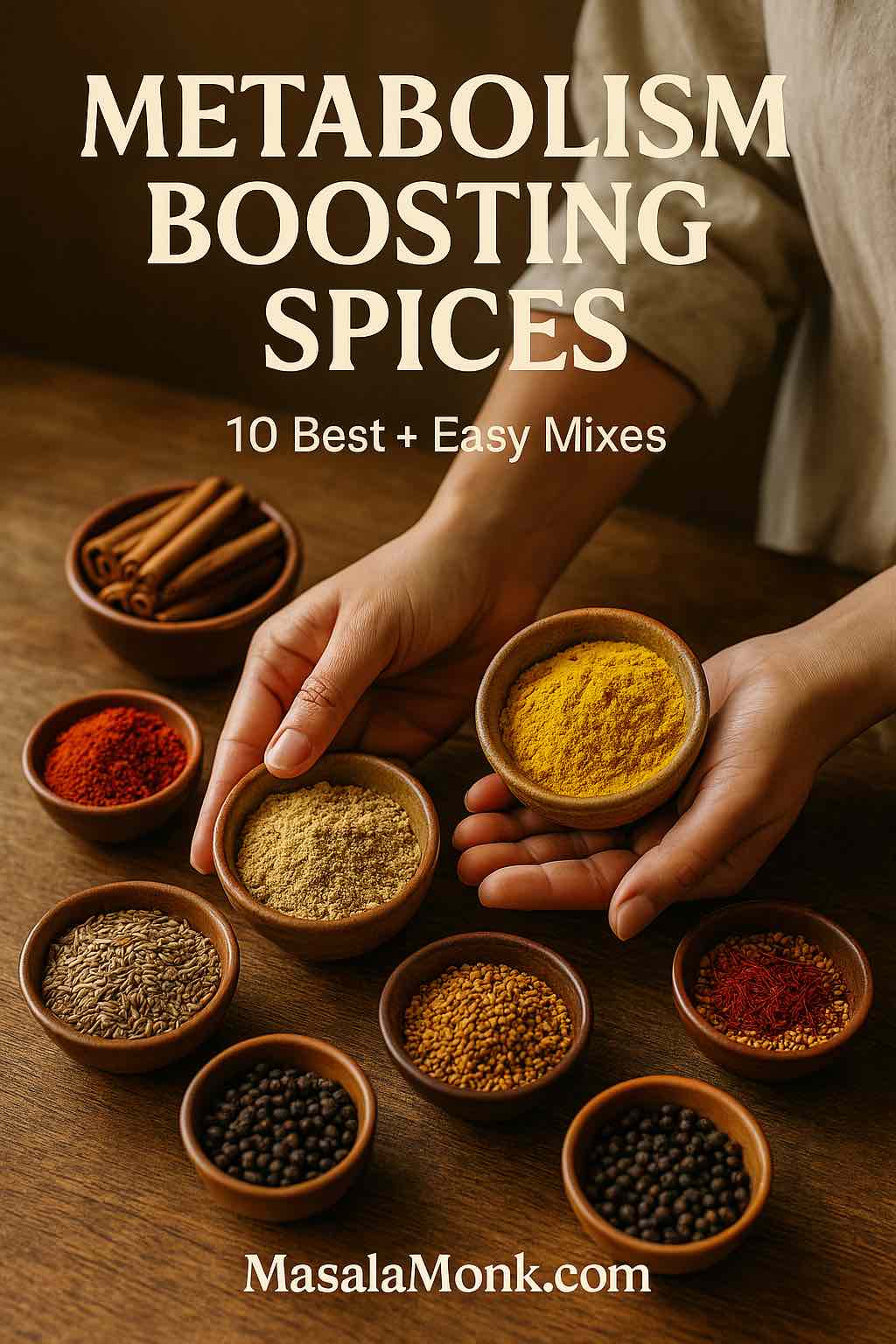
Sometimes the smallest changes do the most. Metabolism boosting spices won’t remake a meal on their own; however, they can gently steady appetite, nudge post-meal thermogenesis, and smooth out energy across the day. When you season consistently—and when you pair flavor with simple routines—those quiet nudges begin to add up. Moreover, you’ll find they slot into foods you already enjoy, which means adherence feels natural rather than forced.
