Plenty of people reach for psyllium (the soluble fiber in Metamucil) to smooth out digestion, encourage regularity, and even give LDL cholesterol a nudge in the right direction. Still, it’s wise to understand the metamucil side effects you might feel in the first days, along with the simple habits that make them far less likely. Because psyllium gels, holds water, and changes stool texture, your gut needs a brief adjustment period. With thoughtful dosing, solid hydration, and realistic timing, most readers adapt quickly and carry on comfortably.
For clarity and accuracy, you can confirm label instructions and safety language on the official listing at DailyMed (see the Metamucil psyllium label (warnings & directions)), skim a concise consumer summary on MedlinePlus: Psyllium for constipation self-care basics, and — if IBS is part of your story — review the ACG Clinical Guideline for IBS for how soluble fiber fits into modern care. Meanwhile, for practical, product-specific tactics, our MasalaMonk guide on when to take Metamucil compares real-world routines without the fluff.
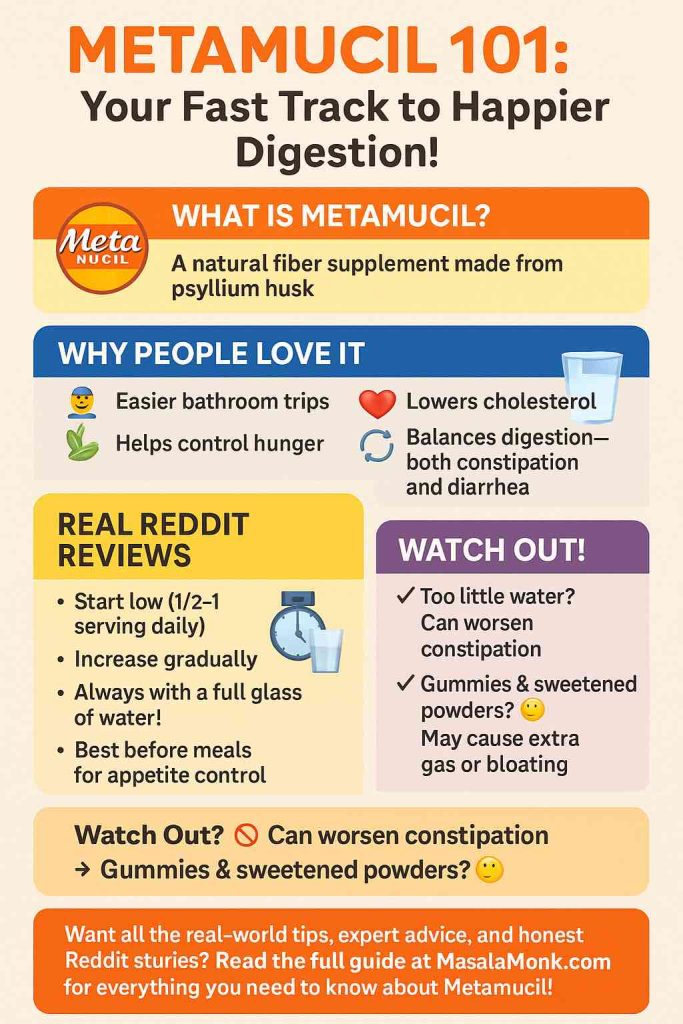
Is daily Metamucil safe?
Broadly, yes. Daily psyllium is generally considered safe for most adults when taken per label with adequate fluids. Moreover, many gastroenterology groups suggest soluble fiber, particularly psyllium, as an initial strategy for chronic constipation and a helpful add-on for numerous people with IBS. “Safe,” however, isn’t automatic; it depends on behaviors like mixing powder thoroughly, drinking a full glass of water with each serving, and increasing the dose gradually instead of jumping straight to a “goal” amount.
Because the active ingredient is psyllium husk (also called isabgol/ispaghula), you might want a broader primer on the ingredient itself. For a plain-language overview that goes beyond brands, see our explainer on psyllium husk side effects. For authoritative label phrasing — including the choking warning — the DailyMed entry is your north star; start with the Metamucil psyllium label and, if you’re comparing formats, you can also check an alternate psyllium SKU to see the same core warnings.
