If you’ve been wondering whether mixing apple cider vinegar and cayenne pepper is actually worth doing, you’re not alone. The tart-meets-spicy combo pops up in kitchen lore, wellness routines, and the occasional bottled “cleanse.” However, beyond the buzz, there’s a slower, steadier story to tell—one about repeatable habits that make meals feel calmer, appetite feel friendlier, and energy feel a little more even. This guide gives you a simple ACV + cayenne drink, several variations you’ll genuinely enjoy, and a grounded explanation of what the research suggests (and what it doesn’t). It also folds in safety tips that protect your teeth and your gut, plus practical day-by-day ideas so the habit sticks.
Take a breath. Instead of chasing miracles, let’s build a ritual you’ll actually repeat.
Why people mix apple cider vinegar and cayenne pepper
To set the stage, it helps to know what’s in the glass. Apple cider vinegar (ACV) contains acetic acid, which in controlled settings can slow gastric emptying and blunt post-meal glucose spikes. Consequently, some people experience steadier energy and an easier time stopping at comfortable portions. Cayenne pepper, for its part, brings capsaicin and related capsinoids, compounds associated with a small thermogenic bump and, in several trials, a gentle reduction in perceived appetite. None of this makes the drink a magic bullet; nevertheless, it can become a before-meal cue that nudges you toward mindful pacing and balanced plates.
Taste matters, too. The sip is tangy and gently hot, which many find satisfying. As a result, they approach the next meal more calmly—often enough to shift portions down a notch without white-knuckling.
The everyday apple cider vinegar and cayenne pepper drink (base recipe)
Serves: 1 | Time: 2 minutes
- 250 ml (1 cup) warm or room-temperature water
- 1–2 tsp (5–10 ml) raw, unfiltered apple cider vinegar (with the “mother”)
- A pinch (1/16–1/8 tsp) ground cayenne pepper
- Optional: 1–2 Tbsp fresh lemon juice; 1–2 tsp honey or maple; a few thin slices of fresh ginger; a pinch of turmeric; or 1/8 tsp cinnamon
Method:
Pour the water first. Then add ACV, sprinkle in cayenne, and stir. Finally, fold in any add-ins and sip before or with a meal. Begin with 1 tsp ACV for a few days and notice how you feel.
Why this version works:
It’s fast, repeatable, and flexible. Moreover, it’s simple to tailor—more lemon on warm afternoons, a whisper of cinnamon when evenings cool, or ginger when you want something soothing yet bright.
Apple cider vinegar and cayenne pepper for weight loss: realistic expectations
Let’s keep this honest. Drinks don’t melt fat. Even so, certain sips can change how you approach food, and that’s where the leverage lives. Taken just before or with a meal, apple cider vinegar and cayenne pepper may help you feel satisfied sooner; consequently, portions often shrink gently without a sense of deprivation. Additionally, ACV’s acetic acid can smooth post-meal glucose waves—something many notice as fewer energy dips and less frantic snacking. Meanwhile, capsaicin’s heat adds a small thermogenic nudge.
That said, the effects are modest in the literature. Meta-analyses and randomized trials suggest that ACV and capsaicin can support small improvements across weight or waist measures over several weeks, particularly when the rest of the day—protein, fiber, movement, sleep—pulls in the same direction. If you want receipts, here are two plain-English starting points: a systematic review on ACV and body metrics in the journal Nutrients (systematic review on ACV) and a meta-analysis on capsaicin and weight outcomes in the British Journal of Nutrition (capsaicin meta-analysis).
When to sip the ACV and cayenne pepper drink (and how often)
Rituals stick when they’re simple. Many people sip the drink 10–15 minutes before lunch; others prefer it with a meal. Start with 1 tsp (5 ml) ACV in a full glass of water plus a tiny pinch of cayenne, once daily. After a week—if everything feels fine—move to 2 tsp (10 ml); later, if you wish, try 1 Tbsp (15 ml). Consistency matters more than bravado.
If an empty stomach feels harsh, place the drink alongside a meal. Comfort drives adherence; adherence shapes results.
Variations people actually stick with (since taste keeps habits alive)
Apple cider vinegar and cayenne pepper with lemon
When you want freshness, add 1–2 Tbsp lemon juice to the base. The flavor brightens immediately, and the sip begins to feel almost like a wellness mocktail. For a deeper dive into this duo—timing, tweaks, and flavor ideas—see Apple Cider Vinegar and Lemon Juice for Weight Loss.
