If you’re dialing in your nutrition yet still crave a twirl of noodles, lentil pasta for weight loss delivers comfort with staying power. It looks and eats like the pasta you love—penne, rotini, spaghetti, fusilli, and even sedanini—yet it’s typically higher in protein and fiber than regular wheat pasta. Consequently, it keeps you satisfied for longer while supporting a sensible calorie target. Because most varieties are naturally gluten-free and often made from a single ingredient (lentils), they fit seamlessly into balanced, high-protein meals that don’t feel like “diet food.” And if you want the broader science on why lentils help, you can skim our explainer on lentils for weight loss (science + recipes) before diving in.
What is lentil pasta—and why is it so weight-loss friendly?
Put simply, lentil pasta is milled lentils extruded into classic shapes. Red lentil pasta leads supermarket shelves, although green and yellow lentil versions exist as well. Many products are literally one ingredient—“red lentils”—which means you’re mostly getting protein and fiber with minimal extras. Others are a blend (often lentils + brown rice flour) to soften the bite for families or first-timers. Either way, the higher protein + fiber combo is the main reason lentil pasta for weight loss makes sense: it slows digestion, steadies energy, and helps you feel fuller with fewer calories.
Moreover, most brands stick to the familiar 56 g (2 oz) dry serving size. Therefore, if you already eyeball portions with wheat pasta, you can keep that habit and simply enjoy better macros per bite. If you’re also exploring gluten-free living, it helps to understand the basics of gluten itself; for a quick refresher, see our plain-English primer: what is gluten.
You’ll find plenty of shapes, so the swap feels easy: lentil spaghetti for lemon-garlic nights, red lentil penne for hearty ragùs, rotini for pasta salads, and even red lentil lasagna noodles from some specialty brands. Because texture can be the make-or-break factor for alternate pastas, we’ll also cover simple cooking tactics that keep things pleasantly firm.
Typical options you’ll see on shelves:
- Barilla Red Lentil Penne – one-ingredient, widely available in penne, rotini, and spaghetti.
- Trader Joe’s Organic Red Lentil Sedanini – short tubes that cling to sauce; easy weeknight pick.
- Explore Cuisine Red Lentil Penne – a blend (red lentil + brown rice) with a smooth, family-friendly texture.