Common metamucil side effects (and why they happen)
Even though psyllium is gentle for many, your digestive system will notice the change. Early effects tend to be mild and temporary, settling as your microbiome adapts. Understanding the “why” helps you correct course quickly.
Gas and bloating as one of the Side Effects of Metamucil
First, the common one. Because psyllium is soluble and gel-forming, it slows gastric emptying, binds water, and can be partially fermented by gut bacteria. As a result, you may feel gas, bloating, or fullness the first week. Thankfully, simple tactics go a long way:
- Start with half a serving (or the smallest capsule count on your label).
- Drink a full glass (~240 mL) of water with every dose — without exception.
- Increase the dose gradually, every few days, only as tolerated.
While you adjust, everyday menu choices can keep you comfortable. For quick, food-level relief, browse our roundup of foods that help you debloat; when gas lingers, meal ideas from what to eat when bloated with gas can make a difference without forcing you into an extreme diet. For a trustworthy clinic perspective on fiber, bloating, and practical pacing, Cleveland Clinic’s plain-English primer on fiber basics is worth a skim.
Stomach cramps or general discomfort
Occasional cramping usually means “too much, too fast,” or not enough fluid. Consequently, cut the dose by half and split it into two smaller servings. Taking psyllium with meals rather than on an empty stomach also softens the impact for sensitive guts. If discomfort persists beyond a week despite these steps, pause, reassess, and consider whether your routine or form (powder vs. capsules) needs a tweak.
Constipation — or the opposite as Metamucil Side Effects
It sounds contradictory, yet both can happen early on. With inadequate water, psyllium’s gel can over-firm stools and slow transit; conversely, starting at a high dose when your gut is touchy may loosen stools temporarily. Therefore, aim for the middle: a modest dose, consistent hydration, and patience. For day-to-day self-care pointers — from fluids to fiber — MedlinePlus’ quick guide to constipation self-care keeps it simple and sensible.
Less common but important risks & Side Effects of Metamucil
Although uncommon, a few risks deserve your full attention. First and foremost, never take psyllium “dry.” Mix powder thoroughly and drink promptly; if you prefer capsules, take one at a time with a full glass of water. Individuals with swallowing difficulties or known esophageal narrowing should speak with a clinician before starting. Stop immediately and seek urgent care for chest pain, vomiting, trouble swallowing, or breathing after a dose — those are not typical adaptation effects. For the exact wording, the product entry on DailyMed is crystal clear.
True allergic reactions can occur, though they’re rare. Hives, rash, facial swelling, wheeze, or sudden breathing trouble require immediate evaluation. When in doubt, stop the product and call your clinician.
How to start — so small issues stay small
Because many metamucil side effects are dose- and hydration-dependent, your first week matters most. A conservative ramp prevents nearly all avoidable discomfort:
- Pick one form (powder, capsules, or gummies) and keep it consistent the first week.
- Start low — for powder, half a serving once daily; for capsules, the smallest labeled count.
- Hydrate every serving with a full glass of water.
- Hold the dose for 3–4 days; if you feel fine, increase slightly; if you feel gassy or crampy, step back for several days and try again.
- Pair with meals (or at least avoid taking it right before lying down).
If you’re still deciding between morning, with-meal, or evening routines, our practical breakdown on when to take Metamucil compares the pros and cons so you can settle on a schedule you’ll actually keep.
Powder vs. capsules vs. gummies
- Powders offer maximum flexibility. You can fine-tune dose and fluid, which often translates to fewer surprises.
- Capsules win on portability, yet they still demand a full glass of water; take them slowly, one at a time.
- Gummies can be palatable, but check for added sugars or sugar alcohols, which can amplify gas for some people.
If you switch forms for tolerance reasons, change one variable at a time and give your gut a few days to adapt before you judge the result.
Gentle add-ons while you adjust
Hydration helps; so do calm, warm beverages. If you’re looking for non-caffeinated options that go down easily, explore our list of teas for digestion, bloating, and gut health and experiment with what actually soothes you.
