Is there a natural supplement that could help you lose weight while also improving your overall health? Enter grape seed extract (GSE)—a powerful antioxidant that’s making waves in the world of wellness. But does it really work for weight loss? Let’s dig deep, separate fact from hype, and explore how you can make the most of grape seed extract in your own health journey.
What is Grape Seed Extract?
Grape seed extract is derived from the seeds of wine grapes (Vitis vinifera), typically the byproduct of winemaking. It’s loaded with potent antioxidants—most notably oligomeric proanthocyanidin complexes (OPCs)—along with vitamin E, flavonoids, and linoleic acid. These compounds are known for their anti-inflammatory, antioxidant, and potentially heart-healthy properties.
Why the Buzz Around Weight Loss?
The modern wellness world is hungry for safe, natural aids to make fat loss easier. Grape seed extract is especially popular because animal studies and some preliminary human research suggest it might:
- Support fat metabolism
- Reduce inflammation linked to obesity
- Improve blood sugar and cholesterol levels
- Potentially suppress appetite
But what does the science say—and is it really worth adding to your supplement stack? Let’s break it down.
Latest Research: Grape Seed Extract & Weight Management
1. What Human Studies Show (and Don’t Show)
Modest Effects on Weight—If Any
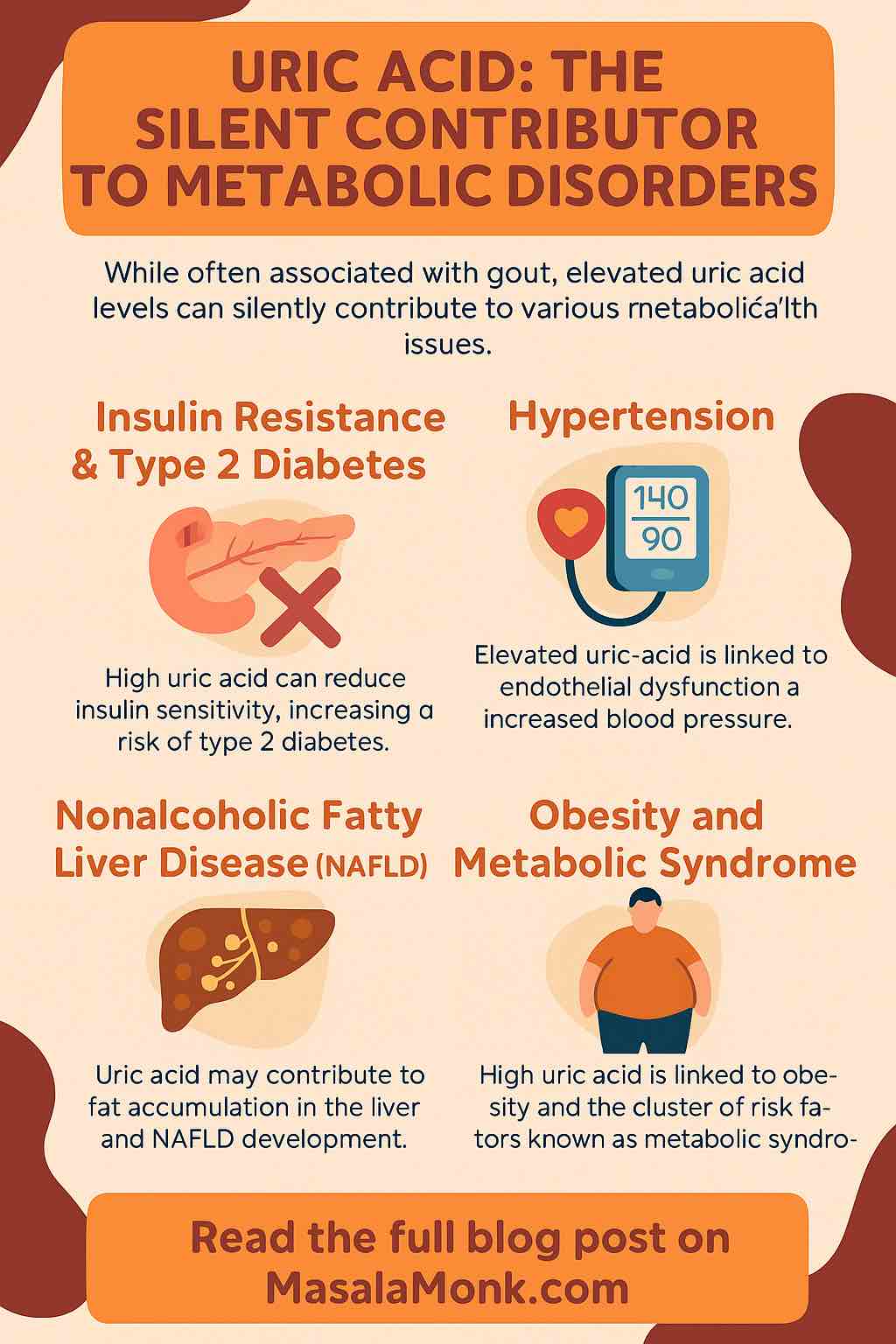