How metabolism boosting spices actually help
To begin with, think of spices as adjustable dials rather than switches. Some, like cayenne, appear to slightly increase energy expenditure after eating; others, like cinnamon, help blunt post-meal glucose bumps; still others, like fennel and saffron, tend to soften snack impulses. In other words, these aren’t fireworks; they’re guardrails. Furthermore, a pinch at breakfast, another at lunch, and something warm in the evening often leads to fewer crashes, fewer “is there anything sweet?” moments, and—eventually—more predictable days.
Cayenne (Capsaicin): a warm spark among metabolism boosting spices
There’s a particular magic to cayenne: a little warmth, a little color, and suddenly a simple plate feels vibrant. Within the world of metabolism boosting spices, cayenne earns its place because a tiny pinch can lift thermogenesis without requiring you to set your tongue on fire.
Use it today. Stir ⅛–¼ teaspoon into scrambled eggs; alternatively, whisk a pinch into lemon-ginger tea on cool mornings; or dust roasted carrots, sweet potato, or chickpeas right before they leave the oven. Additionally, finish dal tadka with a whisper of cayenne so the aroma stays lively. If you’re spice-sensitive, pair it with tomato or yogurt to soften the heat.
Keep it delicious. Cayenne loves citrus, garlic, and creamy textures. Consequently, olive oil + cayenne + lemon zest on grain bowls tastes intentional with almost no work.
Why it belongs here. A meta-analysis in the British Journal of Nutrition associated capsaicin with modest but significant reductions in body weight, BMI, and waist circumference in adults with overweight or obesity (Zhang et al., 2023). Moreover, mechanistic reviews describe capsaicin’s thermogenic pathways in detail (Zheng et al., 2017, Bioscience Reports).
Related MasalaMonk read: Cayenne Pepper for Weight Loss: Spicing Up Your Diet Plan! 🌶️ and then balance warmth and brightness with Cinnamon & Lemon for Belly Fat: Benefits, Evidence & Usage Tips.
Ginger: cozy, versatile, and quietly powerful for metabolism boosting spices
Ginger is the weekday friend that always shows up. Because it slips into tea, stir-fries, soups, chutneys, and smoothies, you can lean on it repeatedly without getting bored. Meanwhile, many people notice that ginger’s gentle heat calms “just a bite” impulses between meals.
Use it today. Grate ½–1 tsp fresh ginger into quick sautés; or simmer slices with water and lemon for a pre-lunch tea; or blend ¼ tsp ground ginger into a curd-and-berry smoothie; finally, stir a little into tomato curries or lentil soups right before serving.
Flavor pairings. Ginger brightens citrus; it mellows beautifully with honey; and, notably, it pairs seamlessly with soy-garlic-chili profiles. In Indian-style broths, ginger + black pepper + turmeric deliver warmth without heaviness.
What to expect. A synthesis in Nutrition Reviews pooling 27 randomized trials found ginger associated with reductions in body weight (~1.5 kg), BMI, waist circumference, and body-fat percentage compared with control (Rafieipour et al., 2024).
Keep going: build a comforting ritual with Turmeric, Ginger & Cinnamon Tea for Weight Loss and explore everyday uses in Ginger and Its Stunning Health Benefits.
Cinnamon (prefer Ceylon): breakfast’s best friend in metabolism boosting spices
Open a jar of cinnamon and the morning changes. Suddenly, oats, yogurt, and coffee feel like a plan rather than a scramble. In practice, cinnamon’s cozy sweetness helps many people steady the first half of the day; consequently, snacking tends to cool down.
Use it today. Stir ¼–½ tsp into oats or curd; additionally, dust it over coffee; or blend into a protein-and-fiber smoothie (banana + curd + ground flax); or simmer with stewed apples/pears and spoon over yogurt. In savory cooking, add a tiny pinch to tomato gravies or slow-cooked beans.
