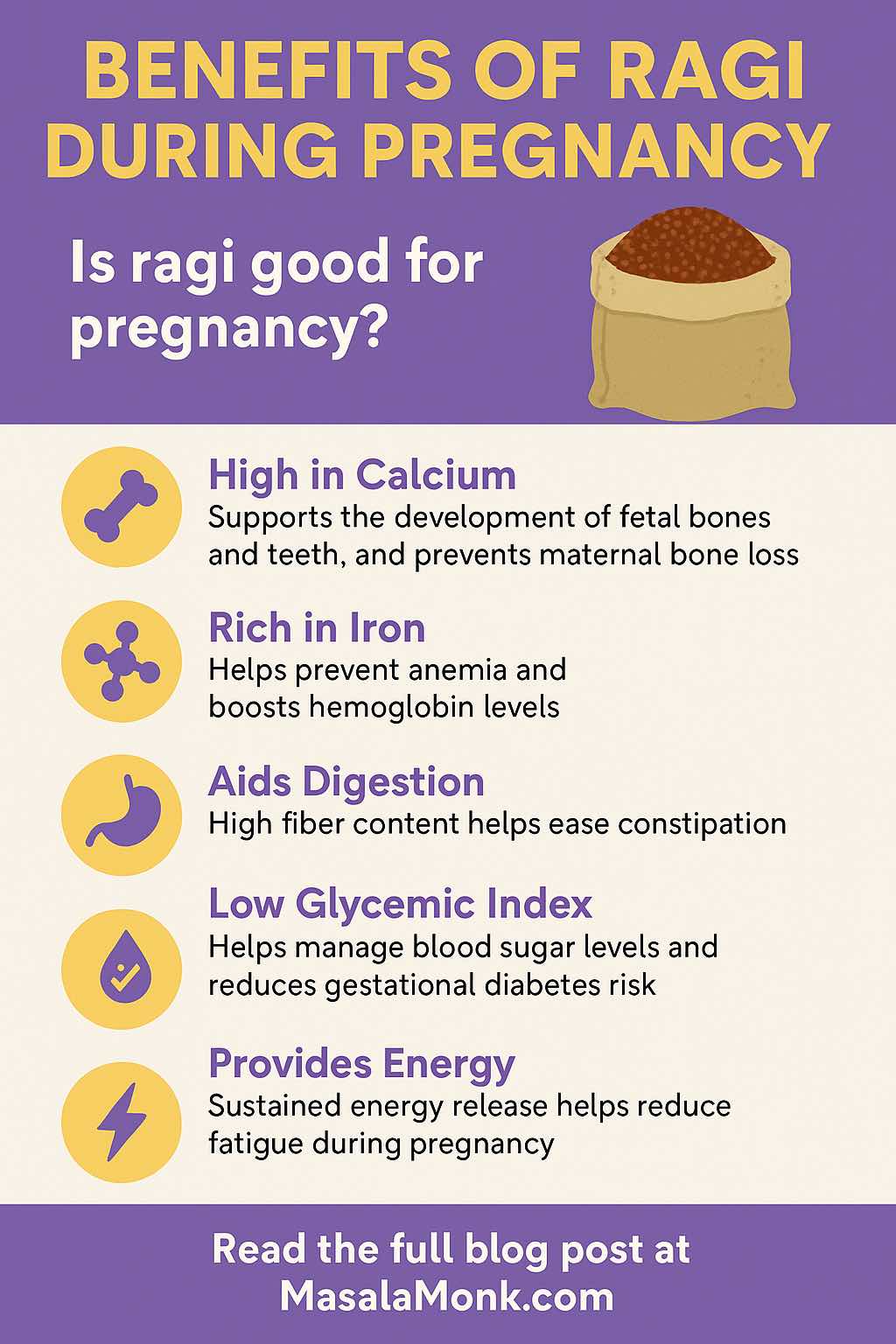
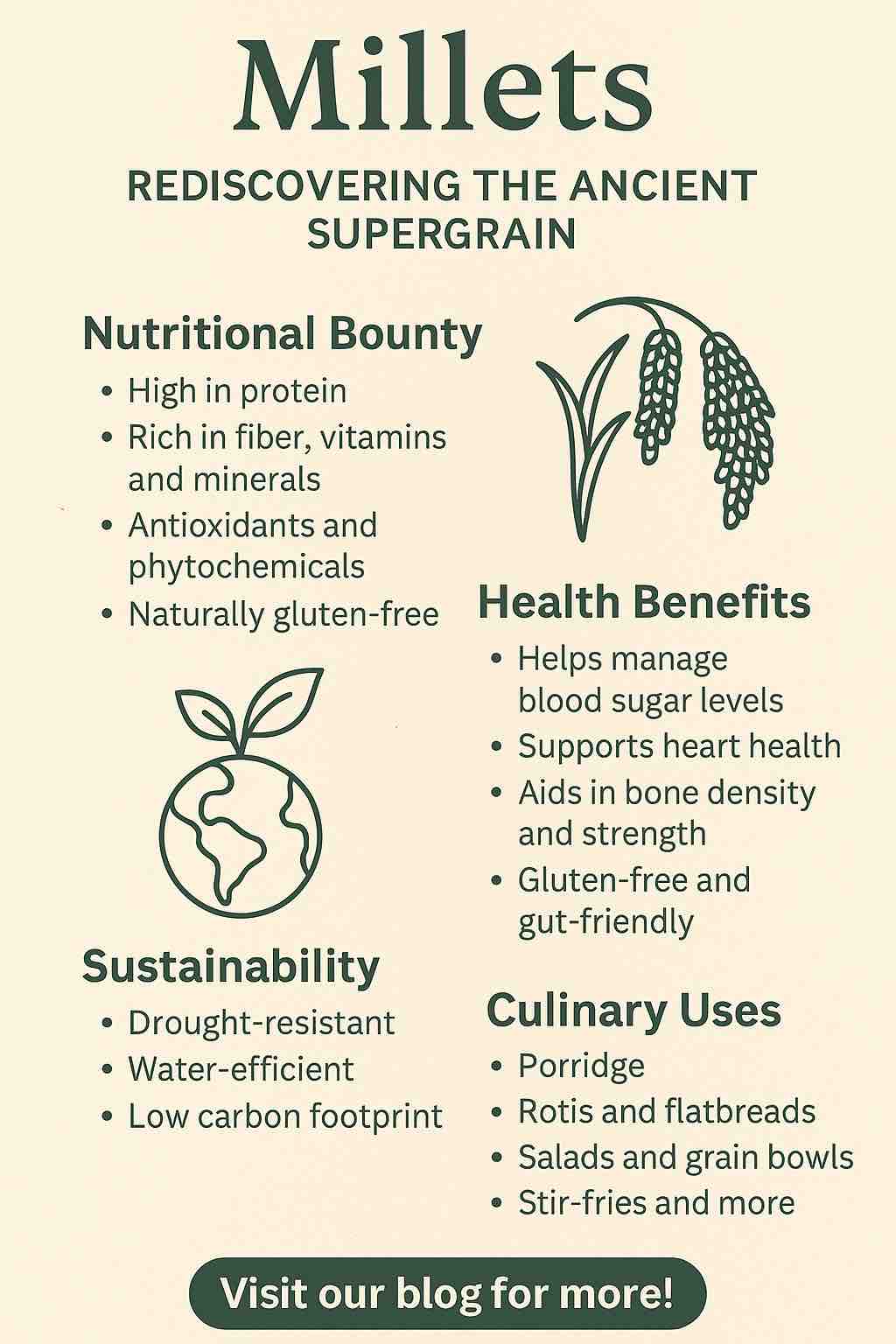
Meanwhile, many Indian staples are naturally GF. To diversify your pantry (and your recipes), explore our primer on millets—the gluten-free superfood.
The Core of a Gluten Sensitivity Diet (So You Feel Satiated, Not Deprived)
A sustainable gluten sensitivity diet leans on naturally gluten-free foods, treats packaged items with care, and prioritizes satisfaction (so you’ll actually stick with it).
Build your plate around:
- Protein: dal, chickpeas, rajma, tofu/tempeh, paneer, eggs, fish, chicken.