Large, high-quality clinical trials specifically measuring weight loss in healthy adults are still limited. Most studies focus on metabolic health or are conducted in people with conditions like Type 2 diabetes or nonalcoholic fatty liver disease (NAFLD).
- Short-Term Intake Reduces Calories: A standout, though older, study found that GSE supplementation reduced 24-hour calorie intake in healthy adults—especially those who normally eat a lot. Over longer periods and with calorie restriction, GSE helped reduce weight, BMI, and waist size more than diet alone. Still, results were modest and not universal.
- For Metabolic Health: Multiple new trials (2023–2024) show GSE improves insulin sensitivity, blood pressure, cholesterol, and liver fat in people with metabolic diseases—even when actual weight doesn’t change much.
- In Type 2 Diabetes & NAFLD: Doses of 500–520mg/day for 4–8 weeks led to better fasting glucose, lower insulin resistance, improved cholesterol profiles, and healthier livers. Body weight itself, however, typically stayed the same.
Takeaway:
GSE can support a healthier metabolism and might help reduce calorie intake—especially if paired with a balanced diet. On its own, it’s not a magic bullet for weight loss.
2. Animal & Laboratory Studies
Animal and cell studies paint a rosier picture:
- GSE reduces fat accumulation and inflammation in rats fed high-fat diets.
- It seems to inhibit fat cell formation, boost fat breakdown, and block enzymes that absorb dietary fat.
- It also appears to protect the liver, regulate blood sugar, and lower blood pressure.
But…
