Autoimmune diseases are complex, unpredictable, and often exhausting. While there’s no magic food that can “cure” conditions like rheumatoid arthritis, lupus, Hashimoto’s, or multiple sclerosis, mounting research shows that what you put on your plate can make a huge difference in how you feel day to day. If you’re seeking more energy, fewer flares, and a chance to regain control, start by adding these science-backed, anti-inflammatory foods to your daily routine.
Let’s break down the most powerful foods for taming inflammation—with real-life tips for making them a delicious, effortless part of your lifestyle.
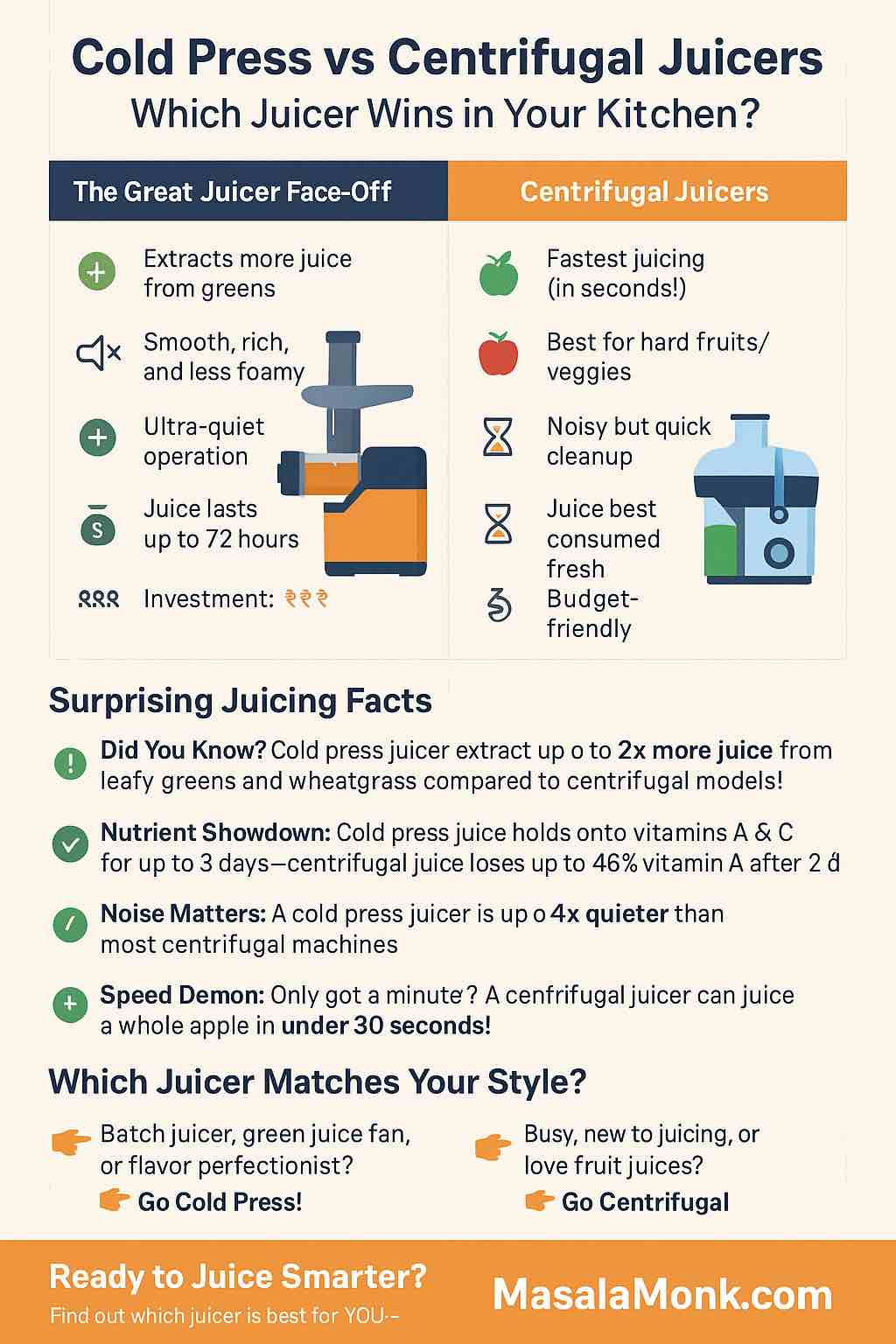
1. Fatty Fish (Salmon, Mackerel, Sardines)
Why they work: Fatty fish are rich in omega-3 fatty acids (EPA and DHA), which act like fire extinguishers for chronic inflammation. These fats not only lower inflammatory cytokines, but they also directly benefit joint pain and stiffness—especially in rheumatoid arthritis.