- Tolerant Organic Red Lentil Penne – robust bite; also look for green lentil shapes for an earthier profile.
- Simply Nature Red Lentil Rotini (ALDI) – one-ingredient, budget/seasonal availability in many regions.
Why Lentil Pasta for Weight Loss Works (Protein, Fiber, and Glycemic Calm)
First, protein and fiber matter for satiety. Compared to standard refined pasta, lentil pasta usually delivers notably more of both per equal dry weight. As a result, you get more fullness for the calories and a steadier appetite curve between meals.
Second, post-meal blood sugar tends to be friendlier with pasta made from lentils than with refined wheat. While numbers vary by brand and blend, the legume base generally supports stable energy, which in turn reduces the urge to overeat later.
Third, portion control becomes simpler. Because you can keep the classic 2-ounce (56 g) dry serving, you’re not reinventing your plate—just upgrading its macro profile. Additionally, the familiar shapes make it easy to swap into your existing pasta recipes with minimal learning curve.
Put together, these factors explain why lentil pasta for weight loss is a practical, sustainable swap: you feel satisfied, you maintain structure, and you enjoy dinner. For readers building weekly structure, these high-protein pasta dishes are a helpful template; browse our roundup of plant-based high-protein pasta meal prep ideas and then plug in your preferred lentil shapes.
Red vs. Green vs. Yellow: Which Lentil Pasta Should You Choose?
Choosing the right color can improve your first experience; therefore, match flavor to the sauce you love.
Red Lentil Pasta for Weight Loss (Neutral, Crowd-Pleaser)
Why choose it: Red lentil pasta tastes mild—sometimes lightly sweet—so it works with almost any sauce. Consequently, it’s the best place to start if you’re new to lentil pasta for weight loss.
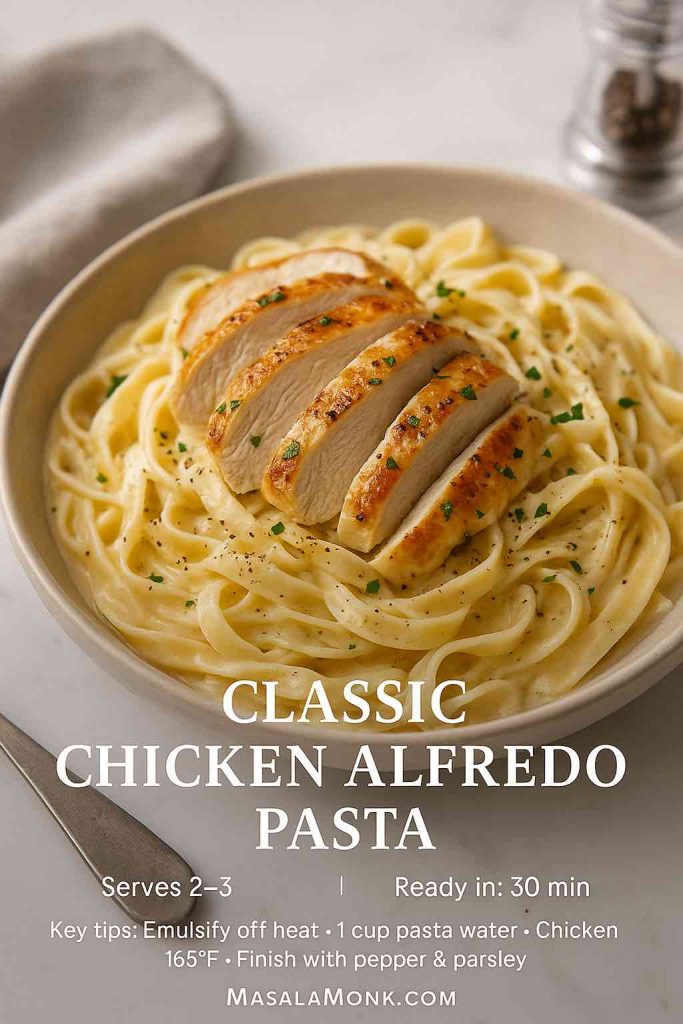
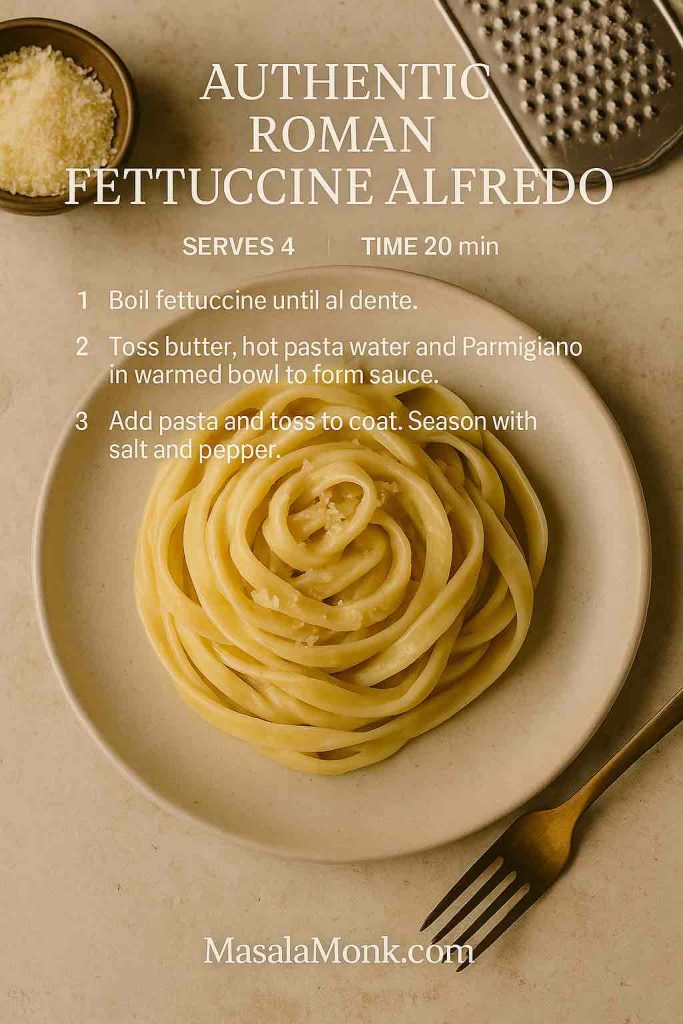
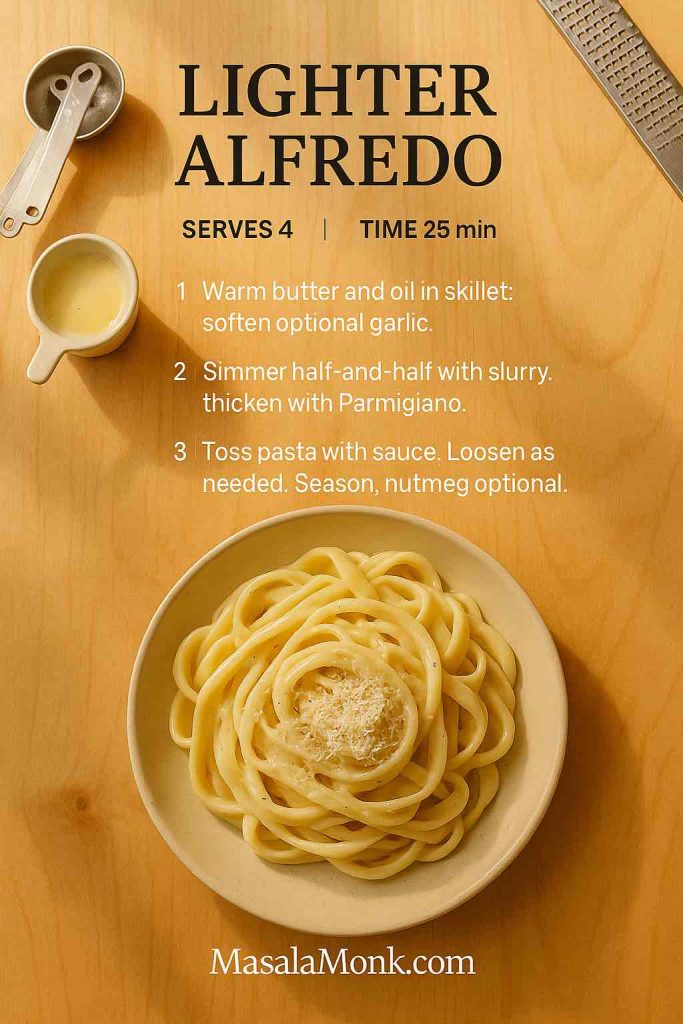
Great with: tomato-basil or arrabbiata, lemon-garlic, and even lighter “alfredo” riffs. If cream sauces are your love language, our technique-heavy guide to classic vs. authentic Alfredo shows how to achieve a silky emulsion with restraint (and how to adapt it to legume pasta).
Shapes to try: red lentil spaghetti, penne, rotini, fusilli, sedanini; you’ll even see red lentil lasagna noodles from some brands.
Bonus reading: If you want to double down on the base legume, see our deep dive on red lentils for weight loss.