- High-fiber carbs: rice, millets (jowar, bajra, ragi), quinoa, potatoes, sweet potatoes, buckwheat (kuttu).
- Colorful plants: as many vegetables and fruits as you’ll enjoy daily.
- Healthy fats: olive oil, ghee (if tolerated), avocado, nuts and seeds.
- Smart pantry swaps: GF tamari (instead of soy sauce), GF pasta when you want convenience, chickpea flour (besan), tapioca, and cornstarch for binding and crisping.
Label-reading shortcut: Prefer products clearly marked “gluten-free.” In many markets, that aligns with the <20 ppm rule; the FDA pages above are handy to link inside your shopping sections so readers can fact-check in one tap.
Treats, thoughtfully: A little joy helps long-term adherence. Keep a couple of easy add-ons—like our quick dairy- and gluten-free chocolate syrup for pancakes, fruit, or yogurt (or dairy-free alt).
Pantry Setup and Batch-Cooking: The Secret Sauce of Consistency
Because weeknights are busy, a gluten sensitivity diet works best when your kitchen is prepped for “grab-and-combine.”
Your weekend hour, well spent:
- Cook two grains (say, quinoa and rice or millet) and refrigerate in clear containers.
- Pressure-cook two legumes (moong/masoor or chickpeas/rajma) and freeze in meal-size portions.
- Prep sauces you love—tahini-lemon, mint-yogurt (or coconut yogurt), and a jar of GF tamari-ginger.
- Wash and chop a big tray of vegetables; store in zip bags or boxes for stir-fries, upma, khichdi, bowls, and quick sides.
As a result, dinner becomes assembly: grain + protein + veg + sauce. Ten minutes, tops.
Also Read: How to Make Lentil Patties that Are Better Than Meat? Vegan Protein-Rich Recipe.
Your 7-Day Gluten Sensitivity Diet Meal Plan (Flexible, Flavor-First, and Realistic)
This plan favors batch cooking and repeats pantry staples to lower effort. Nevertheless, it remains varied—so you won’t feel boxed in. Wherever helpful, we’ve linked to MasalaMonk ideas you can plug in immediately.
Day 1
- Breakfast: Certified GF oats porridge with chia + berries (add cinnamon)
- Lunch: Millet khichdi (moong + carrots/peas) with a squeeze of lemon
- Dinner: Lemon rice + sautéed paneer/veg or chicken tikka (check spice blends are GF)
- Snack: Roasted chana; seasonal fruit
Day 2
- Breakfast: Ragi dosa + coconut chutney
- Lunch: Quinoa pulao with peas and carrots
- Dinner: Grilled fish (or tandoori chicken), herbed potatoes, kachumber salad
- Snack: Yogurt (or coconut yogurt) with seeds and a drizzle of honey
Day 3
- Breakfast: Millet pancakes with a light drizzle of our gluten-free chocolate syrup recipe.
- Lunch: Brown rice + rajma (verify masala blends are GF)
- Dinner: Stir-fried tofu/veg with GF tamari; top with sesame seeds (for more plant-based swap ideas, see our lentil-forward meal prep guide)
- Snack: Peanut chaat with lemon
Day 4
- Breakfast: Besan chilla + mint chutney
- Lunch: Kuttu (buckwheat) rotis + mixed sabzi
- Dinner: Baked sweet potato, black beans, salsa, avocado (squeeze of lime)
- Snack: A small handful of nuts + dates
Day 5
- Breakfast: Poha (confirm GF processing) with peanuts and coriander
- Lunch: Quinoa upma with mixed vegetables
- Dinner: Rice, dal tadka, cucumber salad
- Snack: Roasted makhana, lightly spiced
Day 6
- Breakfast: Smoothie (banana, spinach, peanut butter, milk or plant milk)
- Lunch: Millet bowl—jowar, chickpeas, roasted veg, tahini-lemon dressing
- Dinner: GF pasta aglio e olio with tomatoes and basil; side salad
- Snack: Dark chocolate (check label)
Day 7
- Breakfast: Scramble (eggs or tofu) with peppers and onions
- Lunch: Rice paper rolls (shrimp or tofu) + peanut dip (GF)
- Dinner: Slow-cooked dal + jeera rice + kachumber
- Snack: Hummus with veggie sticks
Dairy-free tweaks: Swap yogurt/milk for coconut or almond options; use olive oil or ghee if tolerated. Additionally, consider a calcium source (tofu set with calcium, leafy greens, fortified plant milks) if you’re dairy-free long-term.
