For centuries, cranberries have been cherished not only for their tart flavor and festive role in holiday dishes but also for their potential health benefits. Among these, their influence on kidney health has garnered significant interest in both the medical community and among health-conscious consumers. But how exactly do cranberries affect the kidneys? Are they a boon for urinary tract infections (UTIs) and kidney function, or do they come with hidden risks? Let’s explore the science, the myths, and the best practices around using cranberries for kidney health.
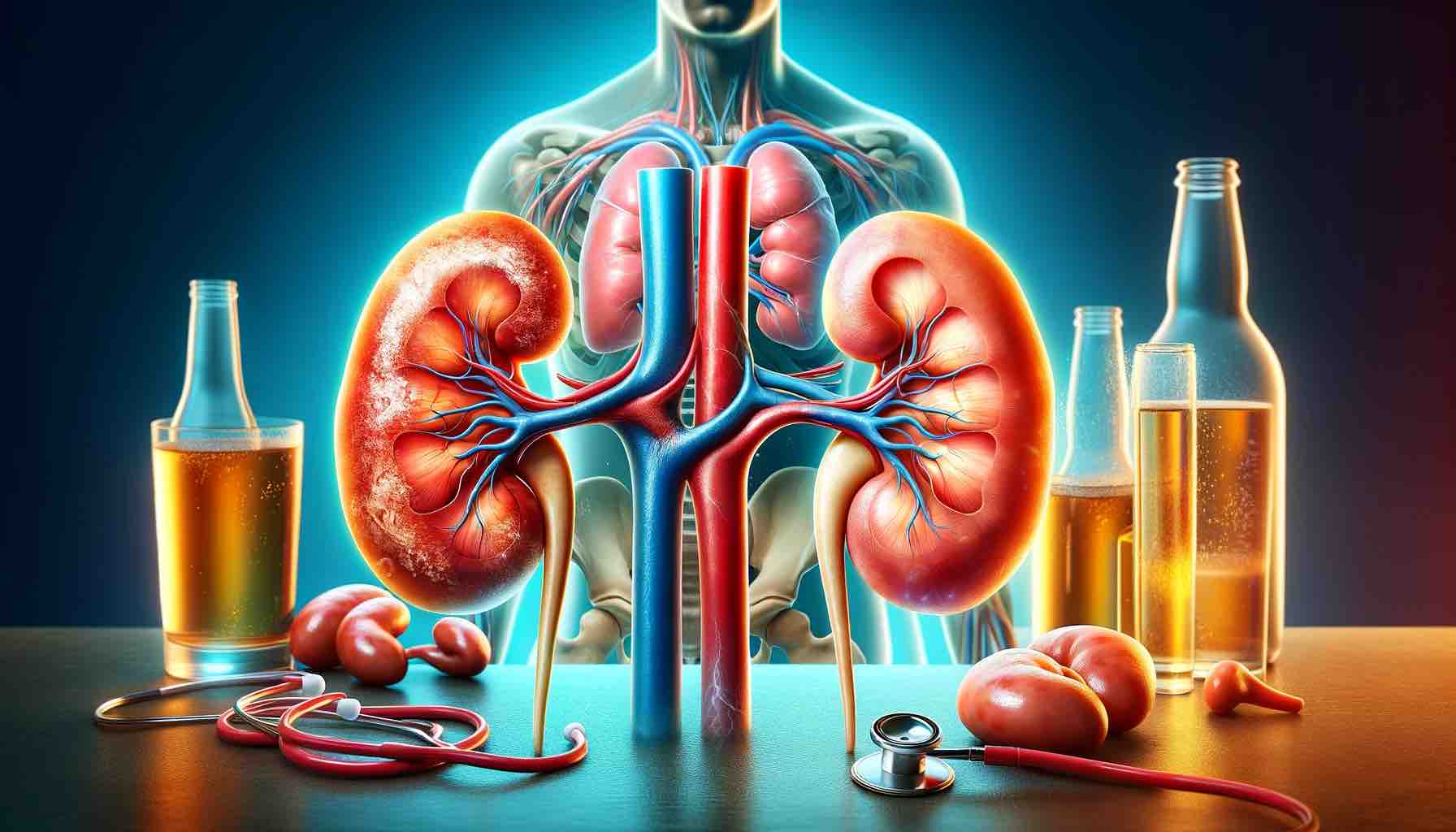
Understanding the Role of the Kidneys
Before we delve into cranberries, it’s crucial to understand what your kidneys do. These bean-shaped organs filter waste products from your blood, balance body fluids, regulate blood pressure, and produce hormones that influence red blood cell production and bone health. Any disruption in kidney function can lead to a cascade of health issues, so supporting kidney health is of paramount importance.
Cranberries and Urinary Tract Health: The Strongest Link
One of the most well-documented benefits of cranberries is their role in preventing urinary tract infections (UTIs). UTIs occur when harmful bacteria, primarily Escherichia coli (E. coli), attach to the lining of the urinary tract. Cranberries contain a type of polyphenol called proanthocyanidins (PACs), which prevent these bacteria from adhering to urinary tract walls.