Green Lentil Pasta (Earthier, Hearty Bite)
Why choose it: Green lentils bring a rustic flavor and a slightly firmer chew. In contrast to the mild red version, the earthiness pairs beautifully with herb-heavy sauces.
Great with: basil pesto, garlicky sautéed zucchini, roasted peppers, and olives. For more dish ideas that match this profile, scan the pesto and roasted-veg pairings inside our plant-based high-protein pasta ideas. Moreover, if you cook whole green or black lentils on the side, our piece on black lentils as a secret weapon for weight loss covers fiber-forward tricks that layer extra satiety into your plate.
Yellow Lentil Pasta (Mild, Occasionally Blended)
Why choose it: Yellow lentil pasta is less common; however, when you find it, expect a gentle, sweet edge. Some SKUs are blends—read the label if you need strictly one ingredient.
Great with: primavera, lemon-parsley, or simple olive-oil sauces where the pasta’s sweetness can shine. Meanwhile, if you’re looking to build a gluten-free pantry beyond pasta, our overview of millets—the gluten-free superfood will give you ideas for side dishes that complement these lighter sauces.
The Best Brands (Plain-English Comparison You Can Scan)
To keep things simple, here’s a “table-without-a-table” summary. Values below reflect typical expectations per 56 g (2 oz) dry; always check your box for exact macros.
Barilla Red Lentil — Penne, Rotini, Spaghetti
Taste & texture: Balanced, neutral, and consistent. Therefore, it’s a safe first purchase if you’re new to lentil pasta for weight loss.
Link: Barilla Red Lentil Penne
Try: Barilla’s red lentil penne in a weeknight tomato-basil bowl; if you prefer creamy, adapt the method from classic vs. authentic Alfredo to keep calories sensible.
Trader Joe’s Organic Red Lentil Sedanini
Taste & texture: Short tubes with plenty of sauce cling; budget-friendly if you shop at TJ’s.
Link: Trader Joe’s Organic Red Lentil Sedanini
Use it for: chunky vegetable ragùs or Mediterranean pasta salad. For even more Gluten Free pantry variety on busy weeks, rotate simple millet sides from millets—the gluten-free superfood.
Tolerant Organic Red or Green Lentil (Penne, etc.)
Taste & texture: Noticeably hearty; the green lentil line has an appealing, rustic edge. Some US labels use 3 oz (85 g) servings—convert when comparing.
Link: Tolerant Organic Red Lentil Penne
Cook’s note: The firmer bite holds up well in meal prep. For batch-cooking strategies, peek at our plant-based high-protein meal prep with lentils.
Explore Cuisine Red Lentil Penne
Taste & texture: The blend with brown rice flour softens the bite, which, in turn, helps legume-skeptics enjoy the switch.
Link: Explore Cuisine Red Lentil Penne
Best for: family dinners when you’re easing everyone onto pasta made from lentils; pair with the lighter Roman-style technique from classic vs. authentic Alfredo for a silky finish without a heavy cream load.
ALDI Simply Nature Red Lentil Rotini
Taste & texture: Solid everyday option when in stock; consequently, it’s great for meal prep on a budget.
Link: Simply Nature Red Lentil Rotini
Tip: When it appears seasonally, stock up for salad-friendly shapes. Then, round out lunches with a jarred soup or a homemade batch from our vegan lentil soup recipes for weight loss.
Pro tip: if a package lists nutrition per 100 g (3.5 oz), multiply those numbers by 0.56 to estimate a 56 g serving. Conversely, if it lists 85 g (3 oz), multiply by 0.66.
How to Cook Lentil Pasta Without Mush (Fool-Proof Method)
Cooking technique makes or breaks alt-pasta; however, these steps keep texture on point every time. Consequently, you’ll enjoy lentil pasta for weight loss without sacrificing bite.
- Salt the water generously. Pasta water should taste like the sea.
- Start tasting one minute early. Pull at firm al dente so the noodles finish in the pan with sauce.
- Stir gently. A little foam is normal with legumes; meanwhile, avoid aggressive boiling or over-stirring.
- Rinse only if advised or for cold salads. Otherwise, toss straight with sauce, and let carryover heat finish the cook.
- Portion wisely. Use 56 g (2 oz) dry as your everyday anchor; scale to 85 g (3 oz) for bigger appetites or training days.
- Match sauce to shape. Penne and rotini grab thick sauces; spaghetti loves slick emulsions like lemon-garlic or Roman-style Alfredo (see classic vs. authentic Alfredo).
5 Healthy Recipes Using Lentil Pasta for Weight Loss (Macros Included)
All five recipes assume 56 g (2 oz) dry red lentil pasta per serving. They’re high in protein and fiber, yet they remain easy and weeknight-friendly. Additionally, each one shows how to leverage flavor without overdoing calories.
1) Red Lentil Penne Bolognese (High-Protein, Ultra-Satisfying)
Why it supports weight goals: Lean ground turkey paired with high-protein pasta delivers a heavy hit of satiety. Consequently, one bowl keeps you full for hours.