Apple cider vinegar and cayenne pepper with honey
Sometimes, a touch of sweetness makes the ritual inviting. Stir in 1–2 tsp honey, taste, and adjust. It’s smoother and easier for beginners. Nevertheless, measure the honey so the drink stays light. For balanced, non-hype guidance, read Lemon, Cayenne Pepper, and Honey for Detox.
“Bragg-style” at home
Prefer the bottled vibe—ACV + lemon + cayenne + honey—but want control? Make it yourself. The ingredient lineup on Bragg Honey Cayenne Wellness Cleanse provides a useful taste map; afterward, dial sweetness to your preference and keep the drink well-diluted. For a quick check, here are straightforward ingredient references: Bragg’s product page and a neutral retailer listing like Good Eggs.
Ginger–turmeric comfort
On cooler evenings, add a few ginger slices and a pinch of turmeric; let it steep for three to five minutes so the aromatics bloom. If you want to understand how turmeric and ACV fit together more broadly, explore Turmeric and Apple Cider Vinegar for Weight Loss.
Cinnamon whisper
When you crave warmth without extra heat, whisk in 1/8 tsp cinnamon. Stir well—cinnamon clumps. For more spice-led kitchen tweaks, browse 10 Metabolism-Boosting, Fat-Burning, Weight-Loss Inducing Spices.
A day built around apple cider vinegar and cayenne pepper (without diet drama)
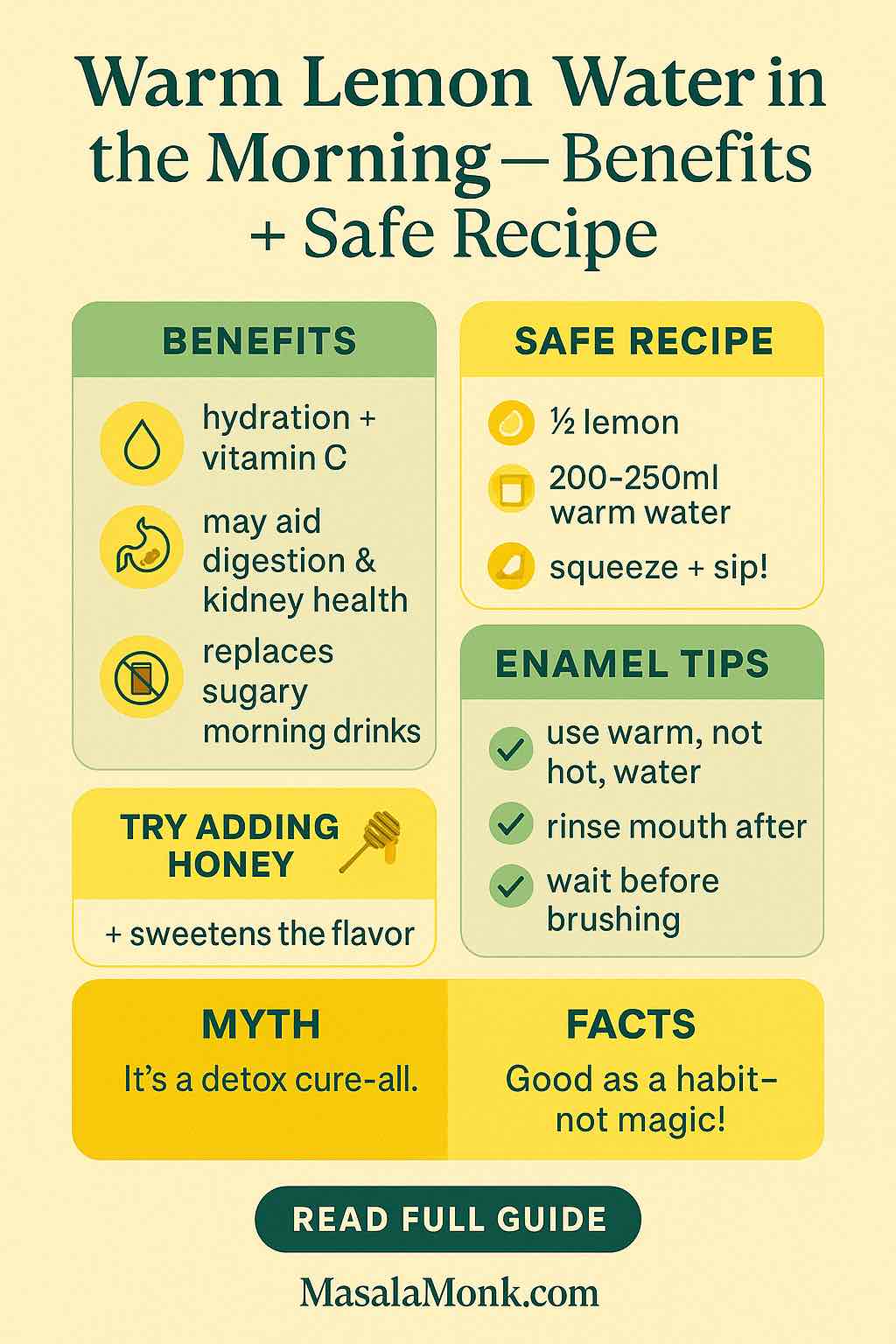
Morning: Hydrate first. If you already love warm lemon water, keep it; then slide your ACV drink closer to lunch.
