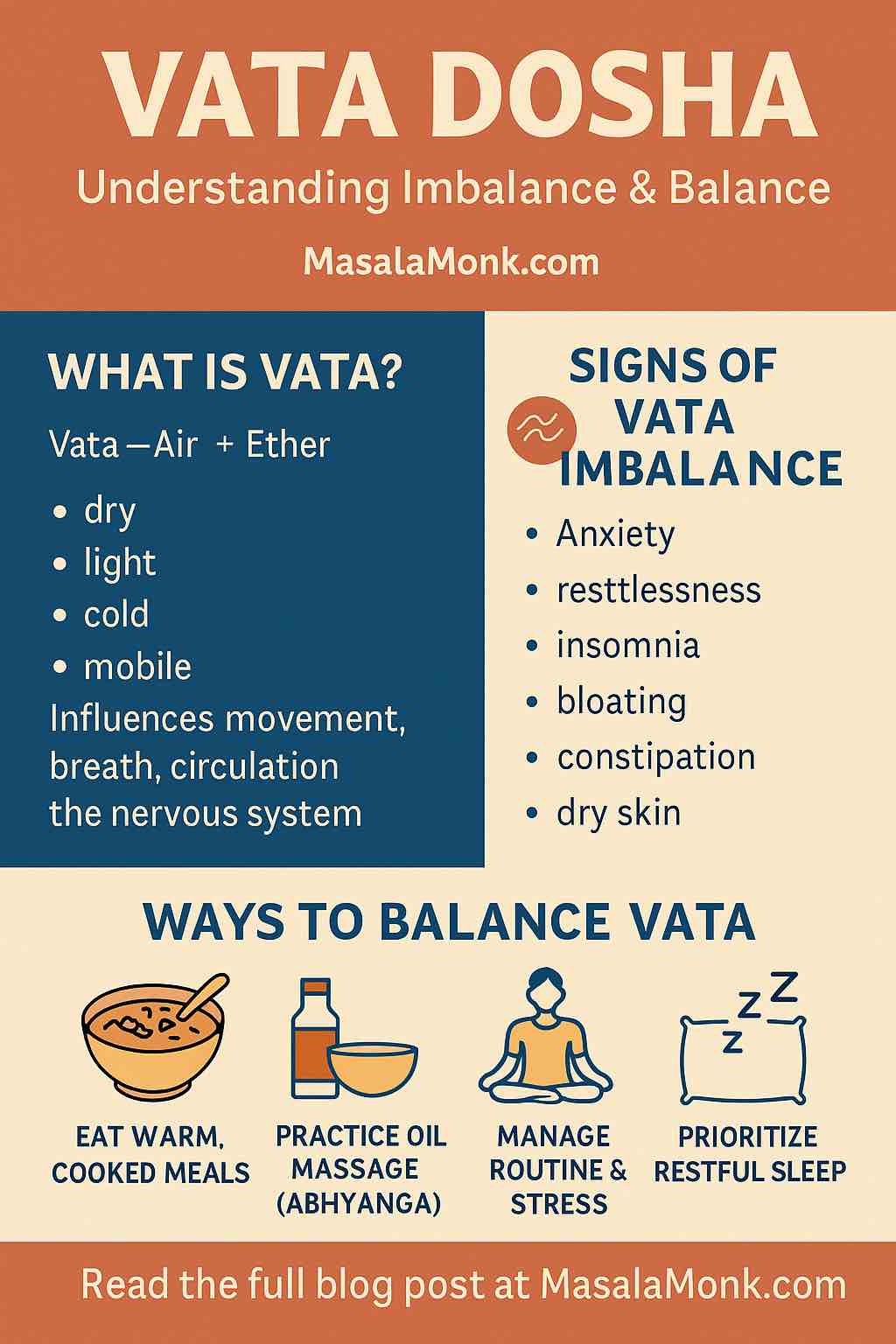
In today’s world of fast food, fast thoughts, and faster burnout, it’s no wonder that Vata dosha is often the first to fall out of balance. Whether you’re feeling scattered, anxious, bloated, or sleepless—chances are, Vata’s whisper has turned into a storm. But before you reach for another supplement or trendy detox, let’s take a deep, nourishing dive into what Vata really is—and how to bring it back into balance with grounded, time-tested (and practical) wisdom.
