Insulin resistance (IR) is often a silent disruptor. It doesn’t knock on the door with loud alarms. Instead, it tiptoes in, masked as fatigue, stubborn belly fat, cravings, or skin changes. Before you know it, it’s wreaking havoc on your metabolism, hormones, and energy levels. But here’s the good news: insulin resistance is manageable, reversible, and you are not alone. This post blends science, real-world experiences, and actionable strategies to help you understand, detect, and fight back against IR.
Section 1: What is Insulin Resistance? Insulin is a hormone produced by the pancreas that helps glucose (sugar) enter your cells for energy. When cells stop responding properly to insulin, the body compensates by producing more. This is insulin resistance. Over time, elevated insulin can lead to prediabetes, type 2 diabetes, PCOS, non-alcoholic fatty liver disease (NAFLD), and even cardiovascular issues.
Think of it like a broken lock: insulin is the key, and your cells are the door. If the lock is rusty (insulin resistant), you need more keys (insulin) to get in.
How It Progresses:
- Phase 1: The body compensates by producing more insulin. Blood sugar stays normal.
- Phase 2: Pancreas can’t keep up. Blood sugar starts to rise (prediabetes).
- Phase 3: Chronic high glucose leads to type 2 diabetes and systemic inflammation.
Symptoms to Watch For:
- Constant fatigue or energy crashes, especially after meals
- Intense cravings (especially for carbs or sugar)
- Abdominal weight gain that won’t budge
- Brain fog and difficulty concentrating
- Skin tags or dark patches (acanthosis nigricans)
- Frequent hunger, even after eating
- Irregular periods or PCOS symptoms in women
- Erectile dysfunction in men
- High triglycerides or low HDL (“good”) cholesterol
- Increased urination and thirst
- Blurred vision and slow wound healing
Section 2: Real Stories, Real Struggles
Bekind123456789 shared on Reddit: “I completely reversed my insulin resistance over six months. I wore a continuous glucose monitor (CGM), gave up added sugars, ate three balanced meals a day, and did strength training twice a week. I lost 63 pounds and dropped my HOMA-IR from 6.2 to 1.9.”
Another user, battling PCOS, described eating as little as 1000 calories a day with no weight loss, extreme fatigue, cravings, and skin tags. Her turnaround came with myo-inositol supplements, a Mediterranean-style diet, and daily 30-minute walks.
A third user, frustrated by slow progress with Mounjaro (a GLP-1 drug), opted for bariatric surgery, citing insulin resistance as the major blocker to fat loss and energy restoration.
Others shared how IR was misdiagnosed as chronic fatigue syndrome or depression, delaying proper treatment. Many described the emotional toll of feeling dismissed by doctors despite obvious metabolic dysfunction.
These stories share a common theme: frustration, self-discovery, persistence, and ultimate improvement through lifestyle change.
Section 3: Diagnosis and Labs
While symptoms give you clues, labs confirm the story. Ask your doctor for:
- Fasting insulin and glucose (calculate HOMA-IR: Insulin x Glucose / 405)
- A1C (reflects 3-month average glucose)
- Lipid profile (check triglycerides, HDL, LDL)
- High-sensitivity CRP (inflammation marker)
- Liver enzymes (for fatty liver assessment)
- Fasting C-peptide (insulin production indicator)
Interpreting Results:
- Fasting insulin > 10 uIU/mL: potential IR
- HOMA-IR > 2.0: insulin resistance likely
- Triglyceride/HDL ratio > 2.0: metabolic dysfunction risk
- Elevated ALT/AST: possible fatty liver
Even with a “normal” A1C or glucose, IR can exist. Always consider insulin levels and inflammation.
