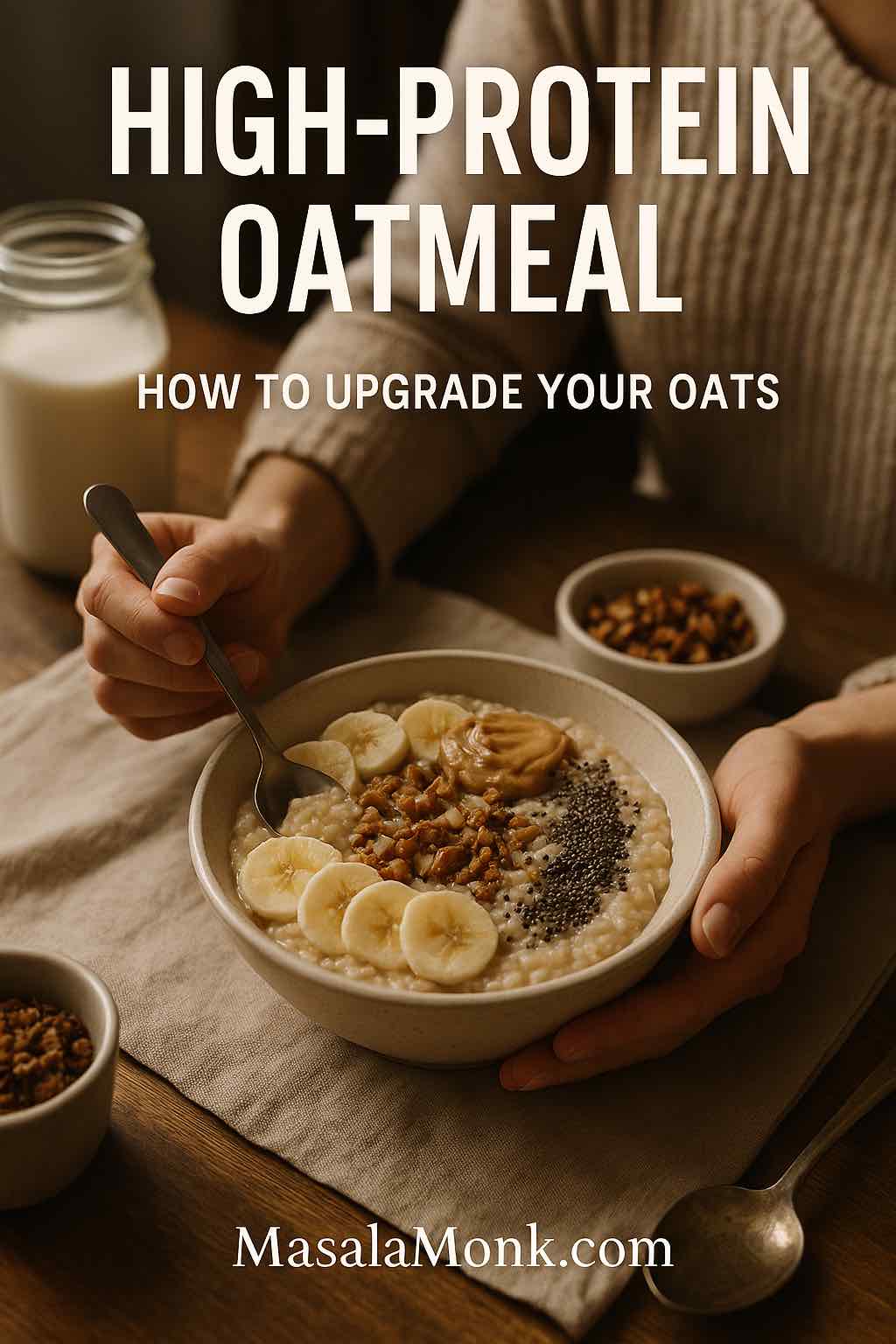
Most people think of oatmeal as “a healthy carb.” It’s warm, comforting, full of fibre… and then you’re hungry again two hours later. Now imagine that same cozy bowl redesigned as a high-protein meal that actually keeps you full, supports your training or weight-loss goals, and still tastes like dessert if you want it to. That’s the idea behind protein oatmeal: you keep everything good about oats and simply upgrade the protein.
In this guide, you’ll learn:
- Why oats are such an excellent starting point
- How much protein you actually get from oats (and why that’s not enough)
- Different ways to build high protein oatmeal – with and without protein powder
- How to tweak your bowl for muscle gain, weight loss, vegan or gluten-free diets
- Flavour ideas so your oatmeal protein breakfast never feels boring
By the end, you’ll have a simple framework you can use to turn any plain oats into a high-protein meal that fits your life.
Also Read: High Protein Overnight Oats | 5 Recipes (Low Calorie, Vegan, Bulking & More)
Why Oats Deserve a Spot in a High-Protein Breakfast
Before you add anything to your oats, it helps to understand why they’re worth eating in the first place.
Oats are one of the most nutrient-dense whole grains available. They provide:
- A generous amount of soluble fibre, especially beta-glucan, which supports heart health and more stable blood sugar
- Complex carbohydrates that digest slowly
- Useful amounts of vitamins, minerals and antioxidant compounds
If you want a clear, friendly overview of oat types, benefits and basic nutrition, MasalaMonk already has a detailed guide to oats, types and nutrition. It walks through steel-cut, rolled, quick and instant oats, and explains how each behaves in your bowl.
In addition, articles on major health sites consistently link regular oatmeal consumption to improved cholesterol profiles, better blood sugar control and long-term heart health. Oats are often highlighted as one of the top whole grains to include in a heart-supportive diet.
So from a health perspective, oats already do a lot:
- The fibre helps with appetite and digestion.
- The slow carbs give you steady energy rather than a hard crash.
- The nutrients quietly check off several boxes in your daily needs.
However, there’s one big limitation: protein.
Also Read: The Science of Protein: Maximizing Muscle Growth and Recovery
How Much Protein Is in Oats – and Why It’s Not Enough
Oats have a reputation as a higher-protein grain, and that’s true compared with many cereals. Yet the actual numbers matter.
Most nutrition databases show that:
- 100 g of dry oats provide roughly 13–17 g of protein (depending on variety and brand).
That certainly makes oats more protein-dense than, say, rice. Nevertheless, most people don’t eat 100 g of dry oats in one sitting. A typical portion might be:
- 40–50 g dry oats (around ½ cup), which only gives 5–7 g of protein.
That’s… okay. It’s better than a sugary breakfast cereal, but it doesn’t come close to the 20–30 g of protein that many people aim for in a high protein oatmeal breakfast.

Meanwhile, research on higher-protein breakfasts suggests:
- Meals with more protein tend to improve appetite control later in the day.
- People often experience fewer cravings and less late-night snacking when breakfast has a solid protein dose.
So oats alone are “protein friendly,” yet they don’t automatically become high protein oatmeal on their own. To reach that level, you need to layer proteins onto the oat base.
That’s good news, because it means you can keep everything you like about oats and simply upgrade them instead of replacing them.