Long-term use, IBS, and regularity — what evidence says
Once you’re past week one, the bigger question appears: Can you take Metamucil long-term? In practice, yes — long-term use is common in clinical trials and everyday life, provided you tolerate the product, keep your fluids up, and space it from medications if your clinician advises. For IBS, professional guidance consistently favors soluble fiber — notably psyllium — to improve global symptoms for many patients. You can read the formal recommendation in the ACG IBS guideline, which lays out the evidence clearly.
For chronic constipation outside IBS, fiber is often a sensible first step prior to prescription therapies, assuming no red flags (bleeding, fever, unintended weight loss, severe pain). Naturally, persistent or severe symptoms deserve personalized care rather than indefinite self-titration.
Longer term, you’ll likely do best when you combine a small, sustainable psyllium dose with fiber-forward meals. Build plates around oats, legumes, seeds, fruits, and cooked vegetables; then — if needed — keep a steady psyllium routine to maintain momentum. If psyllium continues to feel gassy even with a slow ramp, many readers find flax seeds for strong digestion a gentle adjunct, especially when mixed into yogurt, smoothies, or oatmeal.
Does Metamucil lower cholesterol?
Yes — and not just theoretically. Soluble fiber from psyllium has a formally authorized health claim in the United States when eaten as part of a diet low in saturated fat and cholesterol. If you enjoy seeing the exact language, it lives in federal regulation at 21 CFR §101.81. Mechanistically, psyllium’s gel binds bile acids; in response, your body pulls cholesterol from circulation to make more bile, gradually nudging LDL downward over weeks to months.
From a lifestyle perspective, the most practical gains come from consistency rather than hero doses. For an accessible, clinic-level explanation — plus examples of soluble-fiber foods to pair with psyllium — the Mayo Clinic’s overview on cholesterol and fiber is a clear starting point.
Timing: morning, with meals… or before bed?
There’s no single “best” clock time. Instead, consistency and hydration matter more than the hour. Many people prefer dosing near meals since it’s easier to drink a full glass of water and to remember the routine. Others like mornings for momentum. Bedtime can work if you tolerate it and you don’t take it immediately before lying down. Because the label highlights a choking risk, a brief buffer is wise if reflux or swallowing issues are on your radar. If you’re still undecided, our practical comparison of when to take Metamucil helps you choose a pattern you’ll genuinely keep.
Interactions and other gotchas
Because psyllium forms a gel, it can slow the absorption of certain oral medications if taken at the same time. To minimize that, space fiber and meds by a couple of hours if your clinician or pharmacist recommends it. Additionally, if you track carbohydrates closely for diabetes management, review labels for added sugars — especially in flavored powders and some gummies.
If you’ve had bowel obstruction, esophageal narrowing, or specific gastrointestinal surgeries, get personalized guidance first. In such cases, one-size-fits-all rules don’t apply.
Real-world troubleshooting: making psyllium easier to live with
Because many metamucil side effects cluster in week one, a few small adjustments deliver outsized benefits:
- Mix thoroughly and drink promptly so the gel doesn’t set up in the glass.
- Split the dose; two smaller servings are often gentler than one large one.
- Take with meals if empty-stomach dosing feels rough.
- Hydrate between servings, not only at dosing time.
- Give it a week; most gas and bloating subside as your gut adapts. If not, reduce to the last comfortable dose for several days and inch up again.
- Lean on food while you adjust: simple, repeatable meals help. For inspiration, try these high-fiber sandwich ideas for constipation relief and build from there.
If you enjoy structure, anchor a modest psyllium dose to breakfast or lunch and keep evenings simpler. Alternatively, if afternoons are your snacking danger zone, a mid-meal window may reduce grazing while still keeping hydration easy.
When to stop and call a clinician
Yes, most early effects are mild. Nevertheless, stop and seek medical care if you notice any of the following:
- Chest pain, trouble swallowing, or breathing issues after a dose
- Severe or persistent abdominal pain
- Prolonged constipation or diarrhea despite dose adjustments
- Allergic reactions — rash, facial swelling, wheeze, or hives
- Blood in stool, black tarry stools, fever, or unintended weight loss
For precise, official reminders on warning signs, revisit the product page on DailyMed (Metamucil psyllium label). For concise, self-care-oriented advice, keep MedlinePlus: Psyllium & constipation self-care handy.