Ingredients (1 serving)
- 56 g red lentil penne
- 120 g extra-lean turkey mince (or chicken mince)
- 120 g crushed tomatoes
- 40 g onion, finely chopped
- 1 tsp olive oil, garlic, oregano, salt, pepper
- Basil to finish (optional Parmesan)
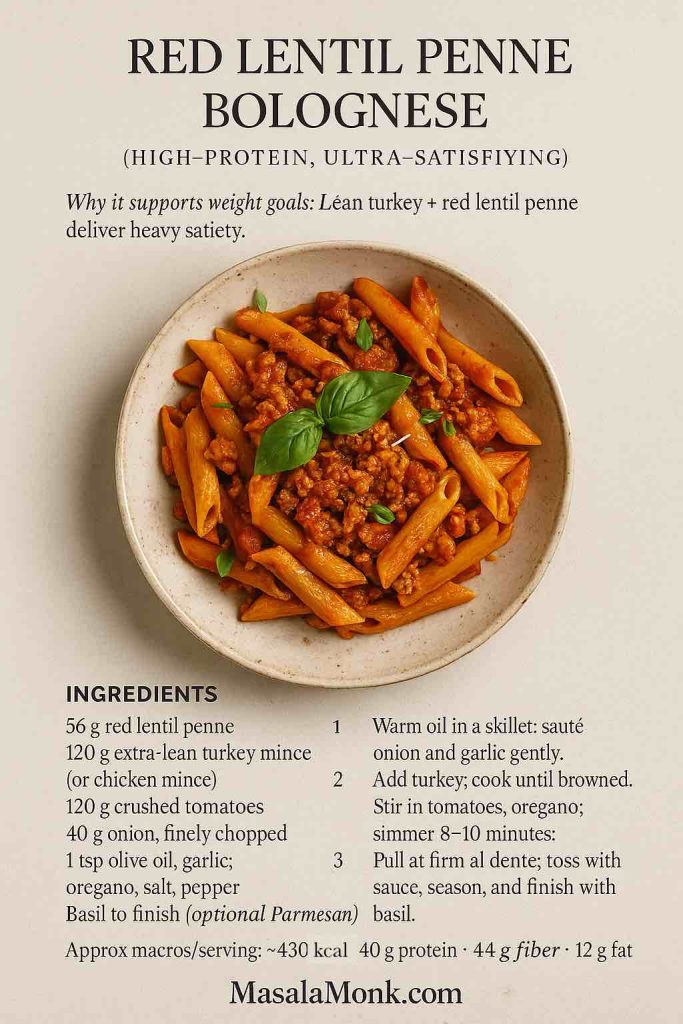
Method
Warm oil in a skillet and gently sauté onion and garlic until translucent. Add turkey; cook, breaking up the meat until browned. Stir in tomatoes and oregano; simmer 8–10 minutes. Meanwhile, cook the pasta to firm al dente. Toss with sauce, season, and finish with basil (and a spoon of Parmesan if desired).
Approx macros/serving: ~430 kcal • 40 g protein • 44 g carbs • 11 g fiber • 12 g fat
Also Read: Beyond Chicken: 5 Tempting Lentil Pasta Dinner Meal Prep Ideas, Plant-Powered and Protein-Rich
2) Lemon-Garlic Lentil Spaghetti (Light, Bright, and Fast)
Why it supports weight goals: The sauce is mostly lemon, garlic, and herbs—therefore, you get big flavor with minimal calories.
Ingredients (1 serving)
- 56 g red lentil spaghetti
- 1 tsp olive oil
- 1 garlic clove, thinly sliced
- Zest + juice of ½ lemon
- 1 tbsp chopped parsley
- 10 g grated Parmesan (or nutritional yeast for vegan)
- Chili flakes, salt
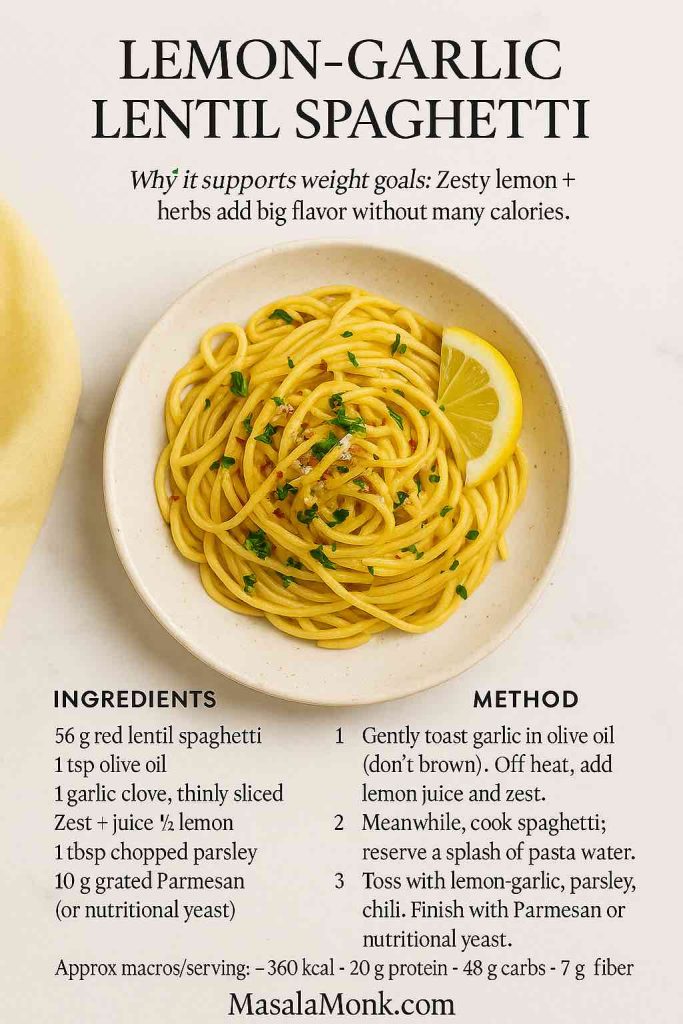
Method
Gently toast garlic in olive oil (don’t brown). Off heat, add lemon juice and zest. Meanwhile, cook spaghetti, reserving a splash of cooking water. Toss pasta with lemon-garlic, parsley, chili, and a spoon of cooking water to emulsify. Finally, finish with Parmesan or nutritional yeast.