Before lunch: Sip your apple cider vinegar and cayenne pepper drink. Build your plate around protein (eggs, curd/Greek yogurt, paneer/tofu, legumes, fish, or chicken) plus vegetables and fiber-rich carbs. Furthermore, season generously; flavor makes restraint easier.
After lunch: Take a short walk—ten to twenty minutes resets energy more than you’d expect.
Dinner: If appetite swells at night, begin with a salad dressed in an ACV vinaigrette to echo the theme while slowing the meal’s pace. On days you want variety, try switchel (a vinegar-ginger classic); the tradition feels old-school, yet it fits perfectly in modern kitchens.
Evening: Rinse with plain water after acidic drinks and wait 30–60 minutes before brushing so enamel can re-harden. Dental organizations and clinicians consistently recommend this timeline; for quick reads, see Mayo Clinic’s brushing-after-acid advice and a concise ADA newsroom explainer.
Apple cider vinegar and cayenne pepper benefits (tempered, practical, and honest)
Since nuance matters, here are the main points, calmly stated:
- Satiety & portions: With meals, ACV can help some people feel content with slightly less; over time, that can gently reduce calorie intake.
- Post-meal steadiness: By smoothing glucose spikes, ACV often translates to fewer crashes and steadier focus. For background, skim a short clinical overview of vinegar’s effect on postprandial glucose and a nutrition review abstract.
- Thermogenic nudge: Capsaicin’s heat effect is small yet real, especially with balanced meals and regular movement. For perspective, here’s a broad capsaicin review in addition to the meta-analysis above.
- Habit stack: Most importantly, the drink becomes a cue for better choices—protein, vegetables, and reasonable pacing. In practice, that’s where sustainable change comes from.
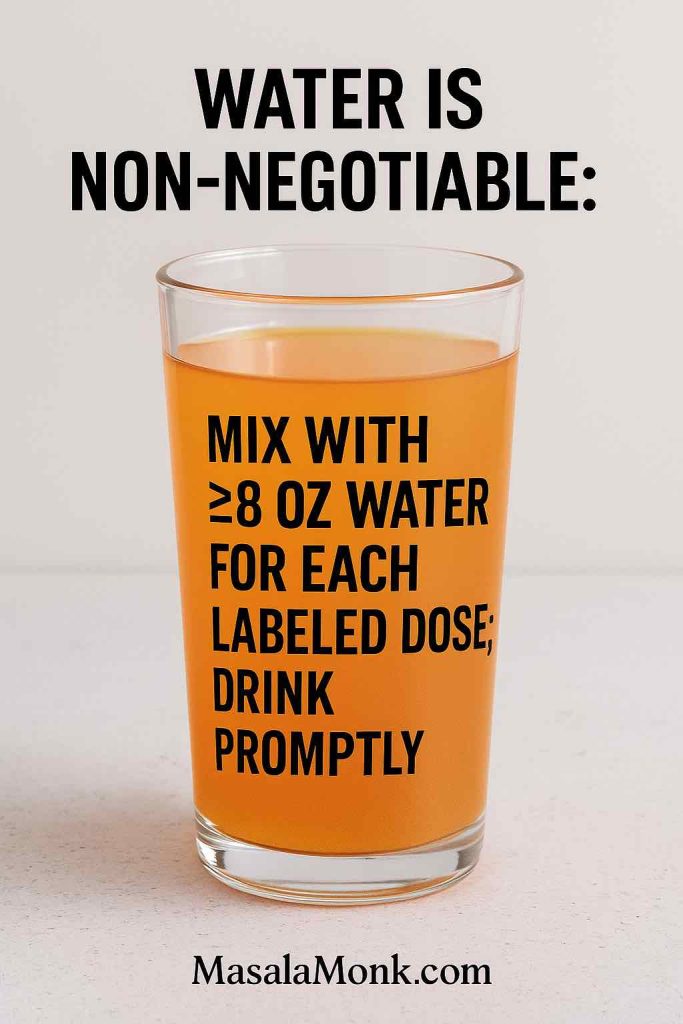
Safety first: how to enjoy ACV and cayenne while protecting teeth and digestion
ACV is acidic and cayenne is spicy; dilution is non-negotiable. In addition, consider a straw and always rinse with plain water afterward. Crucially, wait at least 30 minutes (up to an hour) before brushing so saliva can buffer acids and enamel can re-harden—guidance echoed by clinicians and dental groups (see the Mayo Clinic note and the ADA item once more).