Section 4: Practical Recovery Framework
1. Nutrition: Prioritize Protein and Fiber
- Build meals around protein: eggs, fish, tofu, lean meats, legumes
- Add fiber-rich vegetables: leafy greens, broccoli, cauliflower
- Swap refined carbs for whole grains and root vegetables
- Reduce added sugars and sweetened beverages
- Include healthy fats: olive oil, avocado, nuts, seeds
Sample Day of Eating:
- Breakfast: Omelet with spinach and mushrooms, side of berries
- Lunch: Grilled salmon salad with olive oil vinaigrette
- Snack: Greek yogurt with chia seeds
- Dinner: Stir-fry with chicken, broccoli, and cauliflower rice
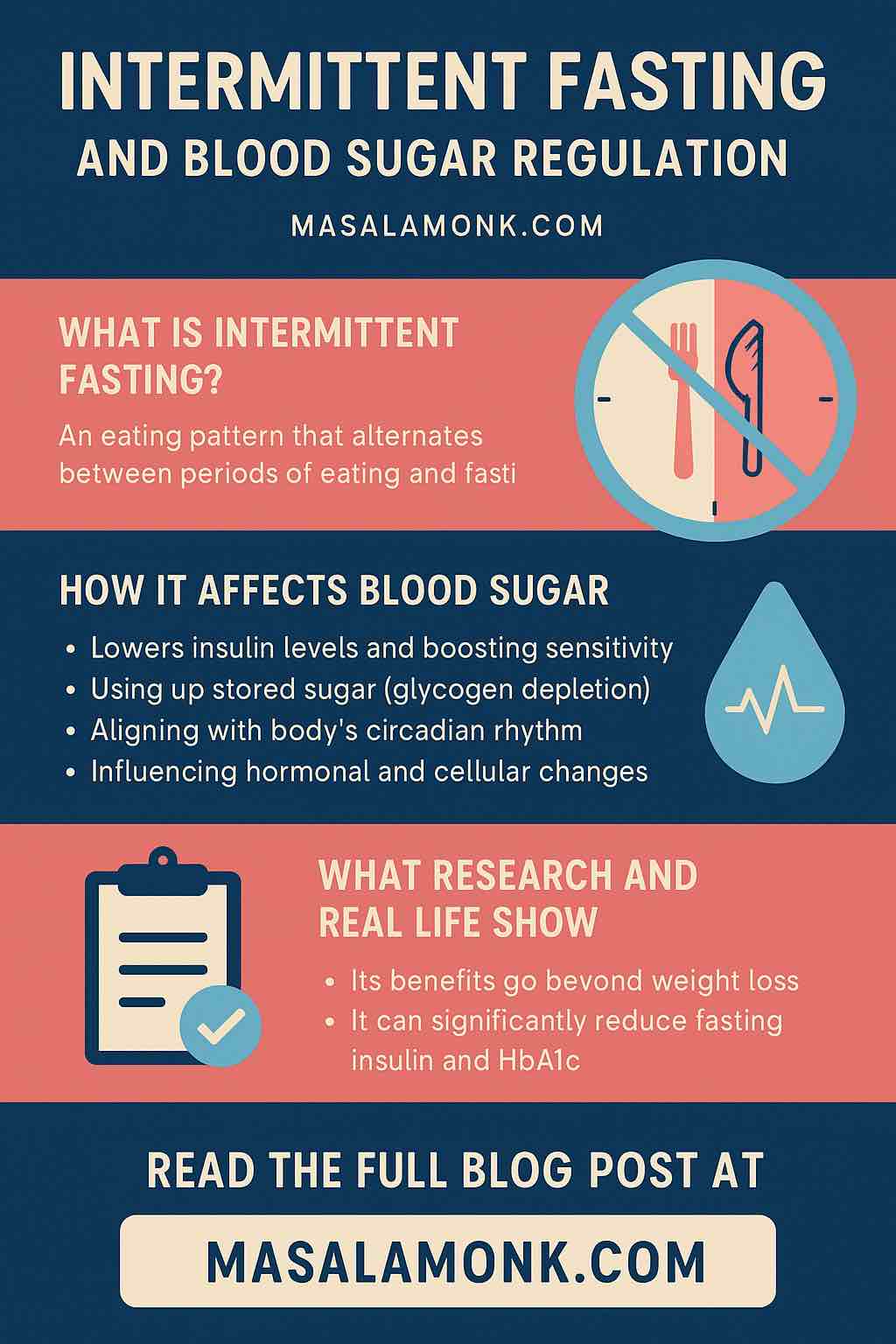
2. Time Your Eating: Intermittent Fasting (IF)
- Start simple: 12:12 or 14:10 eating windows
- Avoid constant snacking, especially at night
- Give your insulin levels time to reset between meals
- Consider early time-restricted feeding (eating earlier in the day)
3. Movement: Walk, Lift, Repeat
- Aim for 7,000–10,000 steps daily
- Strength training 2–3x per week builds muscle and improves insulin sensitivity
- Post-meal walks (even 10 minutes) reduce glucose spikes
- Include mobility work and stretching to reduce cortisol
4. Track and Reflect
- Use CGMs or glucometers to learn your body’s response to food
- Track meals, symptoms, energy levels, and sleep
- Celebrate non-scale victories: energy, mood, cravings, sleep
- Monitor progress every 3–6 months with lab work
5. Sleep and Stress
- Aim for 7–9 hours of quality sleep
- Reduce blue light at night, follow a consistent sleep schedule
- Practice mindfulness: breathwork, journaling, yoga, nature walks
- Chronic stress raises cortisol, which worsens IR and cravings
6. Supplements and Medications (when needed)
- Metformin: helps reduce glucose production in the liver
- Berberine: natural supplement with similar effects to metformin
- Myo-inositol and D-chiro-inositol: helpful for PCOS-related IR
- Magnesium, vitamin D, omega-3s: support glucose metabolism
- Always consult a professional before starting supplements
Section 5: The Mindset Shift This journey is not about perfection. It’s about awareness, experimentation, and consistency. Expect plateaus, setbacks, and learning curves. Listen to your body, seek community support, and stay curious.
Break free from diet culture traps. This isn’t about punishment or restriction. It’s about nourishing your body, managing stress, and choosing long-term health over short-term comfort.
As one Redditor put it: “At first, I felt betrayed by my body. Now, I see IR as a teacher. It forced me to care for myself.”
Conclusion: Reclaiming Your Health Insulin resistance doesn’t have to define your life. Armed with knowledge, support, and practical tools, you can rewrite your metabolic story. This isn’t a sprint. It’s a lifelong relationship with your body.