Approx macros/serving: ~360 kcal (with Parmesan) • 20 g protein • 48 g carbs • 7 g fiber • 10 g fat
3) Mediterranean Lentil Pasta Salad (Meal-Prep Friendly)
Why it supports weight goals: Veggie volume adds fiber and water, which, in turn, boosts fullness without many calories.
Ingredients (1 serving)
- 56 g red lentil rotini
- 60 g cucumber, diced
- 60 g cherry tomatoes, halved
- 30 g red onion, thinly sliced
- 30 g olives, sliced
- 30 g feta or vegan feta
- 2 tsp extra-virgin olive oil
- 1 tsp red wine vinegar
- Dried oregano, black pepper
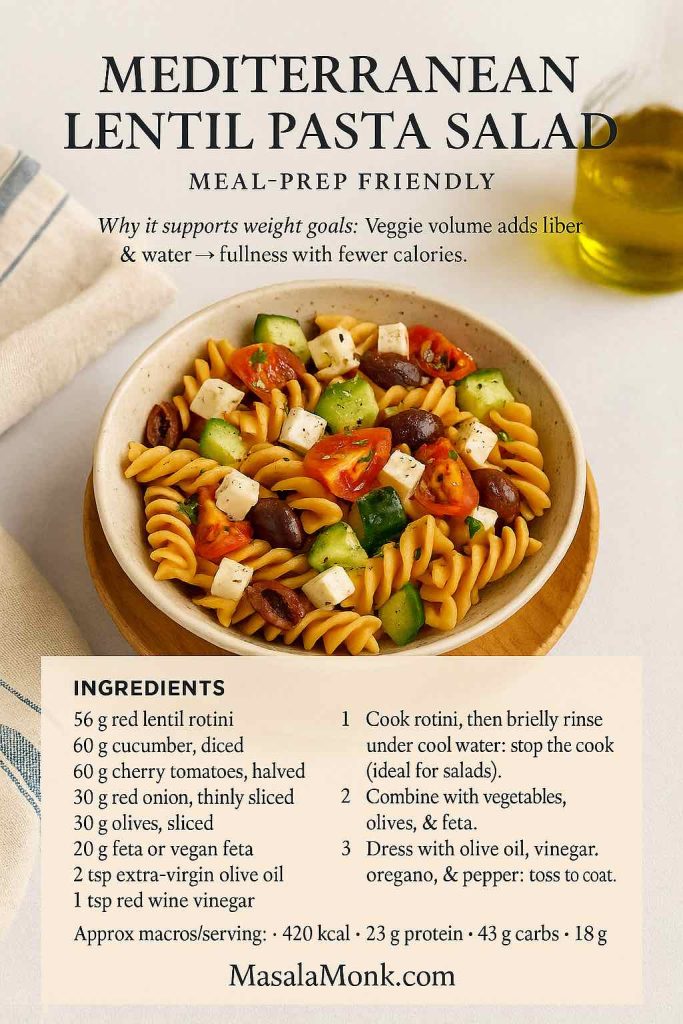
Method
Cook rotini, then briefly rinse under cool water to stop the cook (ideal for salads). Combine with vegetables, olives, and feta. Dress with olive oil, vinegar, oregano, and pepper; toss to coat. Because it holds up well, this salad is great for lunches over the next day or two.
Approx macros/serving: ~420 kcal • 23 g protein • 43 g carbs • 8 g fiber • 18 g fat
Also Read: 10 Most Popular Mediterranean Breakfasts
4) Creamy Vegan Red Lentil Alfredo (No Dairy, Still Silky)
Why it supports weight goals: Cauliflower + almond milk mimic creaminess without the heavy calories; consequently, you get comfort with control.
Ingredients (1 serving)
- 56 g red lentil penne
- 100 g cauliflower florets
- 120 ml unsweetened almond milk
- 1 tsp olive oil
- 1 tbsp nutritional yeast
- 1 tsp lemon juice
- Garlic powder, salt, pepper
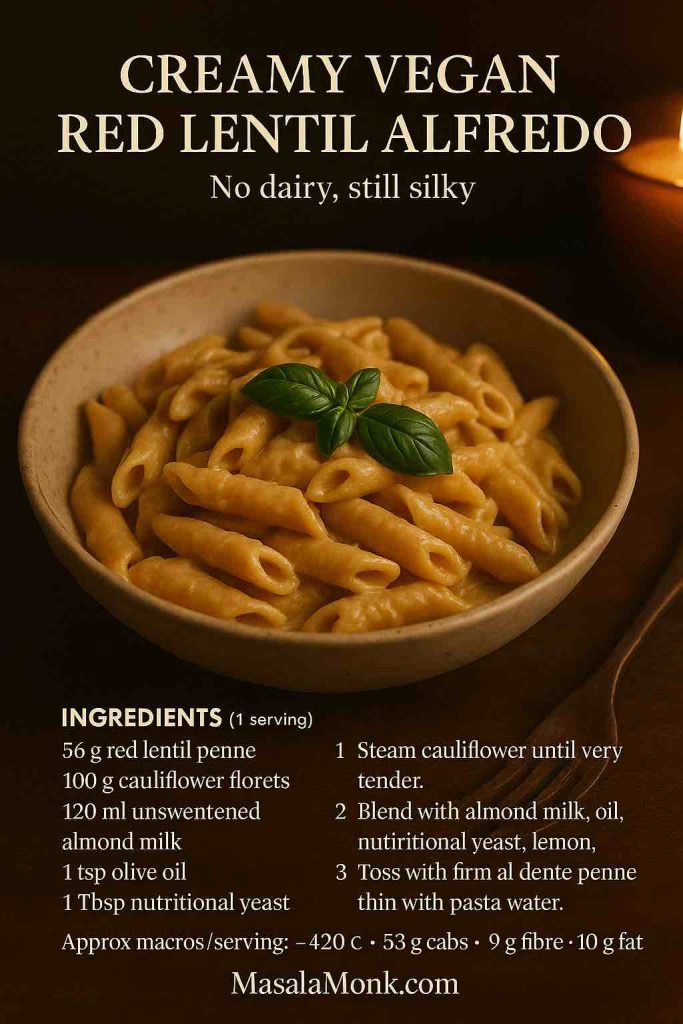
Method
Steam cauliflower until very tender. Blend with almond milk, olive oil, nutritional yeast, lemon, garlic powder, salt, and pepper until silky. Meanwhile, cook pasta to firm al dente. Toss with sauce, adjust seasoning, and add a splash of pasta water if you want it looser.