Also Read: 10 High Calorie Protein Shakes & Smoothie Recipes for Healthy Weight Gain
Step 1: Choose the Right Oats for Your Protein Bowl
The type of oats you start with changes cooking time, texture and even how “heavy” the meal feels. Once you choose your base, it becomes much easier to design your version of protein oatmeal.
Rolled, Steel-Cut or Quick: Which Is Best?
For everyday high protein oatmeal, you’ll usually work with three main options:
- Rolled / Old-Fashioned Oats
- Steamed and flattened whole oats
- Cook in just a few minutes
- Turn soft and creamy, ideal for classic porridge
- Steel-Cut Oats
- Whole oat groats chopped into pieces
- Need more simmering time
- Stay chewy and nutty, with a slightly lower glycaemic impact
- Quick or Instant Oats
- More finely processed
- Cook quickly or even just by soaking
- Can turn mushy if overcooked

If you’d like a deep comparison, have a look at MasalaMonk’s breakdown of steel-cut oats vs rolled oats. It goes into texture, cooking methods and nutrition in much more detail, and it’s a helpful companion piece if you’re trying to decide which to stock at home.
For protein oatmeal, rolled oats are usually the most practical choice: they cook fast, hold mix-ins well and can be used in the microwave, on the stove or baked. Steel-cut oats work beautifully on days when you want something hearty and leisurely. Quick oats shine when you need a high protein oatmeal in under five minutes.
If you ever wonder whether you can swap different oat types in recipes, MasalaMonk also answers that in a simple guide to substituting old-fashioned oats for rolled oats. Knowing how flexible oats actually are makes it easier to experiment.
A Word on “Oats” vs “Oatmeal”
Sometimes people use “oats” and “oatmeal” as if they were the same thing. Technically:
- Oats are the raw grain (rolled, steel-cut, instant, etc.).
- Oatmeal is the prepared dish—what you actually eat from the bowl.
If that distinction ever feels fuzzy, MasalaMonk has a short explainer on the difference between oats and oatmeal that clears things up in everyday language.
Once your base is clear, you can move on to the next decision: what to cook the oats in.
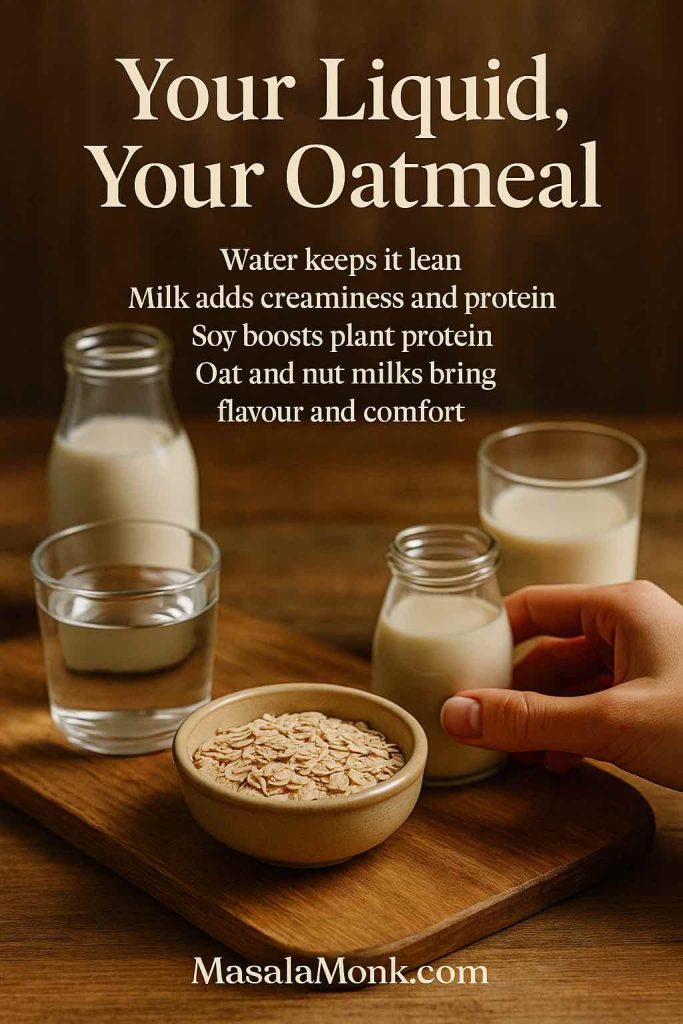
Step 2: Liquids That Quietly Boost Your Protein
The liquid you choose influences flavour, creaminess and, in some cases, the total protein content of your oatmeal.
Here are the main contenders:
Water
- Zero calories from the liquid
- Very neutral base
- Leaves all the work to your add-ins
Cow’s Milk
- Adds extra protein, calcium and creaminess
- Works well for both sweet and savoury bowls
Soy Milk
- The highest-protein plant milk
- Excellent choice for high protein vegan oatmeal
Oat Milk, Almond Milk and Others
- Lovely texture and flavour
- Lower in protein but often fortified with vitamins and minerals
- Great when you rely on other ingredients for the main protein boost
If you enjoy doing things from scratch, you can even make your own oat milk and then cook your oats in it. MasalaMonk’s method for easy homemade oat milk is designed to avoid the classic slimy texture people complain about.
There’s also a full discussion of oat milk and its benefits, including how it may support weight management and digestion. That information can help you decide when oat milk belongs in your protein oatmeal, and when you might prefer dairy or soy instead.
At this point, you have a base:
- The kind of oats you like
- A liquid that fits your preferences
Next, you can finally add the star of the show: protein.
Also Read: How to make Almond Milk at Home
Step 3: Oatmeal with Protein Powder – The Quickest Upgrade
When people look for “oatmeal with protein powder,” “protein powder oats” or “oatmeal and protein powder,” they’re usually looking for a shortcut. They want high protein oatmeal that’s fast, simple and predictable.
Protein powder fits that brief perfectly.
Choosing a Protein Powder for Oatmeal
Several types of protein powders work well with oats. The best one for you depends on taste, digestion, budget and whether you eat animal products.