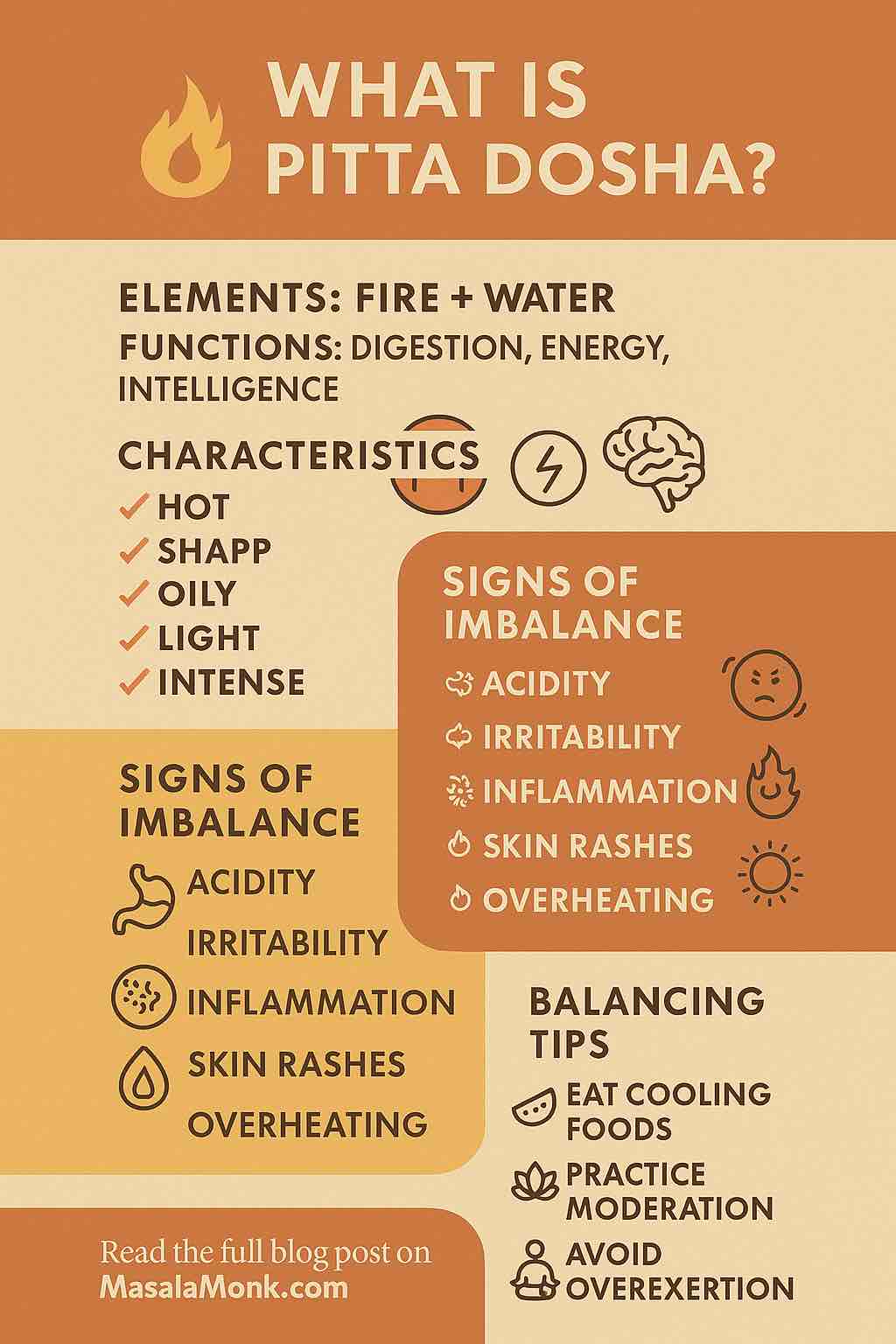
🧬 What is Vata Dosha?
In the Ayurvedic tradition, Vata is one of the three core doshas or energetic principles governing the body and mind. Composed of Air (Vayu) and Ether (Akasha), Vata is movement itself. It’s the force behind blinking, breathing, nerve impulses, creativity, speech, elimination, and even inspiration.