Approx macros/serving: ~380 kcal • 24 g protein • 53 g carbs • 9 g fiber • 10 g fat
5) Spicy Red Lentil Arrabbiata (Low-Oil, Big Flavor)
Why it supports weight goals: Heat from chili and acidity from tomatoes create intensity; therefore, you need less oil and cheese.
Ingredients (1 serving)
- 56 g red lentil spaghetti
- 200 g crushed tomatoes
- 1 tsp olive oil
- 1–2 tsp chili flakes
- 1 garlic clove, minced
- Parsley or basil, salt

Method
Sauté garlic briefly in olive oil. Add tomatoes, chili flakes, and salt; simmer 10 minutes. Meanwhile, cook spaghetti to firm al dente. Combine with sauce and finish with herbs. Because the flavors are bold, the dish feels indulgent while remaining lean.
Approx macros/serving: ~360 kcal • 22 g protein • 52 g carbs • 8 g fiber • 9 g fat
Also Read: Alfredo Pasta Reinvented: 5 Indian-Inspired Twists
Variations and Swaps to Keep Meals Interesting (and On-Plan)
Even with five core recipes, variety helps adherence; consequently, rotate these easy twists:
- Lentil and zucchini pasta: Spiralize or ribbon a small zucchini and toss it into the hot pan during the last minute for ultra-voluminous bowls.
- Italian lentils and pasta: Stir a small ladle of cooked brown lentils into tomato sauce for extra protein and a rustic feel.
- Chickpea and lentil pasta mix: Cook half chickpea pasta and half red lentil pasta for a blended bite and mixed amino profile.
- Lentil lasagna noodles: If you find them, layer with a light turkey ragù or spinach-tofu ricotta for a gluten-free bake.
- Lentil orzo: Use in soups, pilafs, or a quick “orzotto” with roasted vegetables and lemon.
Because these ideas keep textures and flavors changing, they make lentil pasta for weight loss easier to stick with long-term.