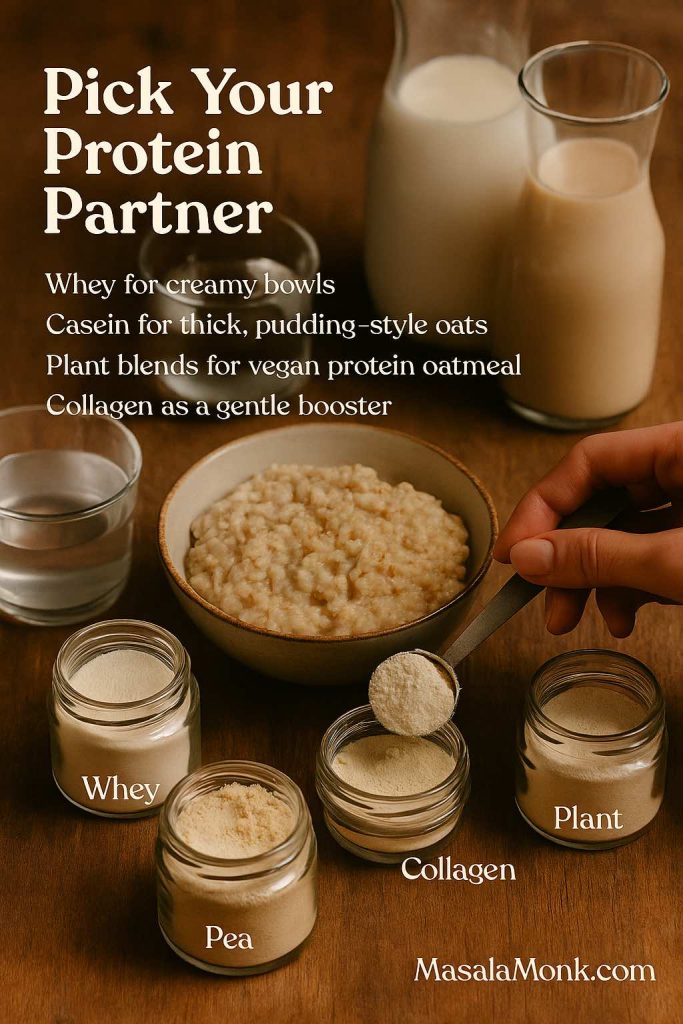
Here’s how they generally behave:
Whey Protein
- Mixes very easily
- Tends to give you the creamiest texture
- Ideal for chocolate protein oatmeal, vanilla bowls, mocha oats and other dessert-style flavours
Casein Protein
- Thickens more than whey
- Fantastic when you want a pudding-like effect, almost like a custard or thick protein porridge
- Often very filling, which is useful for appetite control
Plant-Based Proteins (Pea, Soy, Rice–Pea Blends)
- Essential for oatmeal high in vegan protein.
- Might be slightly thicker or more “earthy” in flavour, but blends improve every year
- Work very well when you pair them with spices, cocoa or fruits
Collagen Powder
If you’re trying to build more plant-forward meals, have a look at MasalaMonk’s list of plant-based protein sources for meal prep. Many of those ingredients also slide neatly into high protein oatmeal bowls.
How to Add Protein Powder Without Ruining Your Oats
Nobody wants lumpy, chalky oatmeal. Fortunately, there’s a simple method that makes oatmeal with protein powder smooth and enjoyable:
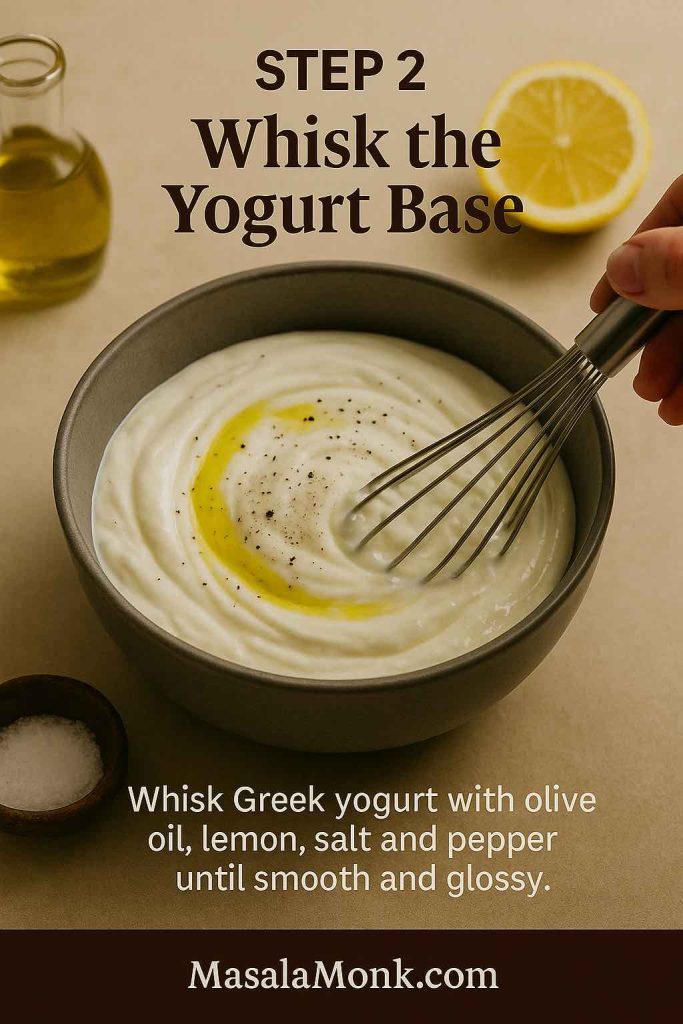
- Cook your oats with water or milk until they’re just how you like them.
- Take the pan off the heat and let it stand for a minute so the mixture stops bubbling.
- In a separate cup or small bowl, whisk your protein powder with a little liquid to create a smooth, pourable paste.
- Stir that paste into the warm oats until everything looks creamy and uniform.
You can then adjust thickness with more liquid if needed.

This technique works beautifully for:
- Vanilla protein oatmeal topped with banana and cinnamon
- Chocolate porridge protein with cocoa powder and a few dark chocolate shavings
- Berry-heavy bowls where the oats and powder form a base for strawberries, blueberries or cherries
Finally, if you prefer to drink your breakfast, you can turn this into a high protein oatmeal shake. Blend cooked oats, liquid and protein powder until completely smooth, then add ice or frozen fruit for a milkshake-like texture.
Also Read: Healthy Wholewheat Carrot Chia Seed Pancakes- Vegetarian High Protein Recipe
Step 4: High Protein Oatmeal Without Protein Powder
Protein powders are convenient, yet they’re not mandatory. You can still build protein rich oatmeal using everyday foods you probably already have in your kitchen.
Egg Whites and Whole Eggs
One of the simplest ways to raise the protein content of oatmeal is to add egg whites directly into the pot.