How to use them:
- Grill salmon fillets with lemon and herbs for a 20-minute dinner.
- Add tinned sardines or mackerel to salads or avocado toast for a protein boost.
Tip: If fish isn’t your thing, high-quality fish oil supplements are a proven alternative.
2. Extra Virgin Olive Oil
Why it works: The backbone of the Mediterranean diet, extra virgin olive oil contains polyphenols and oleocanthal, which have anti-inflammatory effects similar to ibuprofen, but without the side effects.
How to use it:
- Drizzle over roasted veggies or use as a salad base.
- Dip crusty whole-grain bread into olive oil, seasoned with fresh herbs and cracked pepper.
Tip: Use “cold-pressed” extra virgin olive oil for maximum benefits.
3. Leafy Greens (Spinach, Kale, Swiss Chard)
Why they work: These are nutritional powerhouses—rich in magnesium, vitamin C, and fiber. They help reduce oxidative stress, support detoxification, and provide essential nutrients that many autoimmune patients lack.
How to use them:
- Add spinach to morning smoothies (you won’t even taste it!).
- Sauté kale with garlic as a side dish for any meal.
- Try a big mixed green salad every day at lunch.
4. Berries (Blueberries, Strawberries, Raspberries, Blackberries)
Why they work: Berries are packed with anthocyanins and flavonoids—compounds shown to lower markers like CRP and help regulate immune responses.
How to use them:
- Sprinkle fresh or frozen berries on oatmeal, yogurt, or chia pudding.
- Blend into smoothies for a quick, nutrient-rich snack.
5. Fermented Foods (Yogurt, Kefir, Sauerkraut, Kimchi)
Why they work: Your gut is the command center for your immune system. Fermented foods provide probiotics that help restore gut balance and can “retrain” the immune system—especially helpful for conditions like IBD and Hashimoto’s.
How to use them:
- Add a spoonful of sauerkraut or kimchi to grain bowls or salads.
- Choose plain, unsweetened yogurt as a base for fruit parfaits or savory dips.
6. Turmeric (with Black Pepper!)
Why it works: Curcumin, the active compound in turmeric, powerfully reduces inflammation and is shown in trials to lower symptoms in RA, psoriasis, and even MS.
How to use it:
- Whisk turmeric and black pepper into soups, curries, or scrambled eggs.