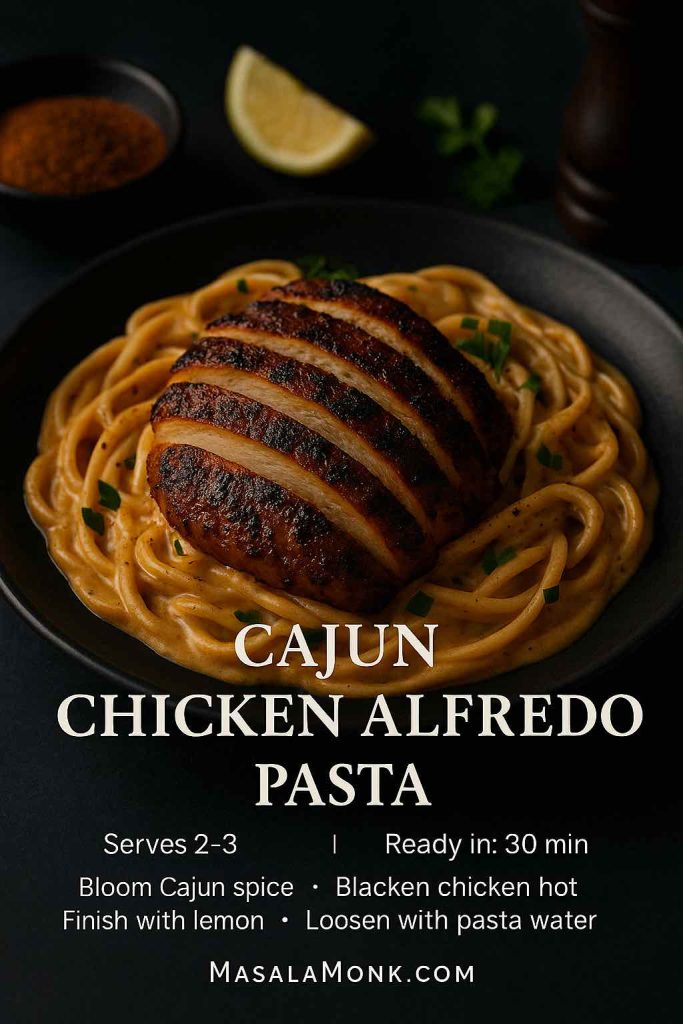
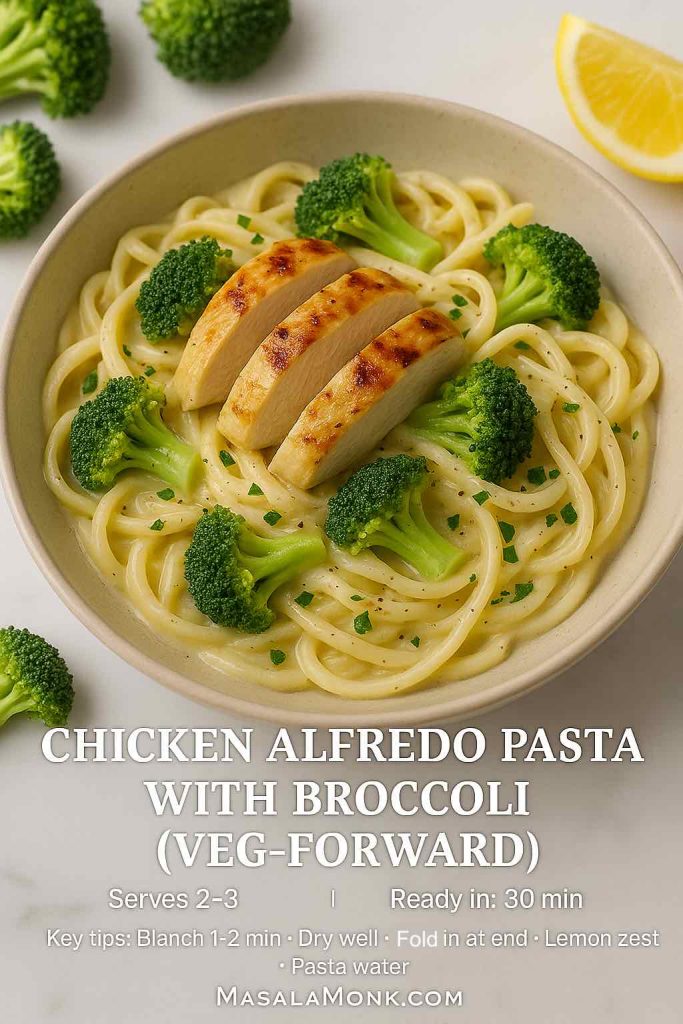
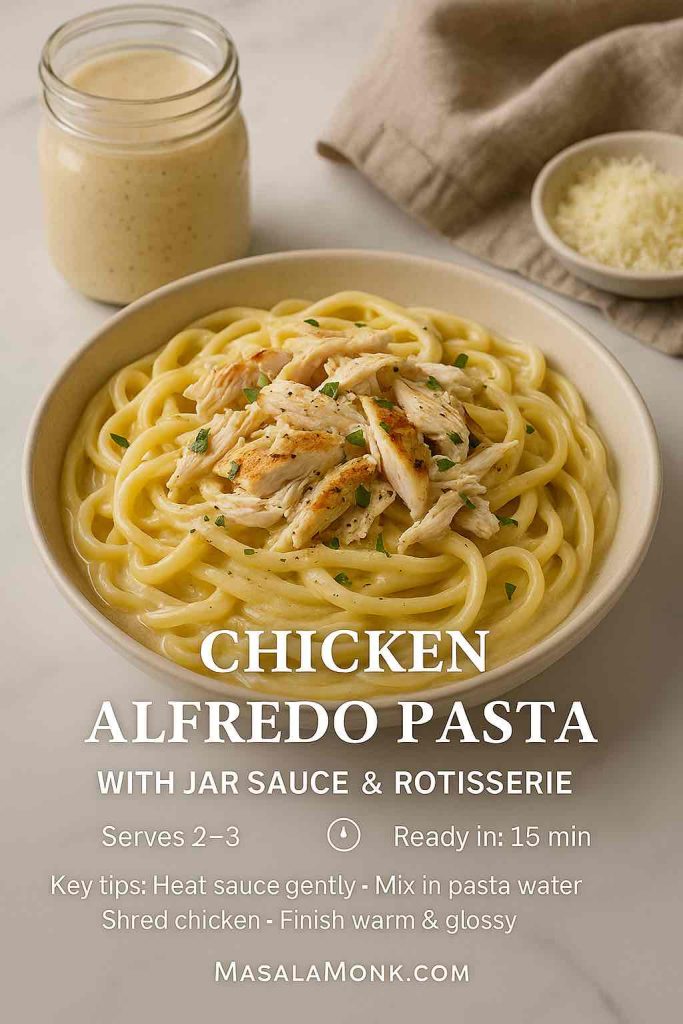
Also Read: Chicken Alfredo Pasta, 5 Ways (Classic to Cajun, Veg, 15-Minute Jar, Healthy)
Common Mistakes—and How to Fix Them Quickly
- Overcooking: Alt-pasta softens fast; therefore, taste early and pull at firm al dente.
- Oversaucing: Legume pasta grabs sauce aggressively. Start small, then add more if needed.
- Under-salting: Bland water equals bland pasta; salt generously.
- Skipping vegetables/protein: The win here is protein + fiber + volume. Add 2–3 cups of veg and a lean protein.
- Portion drift: A “handful” can creep to 100 g dry. Weigh a few times until your eyes calibrate. Consequently, your tracking stays honest.
Where to Buy Lentil Pasta (Popular Choices)
- Barilla Red Lentil Penne – plus rotini and spaghetti in many supermarkets.
- Trader Joe’s Organic Red Lentil Sedanini – US Trader Joe’s locations.
- Tolerant Organic Red Lentil Penne – retailer page with full nutrition.
- Explore Cuisine Red Lentil Penne – blended texture that’s family-friendly.
- Simply Nature Red Lentil Rotini – ALDI storefront listing; availability varies by region.
A practical 7-day rotation (to make it stick)
To turn lentil pasta for weight loss into a habit, plug it into an easy weekly rhythm. For example:
- Mon: Red lentil penne bolognese (double the sauce; freeze half).
- Tue: Lemon-garlic lentil spaghetti with roasted broccoli.
- Wed: Mediterranean lentil pasta salad + cup of vegan lentil soup.
- Thu: Creamy vegan red lentil Alfredo with peas; see classic vs. authentic Alfredo for emulsification cues.