Vata in a Nutshell:
| Category | Description |
|---|---|
| Elements | Air + Ether |
| Qualities (Gunas) | Dry, light, cold, rough, mobile, subtle |
| Primary Site | Colon (large intestine), ears, skin, bones |
| Mental Traits | Quick, curious, imaginative, anxious |
| Physical Traits | Lean build, cold hands/feet, dry skin, restless |
🔍 Are You Vata-Dominant?
You’re likely Vata-predominant if you:
- Have bursts of energy followed by crashes
- Struggle with cold, dry weather
- Experience gas, bloating, or constipation
- Find it hard to focus or finish tasks
- Get anxious or overstimulated easily
- Have irregular appetite and sleep patterns
You might also be a mix (Vata-Pitta or Vata-Kapha), but even then, Vata is the most sensitive dosha—the one that goes off-track first and fastest.
🚨 Signs Your Vata is Out of Balance
When aggravated, Vata can manifest as:
Physical
- Constipation
- Dry skin, cracked lips
- Joint pain or stiffness
- Insomnia or light, fragmented sleep
- Cold intolerance
Mental
- Anxiety or panic
- Racing thoughts
- Inability to focus
- Restlessness or fidgeting
- Creative blocks or mental fatigue
The causes? Too much movement, overstimulation, travel, cold weather, erratic schedules, fasting, intense exercise, or even too much screen time.
✅ The Vata-Balancing Principle: Opposites Heal
Because Vata is dry, light, cold, irregular, mobile, and rough, we heal it using qualities that are:
Warm, moist, heavy, oily, stable, and smooth.
Let’s turn that principle into practical, doable routines.
🥣 Daily Practices to Balance Vata
1. 🌄 Morning Grounding Routine
- Wake up around 6:30–7:00 AM (no jarring alarms).
- Apply warm sesame oil to your body (Abhyanga). Leave it on for 20 minutes, then shower. This calms nerves and soothes dryness.
- Drink a cup of warm water with fennel or ginger to stimulate digestion gently.
- Practice 5–10 minutes of alternate nostril breathing (Nadi Shodhana) or humming breath (Bhramari).
“I never thought 10 minutes of breathing could change my day—but it does. I feel calmer, slower, more here.” – Reddit user
2. 🥘 Vata-Friendly Eating
| Focus On | Avoid |
|---|---|
| Warm, cooked meals | Raw salads, dry snacks |
| Root veggies & squashes | Cold or icy drinks |
| Healthy fats (ghee, avocado) | Excess caffeine or carbonated drinks |
| Soft grains (oats, rice) | Puffed, crunchy, or light foods |
| Mild spices (ginger, cinnamon, fennel) | Very spicy or astringent foods |
Simple Daily Meal Idea:
- Breakfast: Warm oatmeal with stewed apples, cinnamon, cardamom, and ghee
- Lunch: Rice + moong dal khichdi + ghee + sautéed carrots
- Dinner: Sweet potato soup + spiced buttermilk + soft roti
Pro Tip: Eat at consistent times, and never on the go. Sit, chew, breathe.
3. 🧘 Gentle Movement Over Intensity
Vata types often overdo exercise, leading to burnout or injury. Choose:
- Yin or restorative yoga
- Walking in nature
- Swimming (in warm water)
- Light tai chi or qigong
Avoid: high-impact cardio, cold-weather running, overtraining.
“I swapped HIIT for yoga and grounding walks. My knees stopped hurting. I finally started sleeping.” – User from r/Ayurveda
4. 🌙 Sleep Like It’s Sacred
Vata types are prone to light, restless sleep. Tips to restore sleep naturally:
- Go to bed before 10 PM
- Use warm oils on feet and ears before sleep (e.g., Brahmi oil)
- Play low-frequency binaural sounds or a calming mantra
- Avoid screens for 60 minutes before bedtime
- Chamomile or Ashwagandha tea in the evening helps calm racing minds
🌿 Vata-Pacifying Herbs (Safely Used)
These herbs can help nourish and calm Vata—but always consult an Ayurvedic practitioner before taking:
| Herb | Action |
|---|---|
| Ashwagandha | Adaptogen, sleep and energy balance |
| Brahmi | Calms nervous system, sharpens focus |
| Shatavari | Moistens tissues, especially in women |
| Licorice | Soothing, anti-inflammatory |
| Triphala | Supports regular, gentle elimination |
Choose teas, oils, or powders—avoid unregulated capsules.