Shopping Made Simple (Copy This to Notes Before You Head Out)
Grains & starches: basmati + parboiled rice, quinoa, millets (jowar, bajra, ragi), certified GF oats, buckwheat flour, potatoes, sweet potatoes, GF pasta.
Proteins: eggs, chicken/fish, paneer/tofu/tempeh, moong, masoor, chickpeas, rajma.
Pantry & swaps: besan, cornstarch, tapioca, GF tamari, tomato paste, coconut milk, tahini, seeds (chia/linseed), nuts, extra-virgin olive oil.
Spices: prefer single-ingredient spices; double-check blends for wheat fillers.
Treats & condiments: dark chocolate (check label), honey, nut butters, etc.
When deciding between brands, opt for those clearly marked “gluten-free,” which (in many regions) aligns with the <20 ppm standard; the FDA’s resources are concise and dependable: Gluten & Food Labeling and Gluten-Free Means What It Says.
Cross-Contact: The Invisible Gotcha (and How to Avoid It)
Even with perfect shopping, cross-contact can undo your efforts—especially if someone at home still eats gluten. Therefore:
- Divide utensils and surfaces: dedicate a toaster, cutting board, and strainer for GF foods.
- Handle flour carefully: airborne flour can linger; keep GF prep separate in time and space.
- Fryers and oil: avoid shared fryers; batter residues contaminate oil.
- Sauces and spreads: use squeeze bottles or separate knives; crumbs are sneaky.
These small systems are the backbone of a reliable gluten sensitivity diet at home.
Eating Out Without Anxiety (And Actually Enjoying It)
Restaurants vary widely in their knowledge and kitchen setup; cross-contact can happen in shared fryers, toasters, or chopping boards. Nevertheless, you can dine out more confidently by calling ahead, asking about separate prep areas, and clarifying sauces, marinades, and dessert toppings.
For discovery, use tools that crowdsource experience and certification. Apps like Find Me Gluten Free are a practical starting point, while the National Celiac Association’s restaurant resources can point you toward vetted venues and programs.
Troubleshooting Symptoms on a Gluten Sensitivity Diet (When You’re Still Not Feeling Great)
Sometimes, even after removing gluten, symptoms linger. In that case, consider a short, structured audit:
- Hidden gluten: re-check spice blends, sauces, and “natural flavors.” If in doubt, switch to single-ingredient spices and brands that explicitly label GF.
- Cross-contact: scrutinize toasters, fryers, wooden spoons, cutting boards, and baking trays.
- Oats tolerance: even certified GF oats can bother a subset of people; remove oats for 2–3 weeks and reassess. For background on why certified oats matter, read the CDF oats explainer above and the FDA labeling resources.
- FODMAP overlap: if gas, bloating, or pain are dominant, consider whether fructans and other FODMAPs might be the bigger trigger; Monash’s guidance is especially practical for this. See Monash on wheat/fructans.
- Nutrition review: check iron, B12, folate, vitamin D if fatigue persists—speak with your clinician about labs and tailored supplementation.
When in doubt, circle back to your clinician, share your food log, and refine from there.
Weight Loss—or Gain—on a Gluten Sensitivity Diet
Going gluten-free doesn’t automatically cause weight change; energy balance and satiety still rule. However, a gluten sensitivity diet that’s rich in protein, fiber, and minimally processed foods tends to stabilize appetite.
- If your goal is weight loss: base meals around protein (dal, chickpeas, tofu, fish/chicken) and high-fiber carbs (millets, quinoa), load up on vegetables, and keep sauces simple.
- If your goal is healthy weight gain: fold in energy-dense but nutrient-rich picks—tahini, nut butters, olive oil, avocado—and, for to find other great options for a weight gain diet, read our post on Best Weight Gain Foods for Fast, Healthy Gains.