The effects in humans are far milder. It’s a classic case of “promising in rats, less impressive in people.”
How Does Grape Seed Extract Actually Work?
The Science in Simple Terms
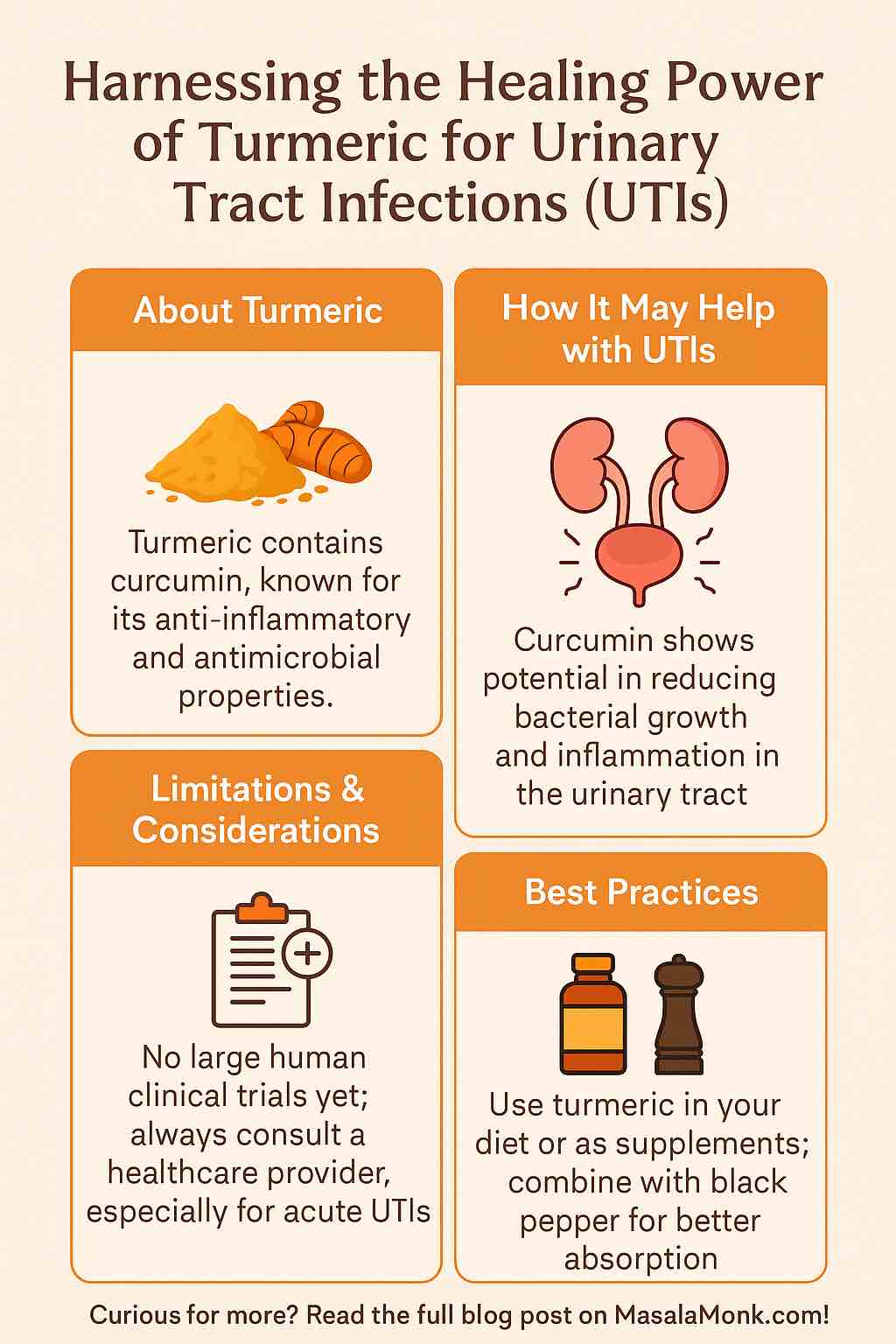
- Antioxidant Action: GSE’s polyphenols fight oxidative stress and inflammation—two processes that sabotage metabolism and can make weight loss harder.
- Fat Absorption Blockade: Some lab research shows GSE inhibits enzymes (like pancreatic lipase) that help the body absorb fat. Less absorbed fat = fewer calories stored.
- Appetite and Calorie Control: Early evidence suggests GSE may reduce appetite or blunt post-meal sugar spikes, helping some people eat less.
- Improved Insulin Sensitivity: By making your body’s insulin work better, GSE may help you burn fat more efficiently and prevent fat gain.
Practical Guide: How to Use Grape Seed Extract Safely
1. What to Look For
- Choose standardized extracts, ideally with 95% proanthocyanidins.
- Reputable brands provide third-party testing for purity and potency.
2. Typical Dosage
- Human studies use 100–600mg/day (most often 300–520mg).
- Higher doses don’t necessarily mean better results.
3. When to Take It
- GSE can be taken with meals.
- For metabolic support, consistency is key—take daily for at least 4–8 weeks.
4. Safety & Side Effects
- Generally very safe.
- Rare side effects: headache, nausea, mild GI upset.
- Caution: If you’re on blood thinners or have a bleeding disorder, talk to your doctor first—GSE may slightly thin the blood.