Smart notes. If you use cinnamon daily, prefer Ceylon (lower coumarin). Cassia, by contrast, works well in bolder dishes in smaller amounts.
What to expect. Controlled-trial syntheses report small but significant improvements in weight, BMI, and waist–hip ratio with cinnamon compared with control (Yazdanpanah et al., 2020, Clinical Obesity; Mousavi et al., 2020, Clinical Nutrition ESPEN).
Next steps: kitchen-level ideas live in Cinnamon for Weight Loss and Cinnamon Water to Reduce Belly Fat.
Turmeric + Black Pepper: the absorption duo of metabolism boosting spices
Turmeric has a reputation; yet, without pepper, much of it doesn’t land. Because piperine in black pepper dramatically improves curcumin absorption, this partnership is the rare “1 + 1 = 3” in seasoning.
Use it today. Stir ½ tsp turmeric into dals, soups, scrambled eggs, or golden milk; subsequently, finish with freshly cracked pepper and a little fat (ghee, olive oil, or coconut milk). Add pepper at the end so aromatics—and piperine—stay vivid.
Why the pairing matters. An umbrella review with updated analyses in the American Journal of Clinical Nutrition linked curcumin with reductions in BMI, weight, and waist circumference, with bioavailability-enhanced forms performing best (Unhapipatpong et al., 2023). Additionally, classic pharmacokinetic work showed 20 mg piperine increased curcumin bioavailability roughly twenty-fold in humans (Shoba et al., 1998, Planta Medica).
More ideas: practical pairing notes appear in Exploring the Science Behind Turmeric & Ginger for Effective Weight Loss.
Cumin (Jeera): a subtle cornerstone of metabolism boosting spices
Some flavors are so foundational that you miss them only when they’re absent. Cumin is that flavor. Freshly toasted and ground, it makes food taste “finished,” which—interestingly—often encourages smaller, more satisfying portions.
Use it today. Toast whole cumin seeds until fragrant; then cool, grind, and keep the jar beside your salt. Sprinkle ½ tsp on raita or chopped salads; fold into chickpea salads and lemony rice; or simmer jeera water in the morning and sip slowly.
Keep it bright. A squeeze of lime over cumin-forward dishes keeps them lively. Likewise, a handful of herbs (cilantro, mint) makes the same bowl feel new.
What to expect. In a three-month study within a reduced-calorie plan, 3 g/day cumin powder mixed into yogurt improved weight, BMI, waist, fat mass, and lipids versus control (Complementary Therapies in Clinical Practice: Zare et al., 2014). Related work in Annals of Nutrition & Metabolism reported benefits for weight-management markers in overweight adults (Taghizadeh et al., 2015).
Build a morning rhythm: sip ideas from Morning Metabolism Boost: 5 Green Tea & Spice Infusions.
Fenugreek (Methi): fullness first in metabolism boosting spices
Fenugreek is the quiet nudge toward “that’s enough.” Because its subtle bitterness gently raises satiety, it’s perfect for moments when second helpings usually appear out of nowhere.
Use it today. Soak a spoon of whole seeds overnight and chew before lunch; alternatively, whisk ½ tsp powdered methi into chapati flour; or temper a pinch in tadkas, sambars, and rustic tomato gravies. Additionally, a light fenugreek tea 20–30 minutes before your usual snack window can take the edge off.
Balance the taste. If bitterness feels new, add lemon or a touch of honey in drinks; in curries, rely on onion-tomato bases and a little fat to round it out.
What to expect. In a randomized, placebo-controlled, three-way crossover trial, fenugreek tea reduced short-term appetite ratings in overweight women versus control (Clinical Nutrition Research: Bae et al., 2015). Although the trial was brief, the satiety signal is practically useful.
Pair with brightness: a morning start using Lemon–Ginger–Turmeric Water complements methi beautifully. Also more about it in our post Fenugreek: An Appetite Suppressant for Weight Management.
Saffron: a graceful curb on grazing within metabolism boosting spices
Saffron doesn’t shout; it elevates. Because it turns simple sips into something special, it often softens the “I need a snack” itch without feeling punitive.