Egg whites are:
- Almost pure protein
- Very low in fat and carbohydrate
- Mild in flavour when cooked properly
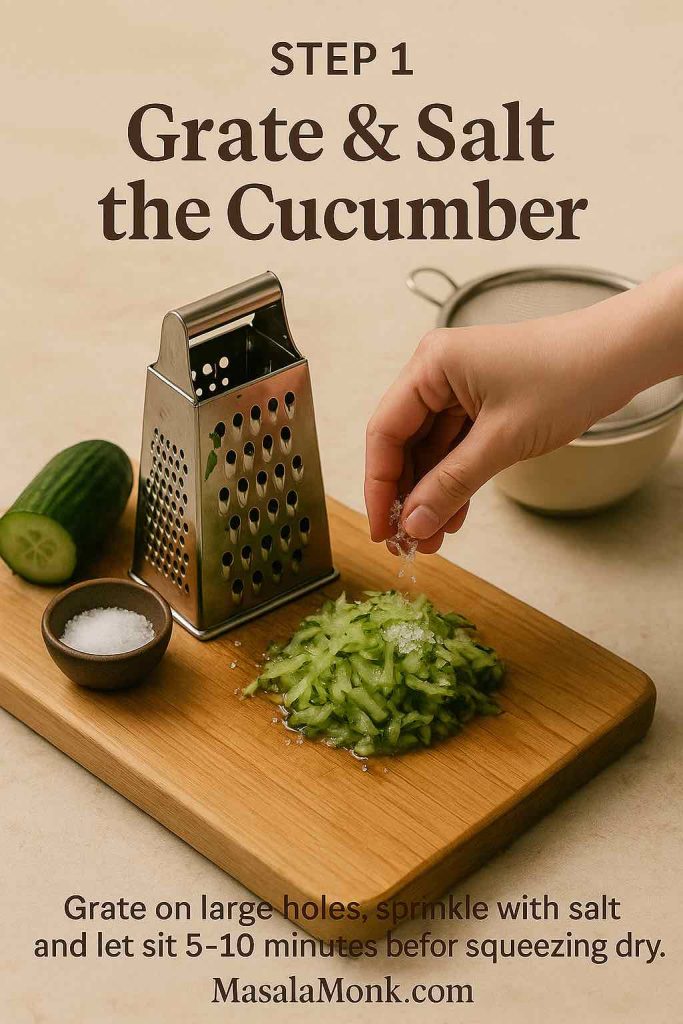
To make egg white oatmeal, you can:
- Cook your oats in water or milk as usual.
- Turn the heat down to low once they’re nearly done.
- Slowly pour in liquid egg whites while whisking continuously.
- Keep stirring for another minute or two until the mixture thickens and the eggs are cooked.
The result is a subtly fluffy, silky high protein oatmeal that doesn’t taste like scrambled egg. This method is ideal for low calorie high protein oatmeal, particularly if you combine it with water or low-fat milk.
If you use a microwave, simply cook your oats in a deep bowl until almost done, stir in whisked egg whites, then microwave again in short bursts, stirring in between to avoid overcooking.
For even more protein, you can add one whole egg (for richness and nutrients) plus extra whites (for volume and total protein) in the same way.
Also Read: Egg Yolks or Yellow: Nutritional & Protein Profile

Greek Yogurt, Curd, Cottage Cheese and Paneer
Dairy is another excellent way to transform plain oats into high protein oatmeal without any powders.
A few effective combinations include:
- Oats cooked with water, then cooled slightly and mixed with thick Greek yogurt
- Porridge swirled with hung curd or a high-protein curd
- Warm oatmeal topped with soft paneer or cottage cheese, either plain or lightly blended
These additions not only increase protein, they also boost creaminess and tang. You can easily create a bowl that feels indulgent while still staying within your calorie target.
This method works especially well for:
- High protein oatmeal for weight loss – use low-fat dairy and plenty of fruit or spices
- Bulking oatmeal – use full-fat versions and add nuts or nut butter on top
Because the dairy is stirred in after cooking, you maintain control over the final texture. You can keep things thick like a cheesecake, or loosen them into a smoother high protein porridge.
Also Read: is Greek Yogurt A Healthy Choice for People with Diabetes?
Nuts, Seeds and Nut Butters
Nuts and seeds play two roles in protein oatmeal:
- They add extra protein and healthy fats.
- They provide crunch and flavour, which makes your bowl more satisfying.
Some favourites are:
- Peanut butter, almond butter or cashew butter
- Chopped almonds, walnuts, peanuts or pistachios
- Chia, flax and hemp seeds
A classic example is oatmeal with peanut butter protein and banana. This combination hits all the right notes: creamy, slightly salty, naturally sweet and very filling. If that pairing interests you, it’s worth reading MasalaMonk’s detailed article on oatmeal and peanut butter for effective weight loss. It explains how the blend of fibre, protein and fat can support hunger management instead of fighting it.
Similarly, oats and chia seeds for weight loss shows how combining those two ingredients gives you both protein and fibre in a single scoop. That’s exactly what you want when you’re building high fibre high protein oatmeal that keeps you full for hours.
Also Read: Benefits of Nuts and Seeds – Protein-Packed Superfoods
High Protein Oatmeal for Muscle Gain and Bulking
Once you understand the building blocks, you can tune your bowl for different goals. Let’s start with muscle gain and strength training.
When your focus is building muscle, calories and protein both matter. You’re often aiming for:
- A calorie surplus to support growth
- Plenty of protein for recovery and repair
- Enough carbohydrates to fuel workouts
In this context, your protein oatmeal becomes more than breakfast; it’s part of your training gear.
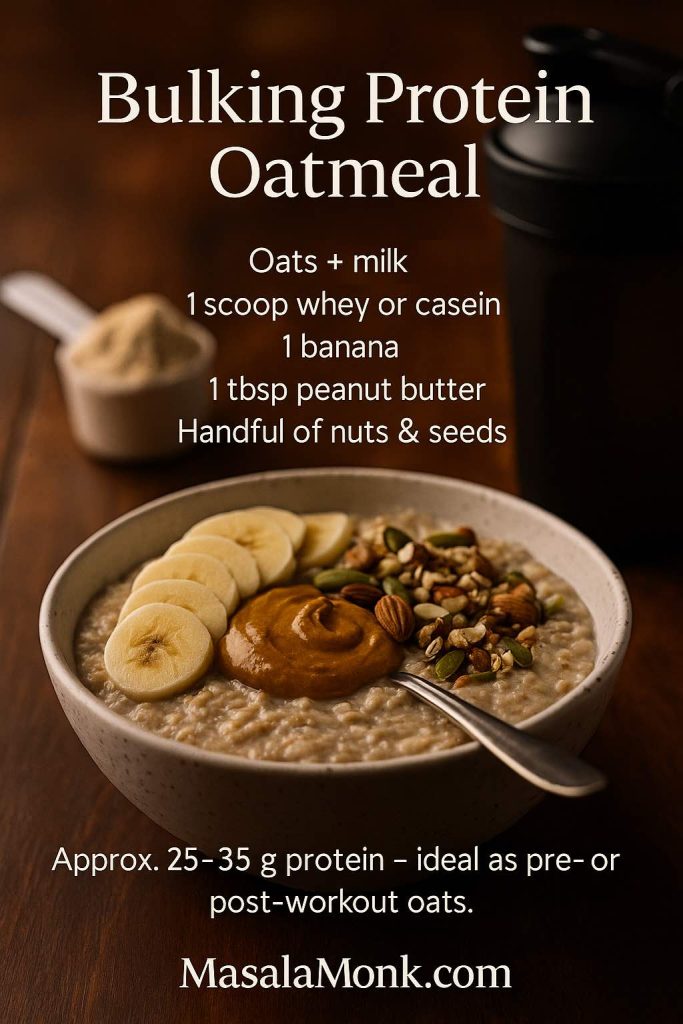
A bulking-oriented bowl might look like this:
- Rolled or steel-cut oats cooked in milk
- Whey or casein protein mixed in after cooking
- A sliced banana for extra carbohydrates and sweetness
- A spoon of peanut butter or almond butter
- A sprinkle of nuts and seeds on top
That kind of bowl easily turns into bodybuilder oatmeal with 25–35 g of protein, substantial carbs and healthy fats. It’s perfect as oats for pre-workout or even as a post-training meal when you want something warm instead of a shake.