Either way, consistency beats perfection; the plan you repeat wins.
Bringing It Together: Your Next Three Steps
- Finish testing (if pending), then commit: after proper screening, decide with your clinician whether you need a strict celiac protocol or a flexible gluten sensitivity diet. Start with the ACG’s overview and NIDDK’s testing guidance to feel confident in the process: ACG—Celiac Disease and NIDDK—Diagnosis.
- Stock your pantry and prep once: set up two grains, two legumes, and two sauces every weekend. For variety—especially at breakfast—lean on millets as a gluten-free superfood and customize with oats if you tolerate certified GF oats (use our oat primers on rolled vs old-fashioned and quick vs instant).
- Batch-cook and repeat favorites: pick two days from the 7-day plan and double them next week. Consequently, you’ll eat well without starting from scratch each evening.
Final Word (and Why This Works)
A gluten sensitivity diet doesn’t have to feel restrictive. Instead, by emphasizing naturally gluten-free foods, verifying labels, and building meals you actually enjoy, you can reduce symptoms while staying satisfied. Furthermore, the framework above keeps decisions simple: protein + fiber-rich carbs + plants + a little fat. Over time, that combination steadies digestion, improves energy, and makes “eating gluten-free” feel like a normal, delicious routine—not a medical chore.
And remember: your best plan is the one you’ll gladly follow. Start small, iterate weekly, and keep it tasty.
⚠️ Disclaimer: This article is for educational purposes only and is not medical advice. It does not diagnose, treat, cure, or prevent any condition. Always consult a qualified healthcare professional for personalized guidance, especially before starting a gluten sensitivity diet, changing medications, or interpreting tests. If you have urgent or severe symptoms, seek medical care immediately.
FAQs
1) What is a gluten sensitivity diet—and who needs it?
A gluten sensitivity diet is an eating pattern that removes gluten (proteins in wheat, barley, and rye) to reduce symptoms like bloating, brain fog, fatigue, and skin issues. It’s used by people with diagnosed celiac disease, suspected non-celiac gluten sensitivity (NCGS), or those advised by a clinician to trial gluten removal. Importantly, test for celiac disease before starting the diet to avoid false negatives.
2) What are the most common signs and symptoms of gluten intolerance?
Typical symptoms include abdominal pain, bloating, gas, diarrhea or constipation, nausea, headaches, brain fog, fatigue, and sometimes skin rashes. Additionally, some notice joint pain or mood changes. However, symptoms alone can’t confirm the cause—proper testing is key.
3) How is gluten intolerance different from celiac disease and wheat allergy?
Celiac disease is an autoimmune condition that damages the small intestine when gluten is eaten. NCGS causes symptoms without that autoimmune damage or IgE allergy markers. Meanwhile, wheat allergy is an IgE-mediated response to wheat proteins (not just gluten) and may involve hives, wheezing, or, rarely, anaphylaxis. Consequently, each requires a different management plan.
4) Which blood tests are used to check for celiac disease?
Common first-line tests include tTG-IgA plus a total IgA check. In certain cases (for example, young children), DGP antibodies may be used. Nevertheless, you must be eating gluten for a period before testing; otherwise, results may be inaccurate.
5) What does a strict gluten-free diet actually include?
Focus on naturally gluten-free foods: rice, millets (jowar, bajra, ragi), quinoa, potatoes, sweet potatoes, legumes, eggs, poultry, fish, meat, fruits, vegetables, and most dairy (if tolerated). Additionally, keep pantry swaps handy—GF pasta, chickpea flour (besan), cornstarch, tapioca, and gluten-free tamari.
6) Are oats gluten free?
Oats are naturally gluten-free; however, they’re often contaminated during farming or processing. Choose certified gluten-free oats and introduce slowly. A small subset of people may still be sensitive to avenin (oat protein), so monitor how you feel.
7) Is sourdough bread gluten free?
Regular wheat sourdough is not gluten-free, even though fermentation reduces some gluten. Only loaves made entirely with gluten-free flours and starters are safe on a gluten sensitivity diet.
8) Is quinoa gluten free—and is it a good substitute?