If you have reflux, ulcers, or a sensitive stomach, place the drink with food, reduce the ACV amount, or skip the cayenne entirely. Moreover, if you use diuretics or diabetes medications, or you manage kidney disease, talk to your clinician about ACV’s potassium and glycemic effects. Personal thresholds vary; prudence keeps the habit comfortable.
Apple cider vinegar and cayenne pepper drink: recipes you’ll actually repeat
Although one size never fits all, the following options cover most palates:
Everyday base (unsweetened)
Water 250 ml + ACV 1–2 tsp + tiny pinch cayenne. Optionally, add lemon. Sip before or with a meal.
Gentle honey-lemon
Base + 1–2 tsp honey + 1–2 Tbsp lemon. Still dilute, still simple, noticeably smoother. For balancing sweetness and spice, here’s the internal guide: Lemon, Cayenne Pepper, and Honey for Detox.
Ginger-turmeric steam
Base + fresh ginger slices + pinch turmeric; let it sit three to five minutes. For broader context, read Turmeric and Apple Cider Vinegar for Weight Loss.
Cinnamon comfort
Base + 1/8 tsp cinnamon; whisk well to avoid clumps. For more spice-first strategies, skim Metabolism-Boosting Spices.
Beyond the glass: simple ways to make apple cider vinegar and cayenne pepper work in real life
- Lead with protein. Breakfasts built around eggs, yogurt, paneer/tofu, or dal steady appetite; evenings feel far less chaotic.
- Add fiber and color. Vegetables, pulses, whole grains, and fruit deliver fullness on fewer calories; as a result, the day feels more even.
- Walk after meals. Even brief strolls improve post-meal glucose; consequently, energy steadies.
- Keep rituals flexible. If mornings are rushed, move the drink to lunch. Conversely, if lunch is unpredictable, sip before dinner.
- Swap when needed. On days the drink doesn’t appeal, toss a salad with a bright ACV vinaigrette; the theme remains, the texture changes.
If you want a wider beverage bench, these sit nicely alongside your ACV habit: 5 Green Tea & Spice Infusions for Weight Loss and a friendly intro to switchel, the classic vinegar-ginger refresher.
What about bottled blends, pills, or gummies?
Convenience tempts everyone. Bottled ACV + lemon + cayenne + honey tastes familiar and travels well. Nevertheless, homemade versions let you adjust acidity and sweetness, which can be kinder to teeth and digestion, and they’re typically cheaper. For quick ingredient snapshots, cross-check the Bragg Honey Cayenne Wellness Cleanse or a neutral retailer page like Good Eggs.
As for pills or gummies, doses vary and labels aren’t standardized. Furthermore, some people report throat irritation from capsules. For these reasons, many prefer the drink for control and timing—especially when pairing it with meals rather than taking it in isolation.
Apple cider vinegar and cayenne pepper with lemon: where it shines
When brightness motivates you, the lemon variation really sings. Lemon’s aroma wakes the palate; you often pace yourself at the next meal. Additionally, vitamin C adds a small perk. For recipes and nuance, head to Apple Cider Vinegar and Lemon Juice for Weight Loss. If you enjoy morning rituals, pair that with The Morning Ritual: Warm Lemon Water—no need to force ACV on an empty stomach if that doesn’t suit you.