By reducing the incidence of UTIs, especially in individuals prone to recurrent infections, cranberries may indirectly protect the kidneys. UTIs that travel upward from the bladder to the kidneys can cause more severe infections like pyelonephritis, which can damage kidney tissues over time. Hence, regular consumption of cranberry juice or supplements may serve as a preventative strategy.
Cranberries and Chronic Kidney Disease (CKD): An Anti-inflammatory Ally?
Chronic Kidney Disease (CKD) is often exacerbated by oxidative stress and systemic inflammation. Cranberries are rich in antioxidants, particularly flavonoids and other polyphenolic compounds, which have shown promise in reducing inflammation markers and neutralizing free radicals.
While research is still evolving, some animal and human studies suggest that incorporating antioxidant-rich foods like cranberries into the diet may help mitigate inflammation in CKD patients. However, more robust clinical trials are needed before definitive conclusions can be made.
The Flip Side: Risks of Cranberries for Kidney Health
Despite their benefits, cranberries aren’t universally safe for all kidney-related issues.
1. Oxalate Content and Kidney Stones: Cranberries contain oxalates, naturally occurring compounds that can contribute to the formation of kidney stones, particularly calcium oxalate stones. For individuals with a history of kidney stones or those prone to high urinary oxalate levels, excessive cranberry consumption could be problematic.
2. Drug Interactions: Cranberry juice and supplements can interact with medications, notably warfarin, a commonly prescribed blood thinner. Cranberries may enhance warfarin’s effects, increasing the risk of bleeding. Always consult a healthcare provider before adding cranberry products to your diet if you’re on medication.
3. Sugar Content in Processed Juices: Many commercial cranberry juices are loaded with added sugars, which can be harmful to people with diabetes or those managing CKD. High sugar intake can worsen metabolic conditions that already strain kidney function. Opt for unsweetened, 100% pure cranberry juice or capsules standardized for PAC content.
How to Safely Incorporate Cranberries into Your Diet
If you’re interested in leveraging cranberries for kidney or urinary health, consider these guidelines:
- Choose Wisely: Opt for unsweetened, organic cranberry juice or high-quality cranberry supplements.
- Mind the Dose: Limit juice intake to one cup per day unless otherwise advised by a healthcare provider.
- Watch for Symptoms: If you have a history of kidney stones, monitor for any signs of recurrence and speak to your doctor before regular cranberry use.
- Stay Hydrated: Drinking plenty of water helps flush the urinary system and supports overall kidney function.
Conclusion: A Balanced View on Cranberries and Kidney Health
Cranberries can be a powerful ally in promoting urinary tract health and potentially mitigating inflammation in kidney disease, but they are not a one-size-fits-all solution. Their high oxalate content and potential drug interactions mean they must be used thoughtfully, especially in individuals with existing kidney concerns.
As with many superfoods, the key is balance and personalization. Talk to your healthcare provider about your specific health needs and how cranberry products might fit into your wellness plan. When used wisely, cranberries can be a tart yet powerful ingredient in your journey to better kidney health.
Have you tried using cranberries for kidney health? Share your experiences or questions in the comments below!
Frequently Asked Questions (FAQs)
1. Can cranberries actually prevent kidney infections?
Cranberries can help prevent urinary tract infections (UTIs), which, if left untreated, may ascend and cause kidney infections like pyelonephritis. The proanthocyanidins (PACs) in cranberries prevent bacteria from sticking to the urinary tract walls, thereby reducing UTI risk.
2. Are cranberries good for people with chronic kidney disease (CKD)?
In moderation, cranberries may offer anti-inflammatory and antioxidant benefits that could support CKD management. However, they should be used with caution, especially due to their oxalate content, which could worsen certain conditions.
3. Is cranberry juice or cranberry supplements better for kidney health?
Both can be beneficial, but supplements standardized for PAC content often provide more consistent doses without added sugars. Choose what’s best based on dietary needs and doctor’s advice.
4. How much cranberry juice is safe to drink daily for kidney support?
Generally, one cup (8 oz or ~240 mL) of unsweetened cranberry juice per day is considered safe for most people. Always consult a healthcare provider for personalized recommendations.
5. Can cranberries help dissolve kidney stones?
No, cranberries cannot dissolve existing kidney stones. In fact, due to their oxalate content, they may contribute to the formation of calcium oxalate stones in susceptible individuals.
6. Are dried cranberries a good alternative for kidney health?
Dried cranberries can offer some benefits, but they often contain added sugars and are less effective for UTI prevention due to lower PAC content. Look for unsweetened versions if consumed regularly.
7. Should people with kidney stones avoid cranberries?
People with a history of calcium oxalate kidney stones should limit or avoid cranberries, as they are high in oxalates that can contribute to stone formation.
8. Can I take cranberry supplements while on medication?
Some cranberry products may interact with medications like warfarin (a blood thinner). Always speak with your doctor before starting supplements if you’re on any prescribed medications.
9. What type of cranberry juice is best for kidney health?
Choose 100% pure, unsweetened cranberry juice without added sugars or artificial ingredients. Organic options are ideal for minimizing exposure to pesticides.
10. Can children or pregnant women use cranberries for urinary health?
Cranberries are generally safe in moderate amounts, but dosage should be adjusted for children. Pregnant women should consult a healthcare provider before using cranberry supplements.