Yes. Quinoa is naturally gluten-free, high in protein, and versatile. Moreover, it cooks quickly and works in pulao, upma, salads, and warm bowls, making it a smart staple for beginners.
9) What about Ezekiel bread, spaghetti, and coffee?
Traditional Ezekiel bread (sprouted grains) contains wheat and is not gluten-free. Choose GF-labeled breads instead. As for spaghetti, select gluten-free versions made from rice, corn, quinoa, or legumes. Plain coffee is naturally gluten-free; flavored products may vary, so always check labels.
10) Can a gluten sensitivity diet be both gluten-free and dairy-free?
Absolutely. Many people also remove lactose or dairy to troubleshoot symptoms. Consequently, use alternatives like almond or coconut yogurt, lactose-free milk, or tofu/paneer swaps if tolerated. Still, prioritize balanced meals with protein, fiber-rich carbs, healthy fats, and plenty of vegetables.
11) How do I handle eating out or “gluten-free near me” situations?
Call ahead and ask about separate prep areas, dedicated fryers, and ingredient lists. Additionally, explain cross-contact (shared toasters, cutting boards, or oil) and request simple grilled or steamed options with sauces on the side. Ultimately, clear questions lead to safer plates.
12) What is cross-contact—and why does it matter so much?
Cross-contact happens when gluten-containing foods or crumbs touch gluten-free items. Even tiny amounts can trigger symptoms for sensitive individuals. Therefore, at home, keep separate toasters, strainers, cutting boards, and knives for GF foods; in restaurants, ask about shared fryers and prep surfaces.
13) Can a gluten sensitivity diet help with weight loss—or weight gain?
It can support either goal when you structure meals well. For weight loss, anchor plates around protein and high-fiber carbs (millets, quinoa) and keep sauces light. For healthy weight gain, add energy-dense options—nut butters, tahini, olive oil, avocado—while still avoiding gluten. Ultimately, consistency beats perfection.
14) Do I need supplements on a gluten-free plan?
Maybe. Some people benefit from iron, B12, folate, vitamin D, or calcium depending on labs and intake. However, don’t self-supplement blindly. Instead, review symptoms, diet quality, and testing with a healthcare professional for a tailored plan.
15) What are the effects of gluten sensitivity if I don’t change my diet?
You might experience ongoing GI issues, fatigue, headaches, or skin flare-ups. In celiac disease specifically, continued gluten exposure can damage the small intestine and affect absorption. Consequently, accurate testing and an appropriate dietary plan are essential.
16) Can millets and other traditional grains fit into a gluten sensitivity diet?
Yes—beautifully. Millets like jowar, bajra, and ragi are naturally gluten-free and fiber-rich. Additionally, they’re easy to batch-cook and pair well with dals, veggies, and lean proteins, keeping meals satisfying and diverse.
17) How do I start a beginner-friendly gluten-free meal plan?
Begin with a simple 7-day rotation: two grains (say, rice and millet), two legumes (moong/rajma), and two sauces (tahini-lemon and a GF tamari mix). Batch-cook on the weekend. Consequently, weeknights become quick assemblies—grain + protein + veg + sauce—in under 15 minutes.
18) Will going gluten-free help hypothyroidism or Hashimoto’s?
Some individuals report symptom improvements, but evidence is mixed. Nevertheless, if you have Hashimoto’s and persistent symptoms, discuss a supervised trial with your clinician—especially to ensure adequate nutrients (selenium, iodine, iron, vitamin D) and to avoid unnecessary restriction.
19) What’s the best gluten intolerance or sensitivity test I can take at home?
Home kits exist, yet they can’t replace clinical evaluation. Moreover, interpretation is tricky, and some tests aren’t validated for diagnosis. Ideally, coordinate testing with your clinician, remain on gluten beforehand, and follow up with appropriate confirmation if results are positive.
20) What does a “strict gluten-free diet” look like day to day?
It means avoiding wheat, barley, rye, and cross-contact—every day. Additionally, you’ll read labels for hidden gluten in sauces, spice blends, and processed foods; choose clearly GF-labeled items; and set up separate kitchen tools where needed. Ultimately, it becomes routine—and much easier than it sounds.