Realistic Expectations: What GSE Can (and Can’t) Do
What GSE CAN Do:
- Modestly improve cholesterol, blood sugar, and blood pressure.
- Help reduce liver fat (in NAFLD).
- Reduce inflammation and oxidative stress.
- Possibly help some people eat less or absorb less fat.
What GSE CAN’T Do:
- Melt away fat without lifestyle change.
- Substitute for a healthy diet or exercise.
Think of grape seed extract as a supportive team player, not the star of the show.
Tips for Maximizing Your Results
- Pair GSE with a calorie-controlled, nutrient-dense diet.
- Stay physically active—GSE may help your body burn fat, but you still need to move.
- Consider other polyphenol-rich foods: blueberries, cranberries, dark chocolate, green tea.
- Track your progress—measure waist, weight, blood markers over time.
The Bottom Line
Grape seed extract is a safe, well-studied supplement with proven benefits for metabolic health. While it won’t melt pounds away overnight, it can support your efforts—especially if you’re dealing with metabolic syndrome, insulin resistance, or fatty liver. As part of a holistic approach (diet, exercise, good sleep), it’s a smart addition for those looking to optimize health.
References (For Further Reading)
- Meta-Analysis, 2021: GSE for Metabolic Syndrome
- Latest RCT in NAFLD Patients
- Examine.com: Grape Seed Extract Overview
- Nutrients (2023): Polyphenols and Obesity
Ready to try grape seed extract? Remember: supplements work best when you work with them! Take control of your health, stay consistent, and watch the results unfold—one smart step at a time.
Have you tried GSE? Share your experience or questions below!
Frequently Asked Questions (FAQs)
1. Can grape seed extract really help with weight loss?
Answer:
Grape seed extract can support metabolic health and may help reduce calorie intake or fat absorption in some people, but clinical evidence for significant weight loss is limited. It works best as part of a healthy lifestyle, not as a standalone fat burner.
2. How much grape seed extract should I take for weight management?
Answer:
Most studies use between 100 and 600 mg per day, often standardized to 95% proanthocyanidins. For metabolic benefits, 300–520 mg daily for at least 4–8 weeks is typical. Always follow the manufacturer’s recommendations and consult your healthcare provider.
3. Are there any side effects of grape seed extract?
Answer:
Grape seed extract is generally well-tolerated. Some people may experience mild side effects like headache, nausea, or stomach discomfort. Rarely, it can increase bleeding risk, especially if combined with blood thinners.
4. How long does it take to see results from grape seed extract?
Answer:
Most metabolic improvements (such as better cholesterol or blood sugar) are seen after 4–8 weeks of consistent use. Weight changes, if any, are usually modest and take time, especially when paired with a healthy diet and exercise.
5. Can I take grape seed extract with other supplements or medications?
Answer:
GSE can be combined with most supplements, but use caution if you take blood thinners or drugs that affect liver enzymes. Always check with your doctor or pharmacist before starting a new supplement.
6. Will grape seed extract interact with my medication?
Answer:
GSE has mild blood-thinning effects and may interact with anticoagulants (like warfarin), antiplatelet drugs, or NSAIDs. If you’re on any of these, talk to your healthcare provider before using GSE.
7. Is grape seed extract safe for everyone?
Answer:
GSE is safe for most adults when used as directed. It’s not recommended for children, pregnant or breastfeeding women, or those with allergies to grapes without medical supervision.
8. What’s the best time of day to take grape seed extract?
Answer:
There’s no strict timing. It can be taken with meals to support absorption and reduce potential stomach upset. Consistency matters more than timing.
9. Should I use grape seed extract if I have diabetes or fatty liver?
Answer:
Clinical studies show benefits for blood sugar control and liver health, especially in people with Type 2 diabetes or NAFLD. If you have these conditions, discuss GSE with your doctor to ensure it fits your care plan.
10. Does grape seed extract have any benefits besides weight loss?
Answer:
Yes! GSE is rich in antioxidants and supports heart health, lowers blood pressure, improves cholesterol, and reduces inflammation. These benefits make it useful for overall wellness, not just weight management.