For people living with diabetes, managing blood sugar levels is a daily priority. Naturally, questions arise about whether fruits—which contain sugar—can be safely included in a diabetes-friendly diet. The answer is a resounding yes with a few smart considerations.
In this in-depth post, we tackle the most frequently asked questions about diabetes and fruit consumption, bust common myths, and share science-backed tips to enjoy fruit safely and deliciously.
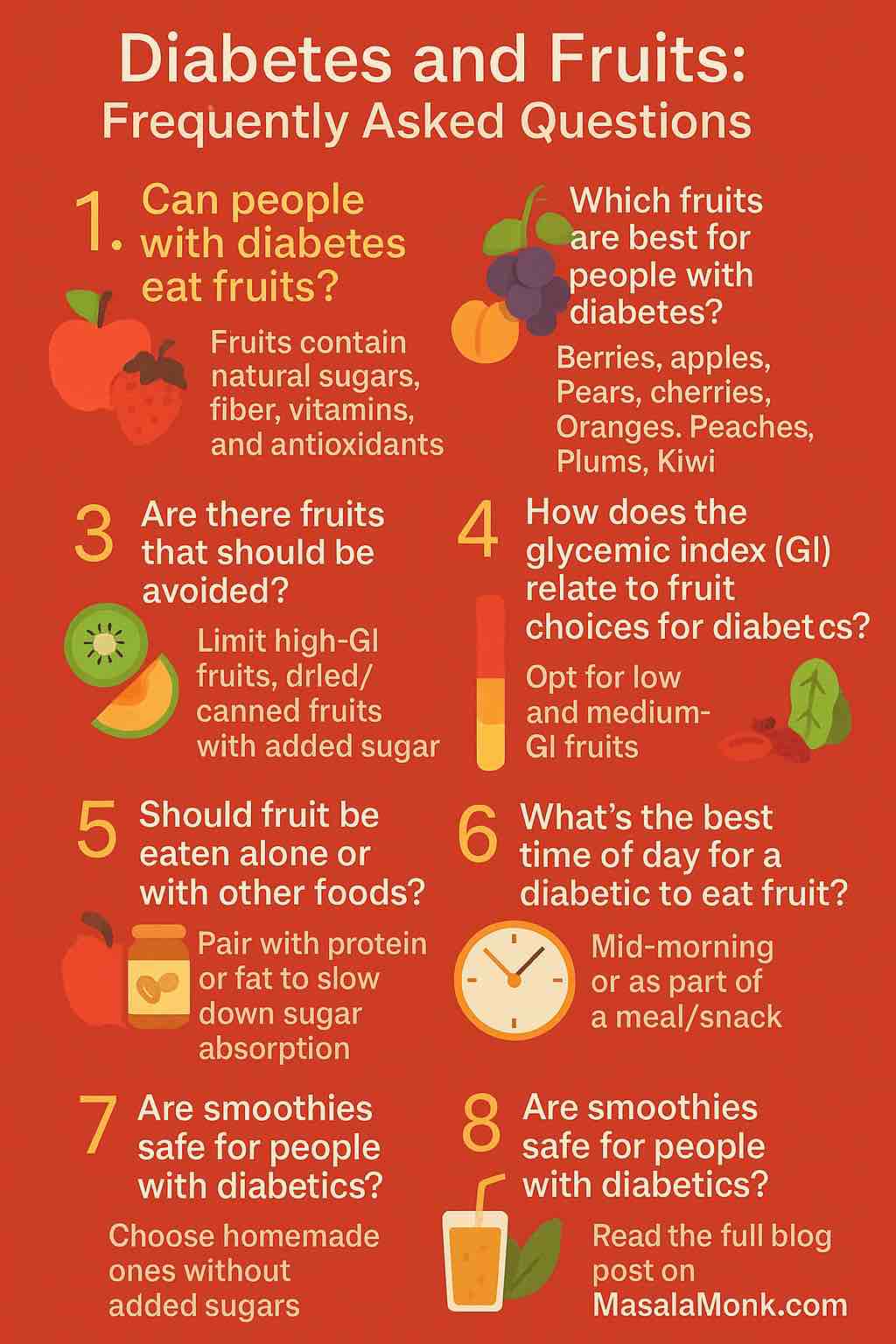
1. Can People with Diabetes Eat Fruits?
Yes. Whole fruits contain natural sugars along with essential nutrients like fiber, antioxidants, and vitamins. The fiber in fruit helps slow down the digestion and absorption of sugar, preventing sharp spikes in blood glucose levels.
Several large cohort studies and meta-analyses have shown that people who regularly consume fruit have a lower risk of developing type 2 diabetes. In people with existing diabetes, moderate fruit intake does not worsen glycemic control when part of a balanced diet.