To see how a breakfast like this fits into your total daily intake, MasalaMonk’s guide on how to eat 100 grams of protein a day can be helpful. When your first meal is already a serious oatmeal protein breakfast, hitting that number becomes far easier.
High Protein Oatmeal for Weight Loss and Appetite Control
On the flip side, you might be trying to lose fat or manage your weight. In that case, you still want high protein oatmeal, but with a different emphasis:
- Enough protein to protect muscle and control hunger
- Plenty of fibre and volume
- Moderated calories and sugars
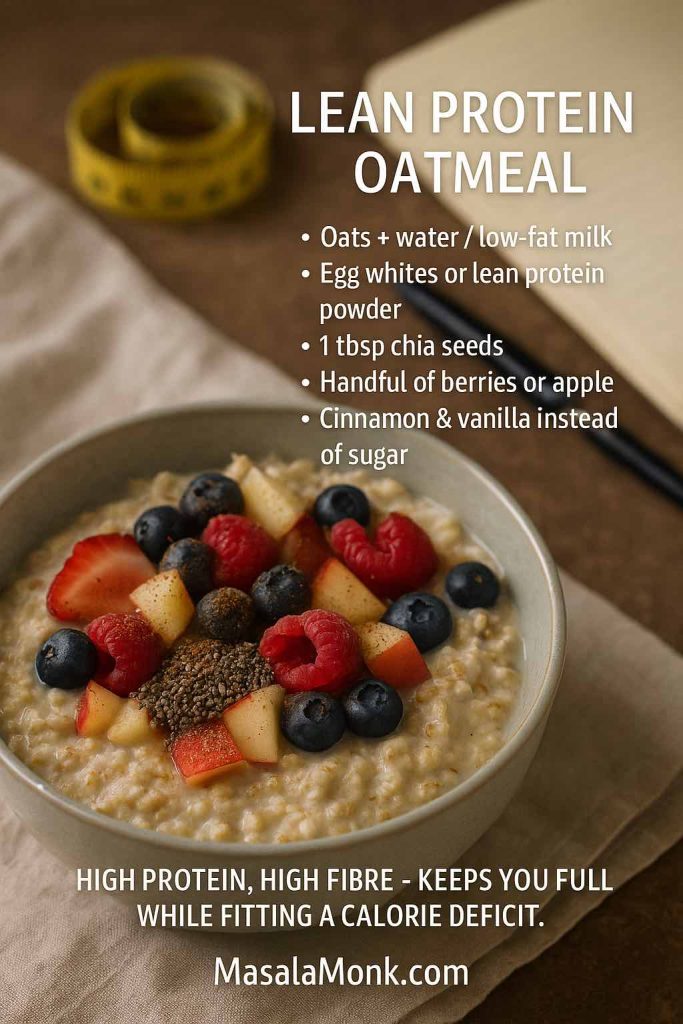
A weight-loss-oriented bowl could look like this:
- A moderate portion of oats, cooked in water or a mix of water and low-fat milk
- Egg whites or a scoop of lean protein powder for high protein low calorie oatmeal
- Chia seeds for thickness and extra fibre
- A generous handful of berries or chopped apple
- Cinnamon and vanilla for flavour instead of lots of sugar
This type of high protein oatmeal for weight loss is designed to:
- Keep you full until your next meal
- Fit into a calorie deficit
- Feel like a proper breakfast rather than “diet food”
Because oats already support steady blood sugar and digestion, and added protein increases satiety, combining them intelligently can make it easier to stay consistent with your plan.
Vegan High Protein Oatmeal
If you follow a plant-based diet, oats are one of your best friends. They’re naturally vegan, widely available and extremely flexible. You simply need to make sure you pair them with solid plant proteins.
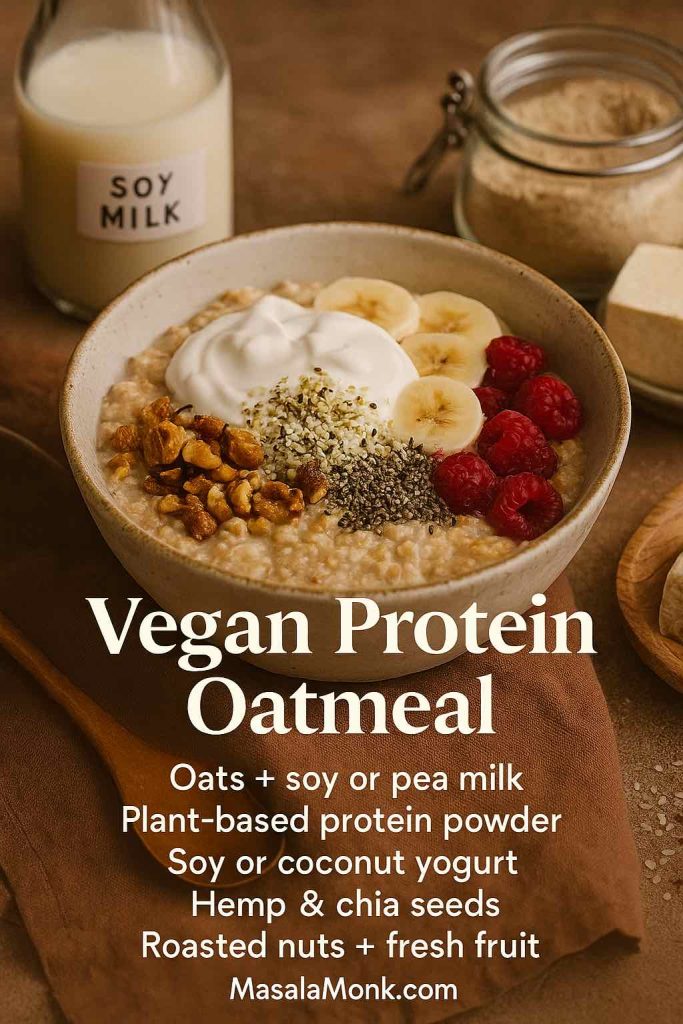
A vegan-friendly high protein oatmeal might include:
- Oats cooked in soy milk or a fortified pea-based drink
- A plant-based protein powder (pea, soy or a blend)
- Soy yogurt or coconut yogurt stirred in at the end
- Hemp seeds, chia seeds and roasted nuts for crunch and extra protein
You can easily reach 20–25 g of protein in a bowl like that, especially if you’re generous with soy milk and a decent scoop of vegan protein.
If you’d like more ideas for plant-based proteins to plug into your protein oatmeal, MasalaMonk’s post on plant-based protein sources for high-protein meal prep is a great starting point. Several of the ingredients there—beans, lentils, tofu, tempeh, seeds and nuts—can be adapted to both sweet and savoury oat bowls.
There’s also a playful guide to using tofu instead of eggs in breakfast which can give you even more ideas for protein-rich, plant-based mornings.