🧭 A Sample Daily Vata-Balancing Schedule
| Time | Practice |
|---|---|
| 6:30 AM | Wake gently, warm water, oil massage |
| 7:00 AM | Light yoga + breathwork (Nadi Shodhana) |
| 8:00 AM | Warm breakfast (oats, ghee, nuts) |
| 12:30 PM | Main meal (heaviest, cooked, grounding) |
| 3:00 PM | Herbal tea, 10 min walk, screen break |
| 6:30 PM | Light dinner (soup, dal, root veggies) |
| 8:30 PM | Brahmi oil to feet, no screens, candlelight |
| 10:00 PM | Sleep |
🌍 Real User Voices: What Works Best
From Reddit, YouTube, and wellness blogs, Vata-dominant users say:
- “Warmth is everything.” – from food to lighting to emotions
- “Abhyanga changed my relationship with my body.”
- “Sleep was my weak spot. Cutting caffeine + regular meals fixed it.”
- “I’m no longer trying to keep up. I’m choosing slowness—and it works.”
🧠 Modern Insights: What Science is Catching Up To
- Vata imbalances correlate with nervous system dysregulation, anxiety, and IBS symptoms
- Emerging studies link Vata Prakriti to specific genetic patterns
- Warm oils (like sesame) have anti-inflammatory and nervous system calming effects
- Ashwagandha and Brahmi are clinically proven to reduce anxiety and improve sleep
🎯 Final Thought: It’s Not About Perfection, It’s About Rhythm
Vata thrives on consistency, nourishment, and slowness. But you don’t have to overhaul your life to find balance. Even small shifts—like eating warm breakfasts, taking 10 minutes to breathe, or oiling your feet before bed—can restore your inner harmony.
You are not broken. You are sensitive—and sensitivity, when respected, becomes strength.
🔍 FAQs on Cayenne Pepper for Weight Loss
1. How much cayenne pepper should I take daily for weight loss?
Start with 1/8 to 1/4 teaspoon per meal and gradually increase to 1/2 teaspoon if tolerated. Most studies show benefits from 2–6 mg of capsaicin per meal, which translates to around 1/2 teaspoon of cayenne powder daily.
2. Can cayenne pepper burn belly fat specifically?
While cayenne may aid in reducing overall body fat through increased metabolism and fat oxidation, it doesn’t target belly fat directly. However, some studies observed small decreases in waist circumference.
3. What time of day is best to take cayenne pepper?
There’s no strict timing, but using cayenne before or during meals can enhance satiety and thermogenesis. Many people add it to their morning drink or main meals for consistent intake.
4. Can I take cayenne pepper on an empty stomach?
It’s best to avoid it on an empty stomach if you’re prone to heartburn or digestive issues. Try adding it to meals to reduce irritation.
5. Are cayenne pepper supplements effective?
Yes. Capsaicin or capsinoid supplements can deliver benefits without the heat. Look for standardized extracts offering at least 6 mg capsaicin per dose. They’re especially useful if you dislike spicy foods.
6. How long does it take to see results with cayenne pepper?
Expect subtle changes over 4–12 weeks. Benefits like reduced appetite may be noticeable sooner, but weight and fat loss accumulate gradually with consistent use and a calorie-controlled diet.
7. Will I build a tolerance to cayenne’s effects?
Yes, thermogenic responses may decrease over time. Cycling off for a few days a week or using varied intake methods (e.g. food + supplements) may help retain sensitivity.
8. Can cayenne pepper interact with medications?
Yes. It can affect blood pressure meds, anticoagulants (e.g., warfarin), diabetes meds, and others. Consult your doctor before regular use if you’re on medication.
9. Is it safe to take cayenne pepper daily?
Generally safe in culinary amounts. For supplements or high doses, consult your healthcare provider, especially if you have GI issues, are pregnant, or nursing.
10. What are the side effects of taking too much cayenne?
Common side effects include stomach irritation, acid reflux, sweating, and, in rare cases, allergic reactions. Start with low doses and observe how your body reacts.