Use it today. Steep 3–4 strands in hot water; then add to milk with a hint of cardamom; or crumble into delicate broths; or fold into basmati rice with peas and toasted nuts. Notably, the luxury of saffron makes small portions feel complete.
What to expect. A double-blind trial linked a standardized saffron extract with less snacking and greater weight loss over eight weeks among mildly overweight women versus placebo (Nutrition Research: Gout et al., 2010). For broader context—and supplement-quality notes—see the overview by Mashmoul et al., 2013 (Journal of Nutrition & Food Sciences).
Also Read: Saffron: The Golden Spice for Weight Loss and Appetite Control
Ajwain (Carom): digestive support in the family of metabolism boosting spices
Ajwain is the friend you invite to keep things comfortable. Although it’s not a direct fat-loss driver in human trials yet, its digestive profile makes heavier meals feel lighter; therefore, it helps you stay consistent.
Use it today. Dry-roast and grind; add a tiny pinch to buttermilk, raita, or the jeera–ajwain–saunf mix below; sprinkle over roasted cauliflower with lemon and cilantro; or fold into paratha dough for a delicate, minty-herbal edge.
Evidence status. Weight-change trials in humans are limited. Nevertheless, a broad review describes thymol-rich seeds, digestive support, and antimicrobial notes (Boskabady et al., 2014, Iranian Journal of Basic Medical Sciences).
Also Read: Ajwain Benefits for Weight Loss: Unraveling the Secrets
Fennel (Saunf): a gentle evening finish among metabolism boosting spices
Fennel tastes like dessert’s cousin—sweetly herbal, soothing, and perfect for closing the kitchen. No wonder, many people find that a fennel ritual reduces night-time rummaging.
Use it today. Chew 1 tsp after dinner; or brew a light tea; or crush lightly and add to spice mixes; or bloom in oil for tomato-based sauces. Furthermore, fennel tea plus a slow 10-minute walk is a remarkably effective “day is done” signal.
What to expect. In the same crossover work that tested fenugreek tea, fennel tea lowered short-term hunger ratings in overweight women compared with control (Clinical Nutrition Research: Bae et al., 2015). Because the study was brief, consider fennel appetite support rather than a primary driver.
Also Read: Guide to Fennel Seeds and Weight Loss
Black Pepper (Piperine): the multiplier inside metabolism boosting spices
Freshly cracked pepper is habit-forming—in the best way. While it doesn’t appear to raise 24-hour energy expenditure on its own, it does multiply turmeric’s usefulness; therefore, it’s the “always add” move whenever curcumin is in the picture.
Use it today. Grind pepper over any turmeric dish—dal, soups, eggs, or golden milk—right at the end. Additionally, finish salads, eggs, and roasted veg with a quick crack to tie flavors together.
What to expect. Whole-room calorimetry found no change in 24-hour energy expenditure with black pepper alone (Functional Foods in Health & Disease: O’Connor et al., 2013). Conversely, piperine boosted curcumin bioavailability roughly twenty-fold in humans (Shoba et al., 1998, Planta Medica), which is why pepper belongs in every turmeric recipe.
Do Read: 8 Benefits of Black Pepper for Weight Loss
Two metabolism boosting spices blends you’ll actually use all week
Jeera–Ajwain–Saunf Powder (all-purpose, digestion-forward)
You’ll need: cumin (2 tbsp), ajwain (1 tbsp), fennel (1 tbsp)
Method: First, dry-roast each spice separately over medium heat until fragrant. Next, cool completely. Then grind to a fine powder and store airtight.
How to use: Stir ½ tsp into raita; sprinkle over cucumber–tomato salads; whisk ¼ tsp into warm water after meals 1–2×/day; add a pinch to paratha dough or khichdi.
Variations: Prefer a softer finish? Tilt the blend toward fennel. Want a minty nip? Nudge the ajwain slightly higher. If reflux flares, keep ajwain modest and pair with yogurt or buttermilk.