Gluten-Free Protein Oatmeal: Doing It Safely
Many people who follow a gluten-free diet would love to enjoy oats, yet they’re understandably cautious. The situation is a little nuanced.
On one hand, pure oats are naturally gluten-free. The main proteins in oats are called avenins, not gluten. On the other hand, oats are often grown, transported or processed in facilities that also handle wheat, barley or rye. Because of that, they can easily become contaminated with gluten.
Coeliac-focused organisations explain that:
- Certified gluten-free oats are produced and tested to contain less than a small threshold of gluten (typically 20 parts per million).
- Most people with coeliac disease can tolerate these certified oats.
- A small percentage are sensitive even to pure oats and may need to avoid them entirely.
If you’d like to read more, Beyond Celiac’s overview of oats and the gluten-free diet and Celiac Canada’s statement on oats both summarise the current thinking very clearly.

To enjoy gluten free protein oatmeal safely, you can:
- Choose certified gluten-free oats
- Check your protein powders for hidden gluten sources
- Be careful with toppings such as granola or flavoured additions that might include malt, barley or wheat
Once you’ve covered that base, you can use all the same protein-boosting strategies—egg-free if needed—to build high protein gluten free oatmeal that feels just as comforting as any other bowl.
Also Read: All About Gluten: Symptoms, Testing, Diet & 7-Day Gluten-Free Meal Plan
Flavour Ideas for Protein Oatmeal (Without Losing the Macros)
Now that the structure is clear, it’s time for the fun part: flavour. The beauty of protein oatmeal is that you can dress it up in almost any direction while keeping the macros on your side.
Here are a few themes you can play with.
Chocolate Protein Oatmeal
This one is perfect when you want breakfast to taste like dessert.
- Rolled oats cooked in milk or soy milk
- Chocolate or cocoa-flavoured protein powder blended in after cooking
- A spoon of Greek yogurt or soy yogurt for extra creaminess
- Berries and a few dark chocolate chips on top
By adjusting the amount of sweetener and chocolate, you can tilt this bowl toward high protein low sugar oatmeal or make it a richer treat for bulking phases.
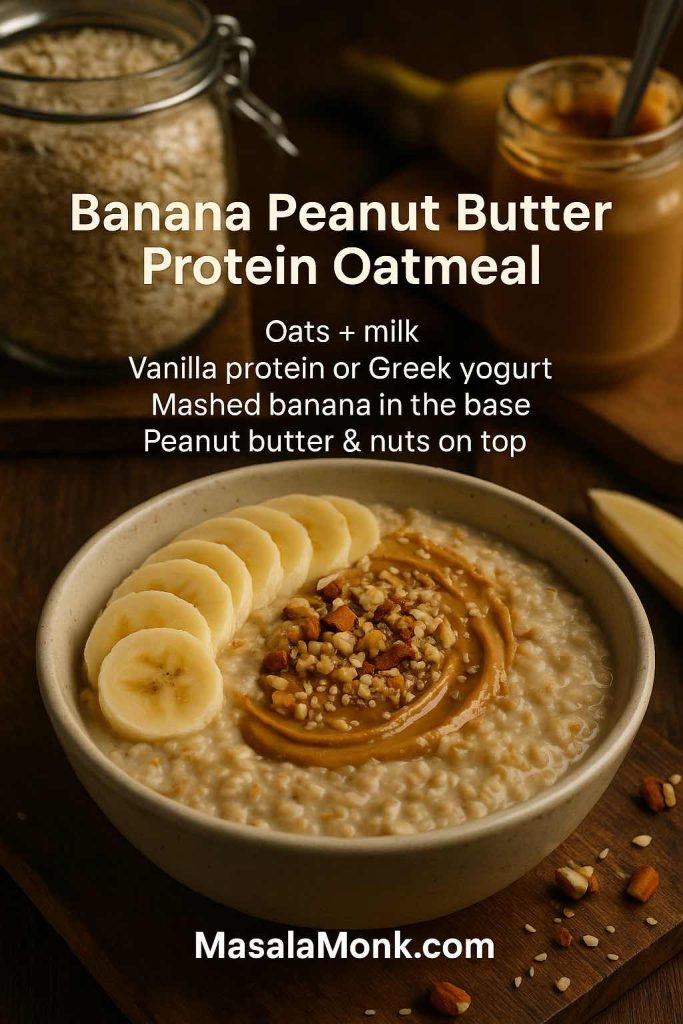
Banana Peanut Butter Protein Oatmeal
This bowl feels like comfort in a mug: warm, nutty, slightly salty and sweet.
- Oats cooked in milk
- Vanilla protein powder or a big spoon of Greek yogurt
- Mashed ripe banana stirred in
- A swirl of peanut butter and some chopped nuts on top
The mix of fibre, protein and fats here makes this classic oatmeal peanut butter protein bowl very satisfying. For more ideas in this flavour lane, you can dig into MasalaMonk’s article on oatmeal and peanut butter as a power combo.
Apple Cinnamon Protein Oatmeal
Think of this as apple pie for breakfast, minus the pastry.
- Oats cooked with water or milk
- Vanilla protein powder, yogurt or cottage cheese mixed through
- Diced apple simmered with the oats or briefly sautéed with a bit of cinnamon
- Ground cinnamon, nutmeg and a teaspoon of maple syrup or date syrup
With a few tweaks, this becomes either a lean high protein oatmeal or a more indulgent autumn bowl, and it naturally matches phrases like “apple cinnamon protein oatmeal” and “cinnamon protein oatmeal” without forcing anything.
Maple Brown Sugar Protein Oatmeal (Lightened)
Those maple brown sugar packets are nostalgic, but they’re easy to upgrade.
- Cook oats in a mix of water and milk.
- Stir in plain or lightly sweetened protein powder.
- Add a small spoon of brown sugar and a drizzle of maple syrup—less than you’d usually use.
- Finish with plenty of cinnamon and a pinch of salt.
Here, most of the sweetness comes from a modest amount of sugar and the natural flavour of oats and milk, while protein acts as the backbone. That’s how you end up with low sugar protein oatmeal that still tastes like the original.