2. Which Fruits Are Best for Blood Sugar Control?
Focus on fruits that are:
- Low to medium glycemic index (GI): These release sugar more slowly into the bloodstream.
- High in fiber: Helps regulate digestion and sugar absorption.
- Rich in nutrients: Support overall health.
Top picks for diabetics:
- Berries (blueberries, raspberries, strawberries): Low GI, high fiber, rich in antioxidants.
- Apples and pears: High fiber, especially with skin.
- Citrus fruits (oranges, grapefruit, kiwi): Vitamin C and soluble fiber.
- Peaches and plums: Low to medium GI, satisfying.
- Cherries: Low GI, anti-inflammatory properties.
3. Are There Fruits That Should Be Limited or Avoided?
No fruit is off-limits, but moderation and portion control matter. Fruits with high GI or high natural sugar content can be enjoyed occasionally and in smaller amounts.
Fruits to limit:
- Overripe bananas
- Watermelon (high GI, though low calorie)
- Pineapple
- Mangoes
- Dried fruits (raisins, dates, figs)
- Fruit juices (even 100% juice can spike glucose)
- Canned fruits in syrup
4. What Is the Glycemic Index and Why Does It Matter?
The glycemic index (GI) ranks how quickly a food raises blood sugar levels. Lower GI values mean slower glucose absorption.
| GI Range | Effect on Blood Sugar | Examples |
|---|---|---|
| Low (<=55) | Gradual increase | Apples, berries, cherries |
| Medium (56-69) | Moderate increase | Bananas, peaches, grapes |
| High (>=70) | Rapid increase | Watermelon, pineapple |
Low GI fruits are generally the most favorable for people with diabetes.
5. What Is the Right Portion Size for Fruits?
A common guideline is that 1 serving of fruit equals ~15 grams of carbohydrates.
Examples of 1 serving:
- 1 small apple or orange
- 1/2 banana
- 3/4 cup berries
- 1 cup melon or papaya
- 17 small grapes
Spread fruit servings throughout the day and include them as part of meals or balanced snacks.
6. Should You Eat Fruit Alone or With Other Foods?
For better blood sugar control, pair fruits with protein or healthy fat to slow down sugar absorption. This reduces glucose spikes and increases satiety.
Smart pairings:
- Apple with almond butter
- Berries with Greek yogurt
- Pear slices with cheese
- Banana with chia seeds and peanut butter
7. What About Smoothies?
Smoothies can be healthy or harmful, depending on how they are made.
To make diabetes-friendly smoothies:
- Use whole fruits, not juice.
- Add leafy greens like spinach or kale.
- Include a protein (like Greek yogurt or protein powder).
- Add a source of healthy fat (chia seeds, avocado, nut butter).
- Avoid adding honey, syrups, or sweetened yogurts.
Portion control is still key: even healthy smoothies can be high in carbs.
8. Do Dried Fruits or Fruit Juices Work?
Dried fruits are highly concentrated in sugar and calories. Just a small handful can exceed 30 grams of carbohydrates. While they contain fiber and nutrients, they’re best limited.
Fruit juices, even 100% natural, lack fiber and cause rapid spikes in blood sugar. It’s better to consume the whole fruit instead.
If you must include dried fruits or juices:
- Measure exact portions
- Combine with protein/fat
- Use them strategically (e.g., pre-exercise)
9. Are Tropical Fruits Like Mangoes or Bananas Off Limits?
Tropical fruits can still be enjoyed in small, controlled portions. Choose less ripe versions when possible, as ripeness increases sugar content and GI.
Example servings:
- 1/2 medium mango
- 1/3 to 1/2 banana
- 1/2 cup pineapple
Balance them with other macronutrients and avoid eating them alone.
10. When Is the Best Time to Eat Fruit?
The best times to eat fruit are:
- Mid-morning or mid-afternoon snacks
- Before or after moderate exercise
- As part of a balanced meal
Avoid eating large amounts of fruit:
- On an empty stomach
- Late at night, especially without other foods
Timing helps prevent blood sugar spikes and optimize nutrient absorption.
11. How Much Fruit Can a Person with Diabetes Eat Daily?
Most people with diabetes can safely eat 2 to 3 servings of whole fruit per day depending on their carb allowance, medication, and activity level.
Personalized meal planning with a dietitian or diabetes educator can help determine your optimal fruit intake.
Final Thoughts: How to Enjoy Fruit Without Fear
Fruits are a vital part of a nutritious, balanced diet—even for people with diabetes. The key is to:
- Choose low-GI, high-fiber fruits
- Watch portion sizes
- Pair fruit with protein or fat
- Avoid sugary juices and processed fruit products
- Integrate fruit into a structured meal plan
With these practical strategies, you can confidently enjoy nature’s sweetest foods while keeping your blood sugar in check.