Turmeric–Ginger Tea (pepper-boosted)
You’ll need: water (250 ml), grated ginger (½ tsp or ¼ tsp powder), turmeric (½ tsp), a pinch of black pepper, optional cinnamon stick, lemon
Method: Simmer water with ginger and turmeric for 5 minutes. Then turn off heat, add pepper, steep 1 minute, strain, and finish with lemon.
How to use: One cup with breakfast or before a brisk walk works well. If evenings are your soft spot, let this be your “kitchen is closed” cue.
Why pepper matters: as noted earlier, piperine multiplies curcumin’s availability in humans, which is exactly why this pairing belongs in a plan built around metabolism boosting spices.
A 14-day, zero-overwhelm rotation (to make metabolism boosting spices stick)
Swap freely as life happens; nevertheless, this structure keeps momentum while steadily weaving metabolism boosting spices into everyday meals.
Day 1
Breakfast: Oats with curd, chia, and cinnamon; additionally, finish with a light crack of black pepper on top if you swirl in turmeric.
Lunch: Lemon-cumin cucumber salad alongside dal tempered with turmeric + pepper; moreover, add a squeeze of lime for lift.
Evening: Fennel tea; consequently, the gentle sweetness helps close the kitchen without cravings.
Day 2
Breakfast: Soft ginger scramble with a whisper of cayenne; alternatively, fold ginger into besan for a quick chilla.
Lunch: Chickpea salad dressed with toasted cumin, garlic, and lemon; furthermore, scatter herbs for freshness.
Dinner: Turmeric–ginger tea (pepper-boosted); meanwhile, keep portions calm with a small side of yogurt.
Day 3
Breakfast: Curd, banana, and cinnamon with ground flax; consequently, the combo rides steady till lunch.
Lunch: Tomato–ginger soup finished with ghee infused with turmeric + pepper; likewise, add a side of steamed veg.
Evening: Warm saffron milk with a hint of cardamom; afterward, lights low to signal “day is done.”
Day 4
Breakfast: Avocado toast with cayenne and cracked black pepper; additionally, a squeeze of lemon brightens the heat.
Lunch: Khichdi sprinkled with jeera–ajwain–saunf powder; meanwhile, a carrot salad adds crunch.
Dinner: Fennel tea and a slow 10-minute walk; consequently, late-night snacking fades.
Day 5
Breakfast: Smoothie (curd, berries, ginger, cinnamon); besides that, add chia for extra fiber.
Lunch: Grilled vegetables tossed with cumin and lemon; alternatively, serve over quinoa.
Evening: Turmeric–ginger tea (pepper-boosted); then, kitchen closed.
Day 6
Breakfast: Masala omelette (tomato, onion, ginger) finished with turmeric + pepper; likewise, a side of fruit.
Lunch: Lentil soup brightened with lime and toasted cumin; additionally, a cucumber salad cools things down.
Dinner: Light saffron broth; consequently, you end satisfied, not stuffed.
Day 7
Breakfast: Warm curd bowl with stewed apples and cinnamon; meanwhile, walnuts add crunch.
Lunch: Dal–rice with ghee infused with turmeric + pepper; furthermore, sprinkle fresh coriander.
Evening: Ginger–fennel tea; finally, an easy book instead of screens.
Day 8
Breakfast: Ginger-spiked besan chilla; subsequently, a spoon of mint raita.
Lunch: Raita seasoned with jeera–ajwain–saunf alongside a mixed-veg pulao; in the end, finish with lemon.
Dinner: Saffron tea; nonetheless, if hungry, add a few almonds.
Day 9
Breakfast: Overnight oats with cinnamon and orange zest; consequently, a bright, steady start.
Lunch: Tomato dal tempered with turmeric + pepper; likewise, a quick salad with toasted cumin.
Evening: Fennel tea; additionally, a short stretch helps digestion.
Day 10
Breakfast: Poha with grated ginger and a pinch of cayenne; alternatively, swap cayenne for extra lemon if sensitive.
Lunch: Quinoa salad with cumin–garlic–lemon dressing; moreover, toss in chickpeas.