- Fri: Spicy arrabbiata with herbs and a big side salad.
- Sat: Swap pasta for millet bowls (ideas from millets—the gluten-free superfood).
- Sun: Batch a pot of dal and skim our primer on lentils for weight loss for quick add-ins all week.
Because the template alternates pasta with soups and grains, you’ll avoid flavor fatigue, maintain fiber variety, and keep adherence high.
Final take: why this swap works in real life
Ultimately, lentil pasta for weight loss isn’t a fad; it’s a practical tweak that preserves pleasure while improving the macro profile of your favorite comfort meals. Choose an easy starter—Barilla for neutral flavor, Tolerant for a heartier bite, or Explore Cuisine for a blended texture—and cook it to firm al dente. Then, add a lean protein, pile on vegetables, and finish with a light, flavorful sauce. Because the texture feels familiar and the satiety is real, you’ll find it easier to stay on track night after night.
FAQs about Lentil Pasta for Weight Loss
1) Is lentil pasta good for weight loss?
Yes. Lentil pasta for weight loss works because it typically offers more protein and fiber than regular wheat pasta. Consequently, you feel fuller on fewer calories, which helps portion control and reduces snacking between meals.
2) Which is best for weight loss: red, green, or yellow lentil pasta?
All can fit, but red lentil pasta is the most neutral and therefore easiest to enjoy with lighter sauces. Meanwhile, green lentil pasta tastes earthier and often has a heartier bite, which some people find even more satisfying. Yellow is milder and occasionally blended; however, it still supports weight goals when portions stay reasonable.
3) Is lentil pasta gluten-free?
Generally, yes—if the ingredient list is just lentils. Nevertheless, always check the label, since some products blend in other flours. For weight management, the lentil pasta options with the simplest ingredient lists tend to be the most predictable.
4) How much protein is in lentil pasta?
Per 56 g (2 oz) dry, many lentil pasta products land around 12–16 g of protein, though brands vary. As a result, a standard plate can rival a small portion of meat or tofu in protein contribution—especially when you add lean protein on top.
5) What serving size should I use for weight loss?
Start with 56 g (2 oz) dry. For larger appetites or training days, you might go to 85 g (3 oz) dry; however, keep sauces lean and add vegetables so calories don’t creep up. Therefore, you maintain volume without overshooting your targets.
6) How do I cook lentil pasta so it doesn’t get mushy?
Salt the water well, then start tasting one minute early and drain at firm al dente. Next, toss directly with hot sauce to finish gently. If you’re making a cold salad, a quick rinse is fine; otherwise, avoid it so the sauce clings better.
7) Is lentil pasta lower carb or low glycemic?
Carbs are still present, but lentil pasta often has more fiber and a friendlier post-meal response than refined pasta. Consequently, many people report steadier energy. Even so, portion size still matters for blood sugar and weight outcomes.
8) Lentil spaghetti vs penne vs rotini—does the shape matter?
Functionally, yes. Lentil spaghetti suits slick sauces like lemon-garlic; penne and rotini grab chunkier sauces and veggies, which adds volume and satiety. Therefore, choose shapes that support the way you like to eat lighter.
9) Can I eat lentil pasta on low-carb or keto?
Strict keto, usually not. However, lentil pasta for weight loss can fit many moderate-carb or balanced plans because the protein and fiber improve fullness. If you’re carb-conscious, pair a modest portion with lean protein and lots of non-starchy vegetables.
10) What sauces pair well without blowing calories?
Tomato-based sauces, lemon-garlic emulsions, broth-y vegetable sautés, or light, dairy-free “alfredo” styles. Moreover, a teaspoon of olive oil plus herbs and chili can feel luxurious while staying calorie-aware.
11) Is organic lentil pasta better?
Nutritionally, organic vs non-organic lentil pasta is typically similar for protein and fiber. Therefore, base the choice on budget, availability, and taste rather than assuming a major macro difference.
12) Are brands like Barilla, Tolerant, Explore Cuisine, and Trader Joe’s very different?
They’re more similar than different, but serving sizes, texture, and minor nutrition details vary. For instance, some list a 3-oz (85 g) serving, which can look “higher” on the label. Consequently, convert to 2 oz (56 g) to compare apples to apples.
13) Can I meal-prep lentil pasta?
Absolutely. It holds up better than many alt-pastas. Nevertheless, undercook slightly, toss with sauce right away, and store in shallow containers. Reheat gently with a splash of water so it returns to al dente rather than turning soft.
14) Does lentil pasta work for athletes or gym-goers?
Yes. The combination of protein, fiber, and complex carbs supports training days. Meanwhile, on heavy workout days, you might increase the portion slightly and add an extra lean protein topping for recovery.
15) What if I’m on a tight budget?
You can still use lentil pasta for weight loss affordably. Look for store brands, seasonal deals, or bulk packs. Then, stretch sauces with canned tomatoes, frozen vegetables, and herbs—flavorful, filling, and cost-effective.
16) Can kids enjoy lentil pasta?
Definitely. Because shapes are familiar, most kids accept it readily—especially with simple tomato sauce. Gradually swap it in for family meals; consequently, everyone benefits from the extra protein and fiber without a big change in routine.
17) How often can I eat it?
As often as it helps you stay on plan. However, rotating with soups, whole grains, and other legumes keeps variety high and nutrition balanced. Therefore, try 2–3 lentil pasta meals per week and adjust based on preference and progress.
18) Any quick add-ins to boost protein even more?
Yes—stir in grilled chicken or turkey, shrimp, tofu, cottage cheese “cream,” or a few extra spoonfuls of cooked lentils. Consequently, the bowl becomes even more satisfying without needing heavy sauces.