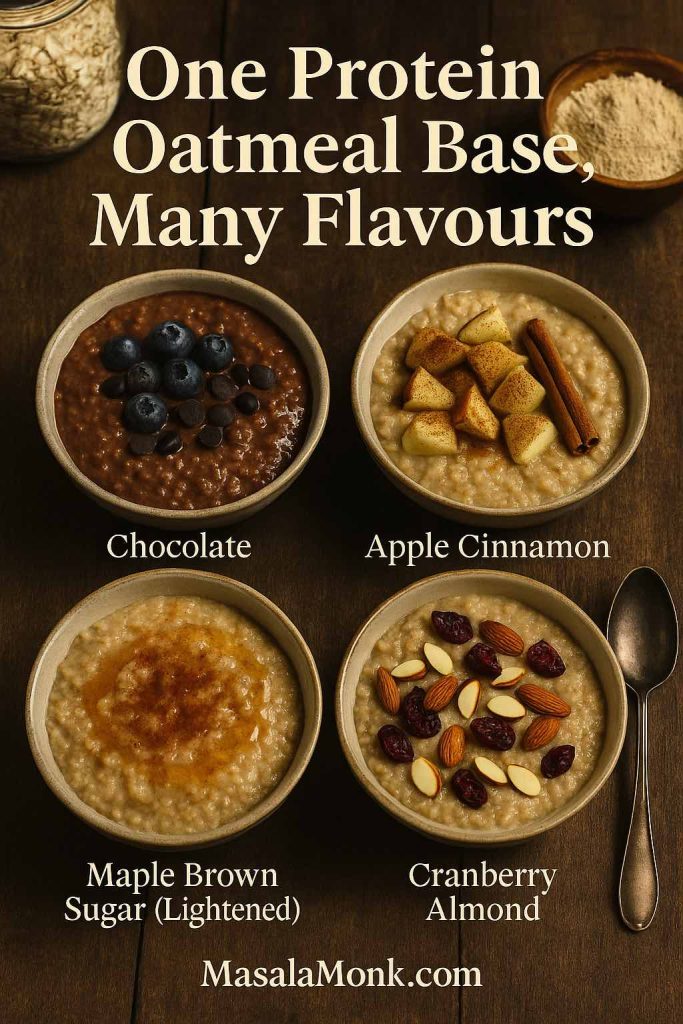
Cranberry Almond Protein Oatmeal
For something brighter and slightly tart:
- Oats cooked in milk or soy milk
- Protein blended into the base
- A handful of sliced almonds
- A sprinkle of dried cranberries or fresh cranberries cooked down briefly with a touch of sweetener
This variation is an easy way to enjoy “cranberry almond” style oats while keeping a firm eye on protein and fibre.
Also Read: Basics of Macronutrients: Diet’s Building Blocks
Beyond the Bowl: Protein Oats as Bars, Puddings and Snacks
Once you’re comfortable building protein oatmeal, it’s natural to wonder what else you can do with oats and protein. The same ingredients often morph beautifully into bars, puddings and grab-and-go snacks.
If you like the idea of portable oat-based snacks, you might enjoy:
- Healthy Oat Protein Bars – 5 Easy No Sugar Recipes – perfect when you want the feeling of a protein packed oatmeal bowl in bar form.
- Oat Bars: The Perfect Snack or Breakfast (No Sugar, No Baking) – a quick, no-bake option for busy days.
For a more dessert-like approach, chia pudding with steel-cut oats and mango shows how oats and chia can transform into a cold, spoonable treat that still offers plenty of fibre and some protein.
All of these recipes work on the same core principle you’re using for protein oatmeal: combine oats, protein sources and fibre, then adjust flavours and textures to suit your tastes.
Where Overnight Oats Fit In
You might have noticed that this guide focuses mostly on hot or freshly prepared oats. That’s deliberate.
Overnight oats are essentially cold oatmeal made in advance. They soak instead of simmering, but they rely on the same ideas:
- A base of oats
- A liquid
- Protein sources like yogurt, milk or protein powder
- Flavourings and toppings
Because MasalaMonk already has a full guide to jar-based recipes, you can treat this article and that one as siblings:
- Use this piece when you’re thinking about hot protein oatmeal, microwave oats and stovetop porridge.
- Switch to the dedicated guide to high protein overnight oats when you want set-and-forget jars that live in the fridge and are ready when you wake up.
The underlying logic is the same; the difference is mainly temperature and convenience.
A Simple Framework You Can Use Every Day
Instead of memorising dozens of recipes, it’s often more helpful to keep a simple framework in mind. Once you understand the structure, you can improvise endlessly.
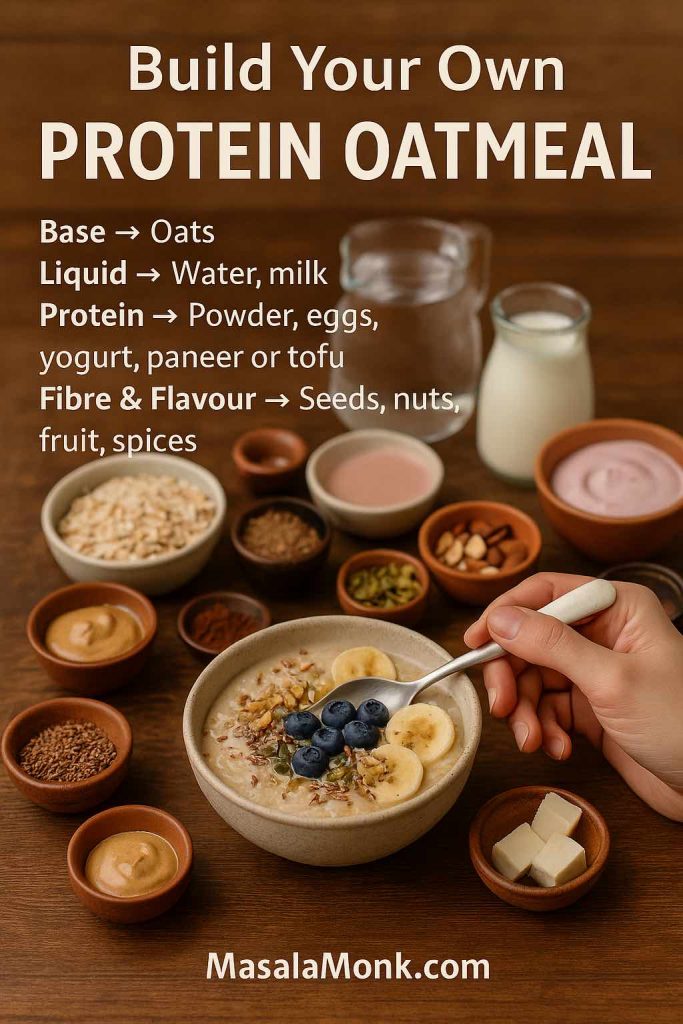
Think of high protein oatmeal like this:
- Base
- 40–60 g oats (rolled, steel-cut or quick)
- 40–60 g oats (rolled, steel-cut or quick)
- Liquid
- Enough water, milk or plant milk to reach your favourite consistency
- Enough water, milk or plant milk to reach your favourite consistency
- Main Protein
- 1 scoop of protein powder or
- Several egg whites or
- A generous amount of yogurt, curd, cottage cheese, paneer or tofu
- Fibre and Extras
- Chia, flax or hemp seeds
- Fruits or grated vegetables
- Nuts or nut butters
- Flavour
- Cocoa, vanilla, cinnamon, cardamom, nutmeg, citrus zest, coffee, fruit, or a touch of sweetener
From there, you simply adjust:
- More oats + nut butter + toppings → bulking oatmeal and bodybuilder oatmeal
- Fewer oats + extra egg whites or lean protein + lots of berries → low calorie high protein oatmeal
- Soy milk + vegan protein + plant yogurt → high protein vegan oatmeal
- Certified gluten-free oats + careful choice of protein powder → gluten free protein oatmeal
Once you’ve played with this a few times, upgrading your oats stops feeling like a “recipe” and becomes second nature. You’ll look at a bowl of plain oats and immediately see three or four different ways to turn it into a high-protein meal that actually matches your day.