Dinner: Turmeric–ginger tea (pepper-boosted); then, kitchen lights off.
Day 11
Breakfast: Curd with berries and cinnamon; meanwhile, pumpkin seeds add texture.
Lunch: Mixed beans with warm cumin vinaigrette; additionally, chopped onions and herbs for bite.
Evening: Saffron milk; consequently, dessert cravings soften.
Day 12
Breakfast: Savory masala oats with ginger; finally, a last-minute dusting of black pepper.
Lunch: Simple dal with a cucumber–onion salad dusted with jeera–ajwain–saunf; furthermore, add lemon.
Dinner: Fennel tea; alternatively, brew fenugreek tea if evenings are your snack window.
Day 13
Breakfast: Smoothie (curd, spinach, ginger, cinnamon); moreover, a teaspoon of flax keeps it satisfying.
Lunch: Roasted cauliflower with ajwain + cumin + lemon; likewise, a spoon of yogurt steadies spice.
Evening: Turmeric–ginger tea (pepper-boosted); consequently, appetite winds down naturally.
Day 14
Breakfast: Eggs with tomatoes and turmeric, finished at the table with black pepper; additionally, toast on the side.
Lunch: Chickpea curry rounded with cumin and coriander; meanwhile, a fresh salad for crunch.
Evening: Ginger–fennel tea to close the day; finally, a calm bedtime routine seals the habit.
How to keep it flexible: If a day runs long, simply swap the evening sip (fennel, saffron, or turmeric–ginger with pepper) for whichever you can make fastest; meanwhile, carry forward the skipped choice to tomorrow. Consequently, you maintain rhythm while continuing to layer metabolism boosting spices into meals you already cook.
Buying, storing, grinding: the unsexy wins behind metabolism boosting spices
First, buy whole (cumin, fennel, pepper) and grind weekly; aroma—and satisfaction—jump immediately. Second, toast before grinding: a minute in a dry pan releases oils and multiplies flavor; cool fully before grinding. Third, store smartly: dark jars, cool cupboards, tight lids; heat, light, and air steal flavor. Finally, finish smart: add pepper and delicate aromatics near the end so volatile compounds don’t vanish into steam.
Troubleshooting (and effortless swaps)
- Too hot? Swap cayenne for cinnamon or cumin; keep ginger mostly in tea rather than dry rubs.
- Too bitter? Temper fenugreek with lemon or a touch of honey; in curries, lean on onion-tomato bases and a little fat.
- Bored already? Rotate regions: dal one night, cumin-lemon salad the next, ginger-miso broth later in the week.
- No time? Keep toasted-ground cumin on the counter, fennel by the kettle, and a pepper mill next to the salt—one twist, one pinch, done.
- No progress yet? Revisit sleep, protein, and steps; metabolism boosting spices make good habits easier, but they don’t replace fundamentals.
Safety and comfort come first
Because your kitchen should make life easier, adjust spices to your context. If you’re pregnant or breastfeeding, on anticoagulants or glucose-lowering medication, or managing reflux or gallbladder issues, tailor doses and check with your clinician as needed. Generally speaking:
- With reflux, go lighter on cayenne and ginger; lean on cinnamon, fennel, and cumin.
- On blood thinners, be cautious with turmeric + pepper and avoid concentrated curcumin supplements unless advised.
- When adjusting glucose-lowering meds, introduce fenugreek carefully and watch for appetite or glycemic shifts.
- For any spice, start tiny (⅛ tsp), then step up slowly.
Keep exploring (reader-friendly companions)
- Cinnamon & Lemon for Belly Fat: Benefits, Evidence & Usage Tips
- Ginger and Its Stunning Health Benefits
- Turmeric, Ginger & Cinnamon Tea for Weight Loss
- Exploring the Science Behind Turmeric & Ginger for Effective Weight Loss
- Morning Metabolism Boost: 5 Green Tea & Spice Infusions
A closing nudge
None of these is a miracle on its own. Together—and, above all, repeatedly—they tilt your meals in the right direction. A little heat here, a calmer morning there, a cup that closes the kitchen at night: that’s how change actually looks. Pick two ideas that feel easy this week, make them yours, and keep going. The rest will follow.