Track your progress. Stay consistent. Celebrate every small win. And remember: reversal is not only possible—it’s already happening for thousands. You can be next.
Have questions or a story to share? Drop a comment. Let’s heal together.
FAQs
1. What causes insulin resistance in the first place?
Insulin resistance is often caused by a combination of poor diet (especially excess sugar and refined carbs), sedentary lifestyle, chronic stress, poor sleep, excess visceral fat, and genetic predisposition. Hormonal conditions like PCOS can also contribute.
2. Can insulin resistance occur if my blood sugar levels are normal?
Yes. Many people have normal fasting glucose or A1C but elevated insulin levels. This is why checking fasting insulin and calculating HOMA-IR is critical for early detection.
3. Is weight gain inevitable with insulin resistance?
No, but weight gain—especially around the abdomen—is common. Insulin is a storage hormone, and when levels remain high, it encourages fat storage. However, with lifestyle changes, this trend can be reversed.
4. How long does it take to reverse insulin resistance?
Recovery varies. Some people see improvements in 3–6 months, while others may need longer depending on severity, consistency, and coexisting conditions like PCOS or NAFLD.
5. Do I need to follow a strict keto diet to improve IR?
Not necessarily. While some benefit from keto or low-carb, others improve with moderate carbs, high fiber, and prioritizing whole foods, protein, and healthy fats. Personalization is key.
6. What’s the difference between insulin resistance and type 2 diabetes?
Insulin resistance is a precursor to type 2 diabetes. In IR, insulin is high but blood glucose is often still normal. In diabetes, the pancreas can no longer keep up, and blood glucose rises significantly.
7. Should I use a continuous glucose monitor (CGM)?
If accessible, CGMs can be a powerful tool to learn how your body responds to specific meals, sleep, and stress. They’re especially helpful for biofeedback and meal timing strategies.
8. Are supplements enough to reverse insulin resistance?
Supplements like berberine or inositol can help, especially for PCOS. But they work best when paired with lifestyle changes such as movement, diet, sleep, and stress reduction.
9. Is insulin resistance reversible at any age?
Yes. While IR becomes more common with age, people in their 30s, 40s, 50s, and beyond have successfully reversed it through consistent lifestyle changes.
10. What’s the first thing I should do if I suspect I have IR?
Start by getting tested: request fasting insulin, glucose, and lipid profile from your doctor. Begin walking daily, reduce added sugars, and build meals around protein and fiber while you wait for results.