And that’s the real power of protein rich oatmeal: it’s not just one dish, it’s a flexible system. You start with oats, you layer in protein, you add fibre and flavour, and you walk away from the table feeling properly fed—rather than wondering what snack you’re going to hunt down next.
FAQs
1. How much protein is in oatmeal, and what makes it “protein oatmeal”?
Plain oats usually provide around 5–7 grams of protein per ½ cup (40–50 g) of dry oats. That’s more than most breakfast cereals, but on its own it’s still not a high protein meal.
You turn it into protein oatmeal by adding extra protein sources like whey or plant protein powder, egg whites, Greek yogurt, cottage cheese, tofu, or soy yogurt until the bowl reaches roughly 15–30 grams of total protein.
2. What is the best protein for oats?
The “best protein for oats” depends on your preferences and goals:
- Whey protein mixes smoothly and is great for creamy high protein oatmeal.
- Casein protein makes thicker, more filling bowls and works well for dessert-style oats.
- Pea or soy protein are excellent options if you want high protein vegan oatmeal.
- Egg whites or Greek yogurt are ideal when you prefer whole foods over powders.
As long as you enjoy the taste and digest it well, it can become your best protein for oats.
3. How do I add protein powder to oatmeal without clumps?
To make smooth oatmeal with protein powder, cook your oats first and let them cool slightly. Separately, whisk the protein powder with a small amount of liquid into a thin paste. After that, stir this paste into the warm oats until everything is blended. This approach avoids chalky lumps and gives you creamy protein oatmeal every time.
4. Does heating protein powder in oatmeal destroy the protein?
Gently heating protein powder in oatmeal and protein powder recipes will not destroy the protein or make it useless. Moderate cooking temperatures might change texture a bit, but the amino acids remain intact. However, extremely high, prolonged heat can sometimes affect flavour, so it’s usually better to stir protein powder into warm oats after cooking instead of boiling it for a long time.
5. How can I make high protein oatmeal without protein powder?
If you don’t want to use any powders, you can still build high protein oatmeal by combining oats with:
- Egg whites or whole eggs
- Greek yogurt or hung curd
- Cottage cheese or paneer
- Tofu or soy yogurt
- Nuts, seeds and nut butters
Blending these into your bowl creates protein rich oatmeal with impressive macros, even though there is no protein powder.
6. Is oatmeal good for bodybuilding and muscle gain?
Yes, oatmeal can be excellent for bodybuilding when you turn it into high protein oatmeal. Oats provide slow-digesting carbohydrates and fibre, which support training performance and steady energy. When you mix in enough protein from powders, egg whites, dairy or tofu, you get bodybuilder oatmeal that fits perfectly into a muscle gain meal plan. It’s especially useful as a pre-workout or post-workout meal when you want sustained fuel rather than a fast sugar hit.
7. Can I eat protein oatmeal for weight loss?
Absolutely. In fact, oatmeal and protein powder for weight loss is a very common strategy. A bowl of low calorie high protein oatmeal made with a moderate amount of oats, lean protein (like egg whites or low-fat Greek yogurt), berries and chia seeds can keep you full for hours. The combination of fibre and protein helps manage appetite, so you’re less likely to overeat later in the day, as long as your overall calorie intake stays in a deficit.
8. What’s the difference between protein oatmeal and high protein porridge?
The terms often overlap. In many cases:
- Protein oatmeal refers to any oatmeal that has been upgraded with extra protein.
- High protein porridge is usually hot, spoonable oats with a thicker, more traditional porridge texture.
In practice, both describe oats cooked with liquid and fortified with ingredients like protein powder, egg whites, yogurt, or paneer. The exact word you use matters less than making sure the bowl has enough protein for your needs.
9. Are proats and overnight protein oatmeal the same thing?
“Proats” is a casual term that usually means “protein oats.” It can refer to hot oats with protein powder or to overnight protein oatmeal stored in jars. On the other hand, overnight oats specifically soak in the fridge instead of cooking on the stove. So:
- All overnight protein jars are a type of proats.
- Not all proats are overnight oats, because some are cooked and served hot.
Both formats use the same idea: oats plus liquid plus a protein source.
10. How do I make low calorie high protein oatmeal that’s still filling?
For low calorie high protein oatmeal, focus on three things:
- Portion control for oats – use a moderate amount (e.g., 30–40 g dry) instead of a huge serving.
- Lean protein – add egg whites, low-fat yogurt, cottage cheese or a lean protein powder to raise protein without many extra calories.
- Volume and fibre – stir in grated zucchini or carrot, chia seeds, berries or apple to bulk up the bowl and slow digestion.
This combination creates a big, satisfying portion of high protein oatmeal without pushing your calories too high.
11. Can I have protein oatmeal at night?
Yes, you can enjoy protein oatmeal in the evening as well. Many people like a warm bowl of oats as a pre-bed snack, especially when they add slow-digesting protein like casein, paneer or Greek yogurt. This kind of high protein porridge can help you feel relaxed and keep hunger away overnight. Just consider your total daily calories and your personal digestion; some prefer lighter meals very close to bedtime.
12. Is oatmeal high in protein compared to other grains?
Oats are relatively high in protein compared to many other grains, which is why people talk about oats high in protein. However, even though 100 g of dry oats may contain 13–17 g of protein, a typical serving is smaller, so it’s not enough to qualify as a full high protein meal. That’s why combining oats with eggs, dairy, tofu or protein powder is so effective: you retain the advantages of oats while lifting total protein to a more substantial level.
13. What is the best type of oats for protein oatmeal?
You can turn any oat type into protein oatmeal, but some work better for certain preferences:
- Rolled oats are versatile and ideal for most bowls.
- Steel-cut oats are great for chewier, slow-cooked high protein porridge.
- Quick oats are perfect when speed matters and you want almost instant breakfast.
Ultimately, the best oats are the ones you enjoy eating and can cook consistently, because consistency matters more than tiny differences in macros.
14. How do I make high protein vegan oatmeal?
To create high protein vegan oatmeal, combine oats with plant-based proteins:
- Cook oats in soy milk or pea-based milk.
- Add a scoop of vegan protein powder (pea, soy or a blend).
- Stir in soy yogurt or coconut yogurt for extra creaminess.
- Top with hemp seeds, chia seeds, nuts and nut butter.
By layering these ingredients, you can easily build high protein vegan oatmeal bowls with 20–25 grams of protein or more, without using any animal products.
15. Can I prep protein oatmeal in advance?
Yes, there are several ways to prep protein oatmeal ahead of time:
- Cook a batch of plain oats and store in the fridge, then reheat with extra liquid and add protein just before serving.
- Prepare jar-style proats with oats, liquid and protein powder or yogurt to keep in the fridge for a few days.
- Bake oat-based dishes like protein oat bars, which you can grab as a portable breakfast.
As long as you store everything in the fridge and reheat gently, prepped high protein oatmeal can make busy mornings much easier while still giving you a balanced start to the day.