FAQs
1) Do metabolism boosting spices actually work for fat loss?
Yes—just not like magic. Firstly, spices such as cayenne, ginger, cinnamon, turmeric (with black pepper), cumin, and saffron can nudge thermogenesis, tame appetite, and smooth post-meal energy. Secondly, these nudges are modest; however, they compound when you use them daily alongside balanced meals and movement. Consequently, think “steady assist,” not “instant fat burner.”
2) What spice boosts metabolism the most?
It depends on what you’ll use consistently. Cayenne (capsaicin) offers a gentle thermogenic lift; meanwhile, ginger and cinnamon help with appetite and post-meal comfort. Moreover, turmeric plus black pepper improves curcumin’s impact, while cumin and saffron support satiety and portions. In short, the “best” metabolism boosting spice is the one you’ll enjoy multiple times a week.
3) Which spices burn belly fat specifically?
No spice targets belly fat directly. Nevertheless, fat burning spices can help reduce overall body fat by supporting better adherence—fewer snack attacks, steadier energy, and more satisfying meals. Consequently, belly fat often decreases as part of overall loss when routines stay consistent.
4) What spices increase metabolism for beginners?
Start simple: cinnamon at breakfast, turmeric + black pepper at lunch, and ginger or fennel tea in the evening. Additionally, keep cumin nearby to finish salads and lentils. Importantly, begin with tiny amounts, then scale by taste; meanwhile, track how your appetite and energy respond.
5) Is there a single “spice that burns fat” fast?
Not really. However, a cayenne pinch can warm meals immediately; ginger can curb grazing; and saffron may lower snack urges. Moreover, cinnamon pairs well with protein and fiber for steadier mornings. Ultimately, sustainability beats speed—choose what you can repeat.
6) Do spicy foods boost metabolism more than mild ones?
Often, yes—capsaicin from chilies can increase thermogenesis a bit. Even so, intensely spicy food isn’t required. Instead, a modest sprinkle of cayenne or a mildly spiced curry can be enough. Furthermore, comfort matters: if heat bothers you, choose cinnamon, cumin, turmeric + pepper, ginger, fennel, or saffron for gentler support.
7) How should I use turmeric for weight loss?
Use turmeric with black pepper and a little fat. Firstly, stir ½ tsp turmeric into dal, soup, or eggs; secondly, finish with freshly cracked pepper; finally, include ghee/olive oil/coconut milk so curcumin absorbs better. Additionally, a small turmeric-ginger tea (pepper-boosted) works as an easy daily ritual.
8) Does turmeric speed up your metabolism on its own?
Turmeric helps more when paired with black pepper; otherwise, much of its curcumin isn’t absorbed well. Consequently, you’ll see better results from the duo. Meanwhile, if you’re sensitive to pepper, start with a very small pinch and build up gradually.
9) Is cinnamon good for losing weight?
Cinnamon pairs wonderfully with breakfast protein and fiber, which can reduce rebound hunger. Moreover, it makes oats, curd, and smoothies feel satisfying. Nevertheless, use modest doses and favor Ceylon cinnamon if you use it daily. In short, cinnamon supports the routine that supports the result.
10) What about cumin (jeera) for weight loss?
Cumin is the quiet over-achiever. Toast, grind, and sprinkle ½ tsp on raita, salads, chickpeas, or lentils. Additionally, jeera water in the morning can become a calming habit. While results are modest, the flavor makes portions feel complete; consequently, grazing often drops.
11) Can ginger help with metabolism and fat loss?
Ginger adds cozy warmth and, for many, reduces snack urges. For example, grate it into stir-fries or brew a quick tea 20–30 minutes before your “danger window.” Furthermore, pair ginger with a short walk; together, they often quiet that “just a bite” loop.
12) Are saffron and appetite suppressant spices useful?
