Breathing is one of the most natural acts we perform, yet we rarely stop to consider the health of our lungs—until something goes wrong. With pollution, allergies, viral infections, and the daily stresses of modern life, keeping our respiratory system strong has never been more important. While medical science provides many solutions, nature offers its own pharmacy, filled with herbs that have soothed lungs and eased breathing for generations.
But do these time-tested remedies stand up to modern science? And what are real people saying about their effectiveness? Let’s explore the research, the stories, and the practical ways you can harness these five powerful herbs to support your lung health today.
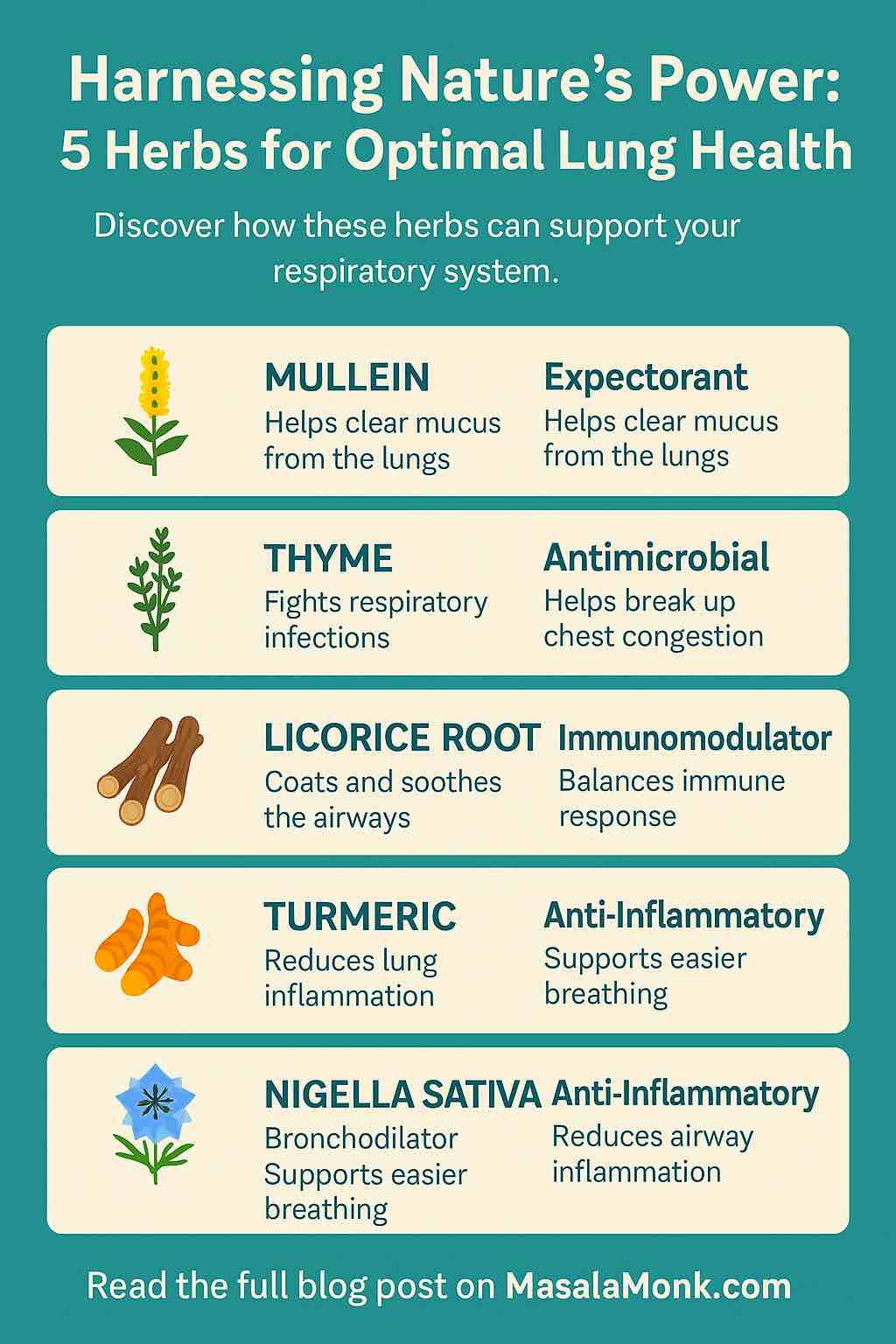
1. Mullein: The Gentle Lung Guardian
What Is It?
Mullein (Verbascum thapsus) is a tall, fuzzy-leaved plant long revered in folk medicine for its gentle, supportive action on the respiratory tract.
How Does It Work?
- Expectorant: Helps clear excess mucus from the lungs, making coughs more productive.
- Demulcent: Soothes irritated lung tissue with its mucilage content.
- Mild anti-inflammatory: Reduces irritation and swelling.
The Science
Recent reviews confirm mullein’s anti-inflammatory and antimicrobial properties, with studies showing it can help ease coughs and clear bronchial congestion【web†source】.