- Try a “golden milk” latte (turmeric, ginger, black pepper, milk of choice) before bed.
Tip: Always pair turmeric with black pepper to boost absorption by up to 2000%.
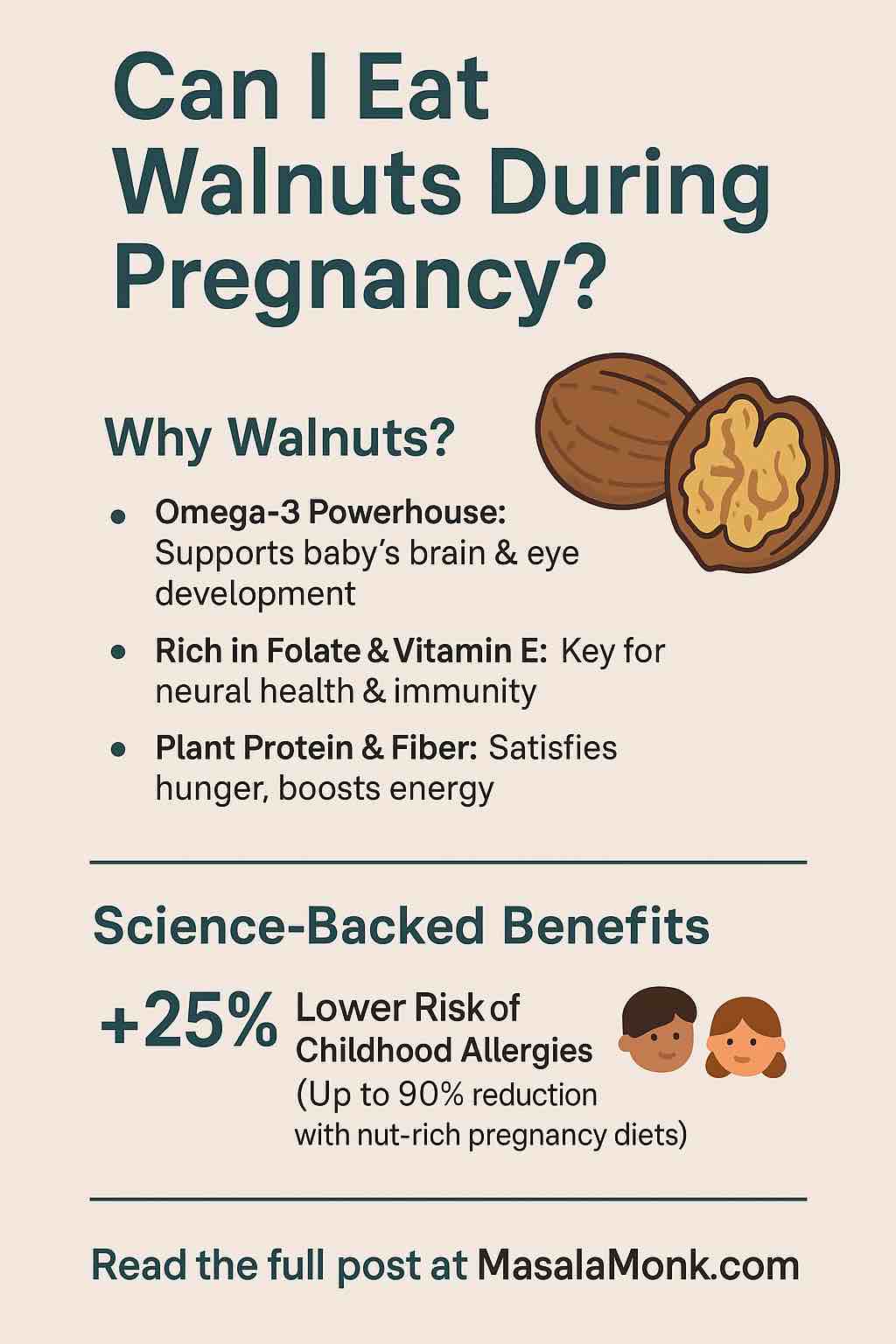
7. Nuts & Seeds (Walnuts, Almonds, Flax, Chia)
Why they work: Packed with healthy fats, fiber, magnesium, and zinc—nutrients that lower inflammation and support immune balance.
How to use them:
- Snack on a handful of mixed nuts every afternoon.
- Sprinkle chia or flax seeds into smoothies or over oatmeal.
- Make your own trail mix with nuts, seeds, and a few dried berries.
8. Cruciferous Vegetables (Broccoli, Brussels Sprouts, Cauliflower)
Why they work: These veggies are rich in sulforaphane and indoles—natural compounds that help regulate detoxification and balance immune responses.
How to use them:
- Roast broccoli or Brussels sprouts with olive oil and garlic for a crispy side.
- Add finely chopped cauliflower to stir-fries or grain bowls.
9. Ginger
Why it works: Like turmeric, ginger blocks inflammatory pathways and soothes gut inflammation. Research supports its use in reducing pain and joint stiffness.
How to use it:
- Steep fresh ginger slices in hot water for a calming tea.
- Add grated ginger to smoothies, stir-fries, or salad dressings.
10. Avocado
Why it works: Loaded with monounsaturated fats and antioxidants, avocado helps lower inflammation and supports healthy cholesterol levels.
How to use it:
- Smash on toast, top with seeds and a squeeze of lemon.
- Dice into salads or blend into creamy smoothies.
11. Whole Grains (Quinoa, Oats, Buckwheat, Brown Rice)
Why they work: Whole grains deliver fiber, magnesium, and phytonutrients that help feed good gut bacteria and modulate immune function.
How to use them:
- Cook a batch of steel-cut oats or quinoa for breakfast.
- Use buckwheat or brown rice as a base for grain bowls.
Practical Tips for Success
- Aim for Color & Variety: The more diverse your diet, the wider the range of anti-inflammatory nutrients you’ll get.
- Watch for Triggers: Not every “healthy” food works for every person with autoimmune disease—track your meals and symptoms to spot personal sensitivities (e.g., gluten, nightshades, dairy).