Saffron can help some people snack less. A few strands in warm milk or tea feel luxurious; therefore, smaller portions still feel satisfying. Meanwhile, appetite-calming spices like fennel or fenugreek can also help you pause, reassess hunger, and stop earlier—especially at night.
13) Which spices boost metabolism without causing acidity?
Choose cinnamon, cumin, fennel, and saffron first. Additionally, turmeric + black pepper can work if you keep doses small and add fat. Conversely, go lightly with cayenne or strong ginger if you’re reflux-prone; nonetheless, tiny amounts folded into moist dishes are often tolerated.
14) What’s the simplest “weight loss spice mix” I can make at home?
Try a jeera–ajwain–saunf blend. To begin, dry-roast cumin (2 tbsp), ajwain (1 tbsp), and fennel (1 tbsp) separately, then grind and store airtight. Next, use ½ tsp in raita or ¼ tsp in warm water after meals. Moreover, adjust ajwain down if you prefer gentler digestion support.
15) Is black pepper itself a metabolism booster?
Alone, black pepper doesn’t seem to raise 24-hour energy expenditure meaningfully. However—and this is crucial—piperine enhances turmeric’s curcumin absorption, which makes the turmeric + pepper duo a practical everyday move. Consequently, keep a grinder beside your salt and finish dishes at the table.
16) Do “fat burning spices” help if my diet isn’t perfect?
They help most when the basics are steady. Even so, spices can reduce cravings, steady energy, and improve meal satisfaction, which, in turn, makes better choices easier. Additionally, they require almost no time: one pinch, one stir, done. Therefore, think of them as low-effort momentum.
17) How many times per day should I use metabolism boosting spices?
Twice is great; three times is excellent. For instance, cinnamon at breakfast, turmeric + pepper at lunch, and ginger or fennel in the evening. Moreover, keep cumin handy to finish salads or lentils. Importantly, small amounts used daily beat large doses used rarely.
18) Can I lose weight with spices but without exercise?
You can make progress with food habits alone; however, movement amplifies your effort. Meanwhile, even short walks—5 to 10 minutes after meals—improve how you feel and how your body handles food. Consequently, pair your spice routine with light activity whenever possible.
19) Are there side effects or people who should be cautious?
Yes, and it’s wise to personalize. For example, if you’re pregnant or breastfeeding, on blood thinners or glucose-lowering meds, or dealing with reflux/gallbladder issues, start small and check with your clinician. Additionally, listen to comfort: if something feels off, scale back and swap to gentler options.
20) What’s a realistic timeline to notice changes?
Give it 2–4 weeks of consistent seasoning to feel steadier energy and fewer snack impulses. Subsequently, look for small changes: slightly smaller portions, calmer afternoons, and easier evenings. Eventually, as meals feel “enough,” overall intake trends down—and results follow.
21) Which spices suppress appetite most naturally?
Different people respond to different cues. Nevertheless, saffron, fennel, and fenugreek stand out for many. Meanwhile, ginger helps when used before a walk or as a pre-meal tea. Additionally, cinnamon with protein/fiber at breakfast often reduces mid-morning grazing.
22) What’s the best bedtime spice routine for late-night cravings?
Go gentle and soothing. For instance, fennel tea after dinner is light and sweetly herbal; alternatively, saffron milk feels special without being heavy. Furthermore, a turmeric–ginger tea (pepper-boosted) can be calming if you tolerate it well. Consequently, late-night nibbling usually fades.
23) Which spices should I focus on for belly fat and metabolism if I only choose three?
Choose what fits your day:
- Cinnamon for breakfast stability and fewer sugar crashes.
- Turmeric + black pepper for a lunch or dinner anchor.
- Ginger (or fennel at night) for snack control.
Moreover, add a cumin sprinkle where you can—it’s an easy bonus.
24) What’s the easiest way to keep this going long-term?
Anchor habits to cues you already have. For example, crack pepper whenever you see turmeric; meanwhile, keep cinnamon by your coffee canister; additionally, place fennel near the kettle. Consequently, you’ll season on autopilot and stick with metabolism boosting spices without thinking.