Real User Experiences
On Reddit and herbal forums, people share stories of gradual but noticeable improvement:
“Mullein tea was the only thing that helped my lungs after a nasty pneumonia. After weeks of struggling, I finally started clearing out mucus and breathing easier.”
“It took a couple of months, but mullein made a real difference in my lung strength and stamina.”
How to Use
- Tea: Steep 1–2 tsp dried mullein leaves/flowers in hot water for 10–15 minutes. Strain carefully—mullein hairs can irritate the throat.
- Tincture or syrup: Available in health stores for those seeking concentrated forms.
- Steam inhalation: Add mullein leaves to boiling water, inhale the soothing vapors.
Tip: Combine with marshmallow root or licorice for extra soothing power.
2. Thyme: The Respiratory Reviver
What Is It?
Thyme (Thymus vulgaris) isn’t just a kitchen staple—it’s a potent herbal ally for fighting coughs, congestion, and chest infections.
How Does It Work?
- Antimicrobial: Thymol and carvacrol combat bacteria and viruses.
- Expectorant: Helps break up and clear stubborn mucus.
- Anti-inflammatory: Soothes inflamed airways.
The Science
Recent clinical trials show thyme syrup significantly improves coughs and FEV₁ (a key lung function metric) in children and adults with mild to moderate asthma. Thyme-ivy extracts are also proven to reduce bronchitis symptoms【web†source】.
Real User Experiences
“Whenever I have stubborn phlegm, thyme tea is my go-to. It cuts through the gunk better than anything else.”
“A blend of mullein, sage, thyme, and licorice root has made my winter coughs a thing of the past.”
How to Use
- Tea: Steep 1 tsp dried thyme in hot water for 10 minutes. Add honey and lemon.
- Steam: Add a handful of thyme to hot water, inhale the vapor.
- Syrup: Look for thyme-ivy formulas at pharmacies for standardized doses.
Practical Blend: Try mixing thyme with mullein and licorice for an all-around lung tonic.
3. Licorice Root: The Soothing Shield
What Is It?
Licorice root (Glycyrrhiza glabra) has a long history in Chinese and Western herbal medicine as a lung soother and immune booster.
How Does It Work?
- Demulcent: Coats and soothes the airways.
- Expectorant: Makes coughs more productive.
- Immunomodulator: Helps balance the body’s immune response.
The Science
A 2024 review found that licorice extract capsules (containing glycyrrhizin) significantly improved lung function and reduced airway inflammation in asthmatic patients. Animal studies show licorice is nearly as effective as prescription steroids in reducing inflammation.
Real User Experiences
“Licorice tea is part of my daily blend during allergy season. My throat feels less scratchy and my cough calms down.”
“Caution: Licorice is awesome, but don’t overdo it—my blood pressure shot up when I drank it every day for a month.”
How to Use
- Tea: Use a small piece of dried root or a teaspoon of chopped root. Steep for 10–15 minutes.
- Blend: Works well with mullein, thyme, and marshmallow root.
- Capsules/extracts: Always check the dosage, and consult with your doctor if you have high blood pressure or heart issues.
Safety Note: Avoid long-term or high-dose use unless advised by a healthcare provider. Licorice can raise blood pressure and affect potassium levels.
4. Turmeric: The Golden Protector
What Is It?
Turmeric (Curcuma longa) is a bright yellow root, famous for its anti-inflammatory effects, used for centuries in Ayurveda.
How Does It Work?
- Anti-inflammatory: Curcumin, turmeric’s key compound, reduces cytokine-driven lung inflammation.
- Antioxidant: Protects lung tissue from damage.
- Immunity modulator: May help the body resist infection and recover from injury.
The Science
Modern studies and reviews show that turmeric and curcumin can reduce lung inflammation and tissue damage in conditions like fibrosis and chronic bronchitis. High-bioavailability forms of curcumin are most effective.
Real User Experiences
“After adding turmeric capsules to my daily routine, my lungs feel less tight, and I haven’t had a winter chest infection in two years.”
“I use turmeric and ginger together for a spicy tea that helps with both inflammation and phlegm.”
How to Use
- Golden Milk: Simmer 1/2 tsp turmeric powder with milk, add black pepper and honey.
- Capsules: Opt for standardized curcumin with black pepper extract for best absorption.
- Tea: Combine with ginger for a warming, anti-inflammatory blend.
Tip: Always pair turmeric with a pinch of black pepper—it increases curcumin absorption up to 20 times!
5. Nigella Sativa (Black Seed): The Ancient Remedy
What Is It?
Nigella sativa, or black seed, has been called the “seed of blessing” and used for millennia in Middle Eastern and South Asian medicine.
How Does It Work?
- Bronchodilator: Relaxes airway muscles for easier breathing.
- Anti-inflammatory and antioxidant: Protects against tissue damage and overactive immune response.
- Mucolytic: Helps clear out mucus and relieve congestion.
The Science
Clinical trials in asthma patients show that black seed extract (50–100 mg/kg daily) improves lung function (FEV₁), reduces nighttime wheezing, and can be as effective as conventional bronchodilators over 6–8 weeks【web†source】.