Apple cider vinegar and cayenne pepper with honey: when smoothness keeps you consistent
Not everyone loves sharp, unsweetened drinks. If a teaspoon or two of honey keeps you showing up, that’s a win. Measure it, taste, and adjust. Sustainability beats perfection every time. For more mix-and-match ideas, revisit Lemon, Cayenne Pepper, and Honey for Detox.
Bottom line
At the end of the day, apple cider vinegar and cayenne pepper can be a low-effort, high-consistency ritual. It’s quick to mix, easy to personalize, and grounded enough to respect your body’s pace. As you keep it diluted, sip it before or with meals, and give your teeth a little care, you may notice that meals feel calmer and energy feels steadier. From there, it’s much easier to make choices you’re proud of—day after day.
Ultimately, the habit is the hero. The drink is just how you start.
External sources
- Systematic review on ACV and body metrics (Nutrients): systematic review on ACV
- Capsaicin & weight meta-analysis (BJN): capsaicin meta-analysis
- Vinegar & post-meal glucose (open-access clinical overview): clinical overview of vinegar’s effect on postprandial glucose
- Dental enamel timing—rinse and wait: Mayo Clinic on brushing after acids, ADA press note
FAQs
1) Can I mix cayenne pepper with apple cider vinegar?
Absolutely. However, always dilute the combo in water. Start with 250 ml water + 1 tsp ACV + a tiny pinch of cayenne. Consequently, you’ll reduce enamel/gut irritation while keeping the flavor pleasant. If it’s too spicy, alternatively scale the cayenne down to a “dusting.”
2) Apple cider vinegar and cayenne pepper for weight loss—does it actually help?
Yes, but modestly. Moreover, the real benefit arrives when you pair the drink with protein-rich meals, fiber, movement, and sleep. Therefore, treat it as a helpful ritual, not a miracle.
3) What are the benefits of apple cider vinegar and cayenne pepper?
In brief: potential appetite control, smoother post-meal energy, and a small thermogenic nudge. Additionally, the habit itself cues mindful eating. Nonetheless, results build gradually over weeks, not days.
4) How to drink cayenne pepper for weight loss (timing and dose)?
Sip 10–15 minutes before a main meal (or with it). Begin with 1 tsp ACV in 250 ml water + a tiny pinch of cayenne once daily. Subsequently, if you tolerate it well after a week, increase to 2 tsp, and, if desired, later to 1 Tbsp.
5) Apple cider vinegar and cayenne pepper drink—what’s the simplest recipe?
Mix 250 ml water + 1–2 tsp raw ACV + a pinch of cayenne. Optionally, add lemon (1–2 Tbsp) or honey (1–2 tsp). Consequently, you’ll get a bright, sippable base you can repeat daily.
6) Apple cider vinegar, lemon and cayenne pepper—any extra advantages?
Lemon adds freshness and vitamin C; meanwhile, the core effects remain modest. Importantly, this variation tends to improve adherence because it tastes better, which ultimately matters most.
7) Apple cider vinegar, cayenne pepper and honey—is honey OK?
Yes—in moderation. However, honey adds calories, so measure 1–2 tsp. Alternatively, swap honey for a zero-calorie sweetener if you’re strictly counting.
8) What is the benefits of apple cider vinegar with lemon and cayenne pepper (as searched)?
Primarily, a tastier apple cider vinegar and cayenne pepper base with similar satiety and post-meal steadiness; plus, lemon’s aroma can slow your pace at meals. Nevertheless, keep expectations realistic.
9) Can this drink burn belly fat or “spot-reduce”?
No drink can target belly fat specifically. Instead, think whole-body change: consequently, consistent meals, steps, sleep, and this pre-meal ritual together move the needle.
10) Apple cider vinegar weight-loss recipe with cayenne pepper—what’s a friendly starter?
Try 250 ml water + 1 tsp ACV + a tiny pinch of cayenne + 1 Tbsp lemon. Subsequently, as tolerance grows, move up to 2 tsp ACV. If needed, 1 tsp honey can smooth the edges.
11) Apple cider vinegar and cayenne pepper drink with lemon—morning or night?
Either. However, if your stomach is sensitive in the morning, alternatively place it before lunch. Consistency, therefore, beats perfect timing.
12) ACV and cayenne vs pills/capsules—what’s better?
The drink is easier to titrate and pair with meals; moreover, it avoids some throat irritation reported with capsules. Capsules, meanwhile, are convenient but vary in dose/quality. Ultimately, choose what you’ll repeat.
13) Can I take apple cider vinegar and cayenne while fasting?