- Prioritize Whole Foods: Limit processed foods, added sugars, and excessive salt. They can all drive inflammation and flare-ups.
- Stay Consistent: Benefits are cumulative—focus on building sustainable habits, not quick fixes.
Sample Day: Anti-Inflammatory Eating
Breakfast: Overnight oats with chia seeds, blueberries, walnuts, and a drizzle of honey
Lunch: Kale salad with roasted salmon, avocado, quinoa, and sauerkraut
Snack: Greek yogurt with raspberries and pumpkin seeds
Dinner: Stir-fried broccoli and ginger over brown rice, topped with tofu or chicken
Drink: Turmeric-ginger “golden milk” latte
Frequently Asked Questions
What about supplements?
Food comes first! But omega-3, vitamin D, high-quality probiotics, and curcumin can help—ask your doctor about appropriate dosing.
How long until I notice a difference?
Many people feel improvement in energy, pain, or gut symptoms within weeks of consistent changes, but individual results vary.
Is there a “best” diet for autoimmune disease?
Most research supports Mediterranean-style or autoimmune protocol (AIP) diets, focusing on unprocessed, anti-inflammatory foods and eliminating common triggers.
Final Thoughts
If you’re battling an autoimmune disease, know that you have real tools at your disposal. Every anti-inflammatory meal you eat is a message to your body: “Let’s work together to heal.” Focus on progress, not perfection. And remember, small changes add up—start with a new berry smoothie, an extra spoonful of sauerkraut, or a golden milk latte, and see how you feel.
Your journey is unique. Listen to your body, stay curious, and never underestimate the power of food as medicine.
10 FAQs & Answers
1. What are the most common autoimmune diseases that benefit from an anti-inflammatory diet?
Most autoimmune diseases—including rheumatoid arthritis, lupus, Hashimoto’s thyroiditis, multiple sclerosis, inflammatory bowel disease (IBD), psoriasis, and type 1 diabetes—may benefit from anti-inflammatory dietary patterns. Scientific studies consistently show improvement in symptoms and lower inflammation markers across these conditions.
2. Can diet alone cure autoimmune disease?
No, diet cannot cure autoimmune disease. However, the right foods can reduce flare frequency, lessen symptom severity, and improve overall well-being. Diet is best used alongside medications and medical guidance.
3. How quickly will I notice improvements after changing my diet?
Some people notice increased energy, reduced pain, and better digestion within 2–4 weeks. For others, improvements may take longer. Consistency is key—results often build gradually.
4. Are there foods I should avoid with autoimmune disease?
Yes, common triggers include ultra-processed foods, added sugars, excessive alcohol, and trans fats. For some people, gluten, dairy, soy, or nightshades (tomato, eggplant, peppers) can worsen symptoms. It’s best to track your own triggers with a food diary.
5. Can I follow a vegetarian or vegan diet if I have an autoimmune disease?
Absolutely. Focus on plant-based sources of anti-inflammatory nutrients—legumes, nuts, seeds, leafy greens, berries, whole grains, and healthy oils. Consider supplementing with vitamin B12, vitamin D, and possibly omega-3s (from algae oil) to avoid deficiencies.
6. Should I take supplements like fish oil or curcumin?
Supplements can help if you’re not getting enough from food. Fish oil (for omega-3s), curcumin (turmeric extract), vitamin D, and probiotics have research support. Always consult your healthcare provider before starting new supplements, especially if you take medications.
7. How important is gut health for autoimmune conditions?
Extremely important! Over 70% of your immune system resides in the gut. Eating plenty of fiber, fermented foods, and a diverse range of fruits and vegetables supports healthy gut bacteria and immune balance.
8. Are all fermented foods helpful?
Most are, but look for “raw” or “live culture” products (e.g., unpasteurized sauerkraut, kimchi, kefir, yogurt with live cultures). Processed or pasteurized versions may not provide probiotic benefits.
9. How do I manage food sensitivities or allergies alongside autoimmune disease?
Elimination diets (like AIP or low FODMAP) can help identify food triggers. Work with a registered dietitian or healthcare provider to avoid nutritional gaps when restricting foods.
10. What’s a simple way to start eating anti-inflammatory?
Begin by adding one or two anti-inflammatory foods (like berries or leafy greens) to your daily routine. Replace processed snacks with nuts or seeds. Cook more meals at home using olive oil and a variety of colorful vegetables.