Real User Experiences
“Black seed oil took the edge off my asthma attacks. I take a spoonful every morning during allergy season.”
“Started using black seed capsules and felt my wheezing cut in half within a month.”
How to Use
- Oil: 1 tsp daily, either straight or mixed into smoothies/yogurt.
- Capsules: Follow product guidelines; most studies use 500–1,000 mg daily.
- Whole seeds: Sprinkle on food or add to bread, but oil or capsules are more concentrated.
Note: Start low and increase gradually; discuss with your healthcare provider if you’re on medications.
How to Create Your Own “Lung Health” Herbal Routine
1. Start Simple
Choose one or two herbs based on your needs. For stubborn mucus, thyme and mullein; for inflammation, turmeric and licorice; for asthma-like symptoms, black seed.
2. Use Consistently
Most users and clinical studies report best effects with daily use over several weeks. Herbal teas can be sipped 2–3 times daily; capsules should follow label or practitioner advice.
3. Combine Wisely
Herbs can be blended for synergistic effects. A classic tea blend:
- 1 tsp mullein
- 1/2 tsp thyme
- 1/2 tsp licorice root
- 1/2 tsp marshmallow root
Steep in hot water, strain, and sip slowly.
4. Monitor and Adjust
Keep a journal of symptoms, energy levels, and lung function (if using a peak flow meter). Adjust your routine and consult your doctor if you have chronic health issues or are on medication.
5. Stay Safe
- Check for allergies before trying new herbs.
- Use high-quality, reputable products.
- Consult your healthcare provider if you’re pregnant, nursing, have heart/kidney issues, or take prescription medications.
Final Thoughts
Our lungs are our life force. By embracing nature’s time-honored remedies—backed by both science and lived experience—you can give your respiratory system the gentle support it deserves. Whether you’re recovering from illness, facing allergies, or just seeking to breathe easier, herbs like mullein, thyme, licorice root, turmeric, and black seed can play a practical role in your wellness toolkit.
Remember: herbal medicine works best when it’s personal, consistent, and respectful of your body’s needs. Listen to your breath, nurture your lungs, and let nature help you breathe easier—one cup of tea at a time.
Further Reading & Resources
- Reddit: r/herbalism
- Herbal Research at PubMed
- Cleveland Clinic – Mullein Benefits
- Herbal Reality: Lung Health
Ready to breathe easier? Try an herbal blend today, and let us know your experience in the comments!
Frequently Asked Questions (FAQs)
1. Are herbal remedies safe for everyone?
Most herbs for lung health are generally safe for adults when used appropriately. However, people who are pregnant, breastfeeding, have chronic diseases (like high blood pressure or kidney issues), or take prescription medications should consult their healthcare provider before starting any herbal supplement.
2. How long does it take to notice results from herbal lung remedies?
Herbs like mullein and thyme may take several days to a few weeks for noticeable effects. Chronic lung issues or recovery from illness may require consistent use for several months. Acute relief (e.g., for cough or congestion) may be noticed within days.
3. Can these herbs replace my inhaler or prescribed medications?
No. Herbal remedies are meant to complement, not replace, prescribed treatments like inhalers, steroids, or antibiotics. Always follow your healthcare provider’s advice and use herbs as supportive care.
4. What’s the best way to use these herbs: tea, capsules, tinctures, or oils?
The best form depends on the herb and your preference:
- Tea: Best for mullein, thyme, marshmallow root.
- Capsules or tinctures: Good for turmeric, licorice, black seed, and standardized extracts.
- Oils: Black seed oil is usually taken by spoon or capsule.
5. Are there any side effects to be aware of?
Some herbs have mild side effects:
- Licorice root: May raise blood pressure and lower potassium.
- Thyme: Rare allergic reactions.
- Turmeric: High doses can cause digestive upset.
- Black seed: Rare stomach upset or allergic reactions.
Always start with low doses and watch for reactions.
6. Can I blend several lung health herbs together?
Yes, many people find blends (like mullein, thyme, and licorice) more effective. Just be mindful of cumulative effects and potential herb–drug interactions.
7. How do I choose a high-quality herbal product?
- Buy from reputable brands.
- Look for organic certification and third-party testing.
- Avoid products with fillers, artificial colors, or unnecessary additives.
- For dried herbs, check for freshness and a strong, clean aroma.
8. Can children use these herbs?
Some herbs (like mullein and thyme in tea form) are safe for children in appropriate, lower doses. Licorice, turmeric, and black seed should be used with pediatrician guidance.
9. Do these herbs help with allergies or just colds and infections?
Many of these herbs, especially mullein, turmeric, and black seed, can help calm allergic inflammation as well as support recovery from respiratory infections. Their anti-inflammatory and mucolytic properties make them useful for a range of lung and airway issues.
10. How do I know if an herb is working for me?
Keep a journal of symptoms—track cough, mucus, breathing ease, and medication use. Improvements may be gradual. If symptoms worsen or new symptoms develop, stop the herb and consult your healthcare provider.