Plain ACV + water is very low-calorie; some fasting styles allow it. Honey, however, breaks a fast. Consequently, follow the rules of your chosen protocol.
14) Side effects of apple cider vinegar and cayenne pepper?
Undiluted ACV can affect enamel and the throat; cayenne can irritate reflux-prone stomachs. Therefore, always dilute, consider a straw, rinse with water afterward, and wait 30 minutes before brushing. Additionally, if you have GERD, ulcers, kidney disease, or take diuretics/diabetes meds, consult your clinician first.
15) ACV and cayenne pepper drink—can I use warm water?
Yes. In fact, slightly warm (not hot) water helps flavors meld. Nevertheless, avoid boiling water; it’s unnecessary and may taste harsh with ACV.
16) Apple cider vinegar and cayenne pepper with cinnamon—worth trying?
Definitely, if you enjoy warmth without extra heat. Add 1/8 tsp cinnamon; whisk well so it doesn’t clump. Alternatively, swap cinnamon for fresh ginger slices.
17) ACV, turmeric and cayenne pepper—is that combo fine?
Yes—start with a pinch of turmeric plus ginger slices. Meanwhile, let it steep 3–5 minutes for aroma. Consequently, many find this evening-friendly and soothing.
18) Apple cider vinegar and cayenne pepper drink—how long until results?
Give it 3–8 weeks alongside balanced plates and regular steps. Importantly, track appetite, portions, and energy rather than only the scale; progress, therefore, feels more obvious.
19) Can I mix apple cider vinegar and cayenne pepper with lemon water I already drink?
Sure. Moreover, it’s an easy habit stack: keep your lemon water ritual and, subsequently, fold ACV + a tiny pinch of cayenne into one serving per day.
20) How much cayenne is too much in an ACV drink?
Stay at a pinch (about 1/16–1/8 tsp). If you feel throat or gut irritation, consequently cut it in half—or skip cayenne and keep only ACV + lemon.
21) Apple cider vinegar and cayenne pepper drink recipe—can I batch-prep?
You can pre-mix ACV + water in a bottle (refrigerated) for 24 hours. However, add lemon, cayenne, or honey right before drinking; flavors and potency hold better that way.
22) ACV and cayenne pepper for weight loss—should I take it twice a day?
Once daily is sufficient for most. Nevertheless, if tolerance is good, you could split your usual ACV amount across two small pre-meal drinks. Ultimately, let comfort and consistency guide you.
23) Apple cider vinegar and cayenne pepper drink—does brand matter?
Choose raw, unfiltered ACV with the “mother.” As for cayenne, any reputable, fresh, bright-red ground cayenne works. Additionally, check best-by dates for potency.
24) Apple cider vinegar, cayenne pepper and lemon—can I sweeten without honey?
Yes. Alternatively, use a few drops of stevia/monk fruit, or even a thin apple slice muddled in the glass. Consequently, you’ll keep calories low while softening the tang.
25) Vinegar and cayenne pepper for weight loss—can I use white vinegar?
Technically yes, though apple cider vinegar is the focus here and tends to be gentler in flavor. If you swap, subsequently start at an even smaller dose and assess taste/tolerance.
26) Apple cider vinegar and cayenne—is a “shot” better than a drink?
No—avoid straight shots. Instead, always dilute in a full glass of water. Consequently, you’ll protect teeth and reduce throat discomfort while getting the same practical effect.
27) How do I scale the recipe without overdoing acid or heat?
Keep a simple ratio: per 250 ml water, use 1–2 tsp ACV + a pinch of cayenne. Moreover, if you want a larger glass (500 ml), simply double the water and lemon first; then, cautiously increase ACV.
28) Apple cider vinegar and cayenne pepper—which meal is best?
Whichever meal you overeat most. For many, that’s lunch. Alternatively, use it before dinner if evenings are your challenge. Therefore, align timing with the moment of highest payoff.
29) Apple cider vinegar and cayenne pepper benefits—will this affect my workouts?
Possibly. Some experience steadier energy and fewer cravings post-workout. Conversely, if spicy drinks bother you before training, simply have it with a different meal.
30) Final guide: what’s the smartest starting plan?
Week 1: 250 ml water + 1 tsp ACV + tiny pinch cayenne once daily before a main meal. Week 2: if comfortable, 2 tsp ACV. Meanwhile, keep meals protein-forward with veggies and fiber; add lemon for taste, and honey only if needed. Ultimately, consistency beats intensity.