Metamucil side effects vs. benefits: the bottom line
At its best, psyllium is a steady, durable tool: not flashy, yet reliably effective when paired with a few smart habits. Mix it well, drink a full glass of water each time, and ramp slowly. Choose a form that fits your routine and listen to your body’s feedback. If your gut wants extra grace during the transition, make simple choices that support it — warm beverages, gentle meals, and a little patience. On balance, these small decisions determine whether your fiber supplement becomes a long-term ally.
Finally, if you’d like the “how-to” details side-by-side, circle back to our practical guide on when to take Metamucil. And if you’d rather understand the ingredient from every angle — uses, benefits, and potential downsides — our overview of psyllium husk side effects fills in the gaps. For readers actively troubleshooting bloat, our list of foods that help you debloat makes an ideal companion while your gut adapts.
FAQs
1) Is it safe to take Metamucil every day?
Generally yes—when used as directed with enough water. Importantly, start low, increase gradually, and watch how your body responds. If unusual symptoms persist or worsen, pause and speak with a clinician. On balance, most adults tolerate daily psyllium well.
2) What are the most common Metamucil side effects?
Most people report gas, bloating, mild stomach cramps, or changes in stool form during the first week. Moreover, these effects usually fade as your gut adapts, especially if you hydrate properly and titrate the dose slowly.
3) Does Metamucil cause gas and bloating?
At first, it can. Psyllium ferments slowly and forms a gel, which may produce gas and a “full” feeling. Furthermore, splitting the dose, taking it with meals, and increasing gradually typically reduces bloating within several days.
4) Can Metamucil make you constipated?
It might if you take too much too soon or drink too little water. Consequently, lower the dose, add fluids, and give your system time to adjust. If constipation persists, reconsider timing or total daily intake.
5) Does Metamucil cause diarrhea or loose stools?
Occasionally, yes—especially with a rapid dose jump. Conversely, easing back to a smaller serving and pairing it with food often restores balance. If loose stools continue, reassess dose and frequency.
6) Why do I get stomach pain or cramps after taking it?
Often it’s a sign of fast titration or inadequate hydration. Specifically, reduce the serving size by half, take it with a meal, and evaluate again after a few days. If pain is severe or persistent, discontinue and seek guidance.
7) Will Metamucil make me poop more—or just more regularly?
In practice, psyllium normalizes stool form—softening hard stools and firming loose ones—so bathroom trips may become more predictable rather than simply more frequent. Nevertheless, early adjustments can feel irregular for a short time.
8) Is it okay to use Metamucil before bed?
Yes—provided you tolerate it and drink a full glass of water with your serving. Nevertheless, avoid taking it immediately before lying down, particularly if you have reflux or swallowing issues, to minimize discomfort.
9) Does Metamucil help with bloating long term?
Often it does. Initially, bloating can rise; over time, many users notice less straining and steadier digestion. Additionally, steady hydration and a measured dose ramp are key to long-term comfort.
10) Can Metamucil cause heartburn?
Sometimes large or rushed servings—especially right before lying down—can aggravate reflux. Accordingly, try smaller amounts, take it earlier, and sip water unhurriedly. If heartburn persists, adjust timing or discuss alternatives.
11) Can I take Metamucil every day for months or years?
As a rule, long-term use is common when tolerated, with appropriate fluids and reasonable dosing. Importantly, if your symptoms change, review the plan with a healthcare professional to personalize it.
12) What is the best time to take it—morning, with meals, or evening?
Consistency matters more than the clock. For example, many prefer with meals because it’s easier to remember and to drink a full glass of water. Still, choose the time you’ll sustain comfortably.
13) Capsules vs powder vs gummies—do side effects differ?
Powder allows finer dose control and typically pairs with more water, which may feel gentler. Meanwhile, capsules are convenient but still need a full glass of water. Gummies can include sugars or sugar alcohols that, for some, increase gas.
14) Can Metamucil cause dehydration?
Indirectly, yes—if you skimp on fluids. Because psyllium holds water in the stool, insufficient intake can make stools harder. Therefore, drink a full glass with each serving and maintain overall hydration through the day.
15) Does Metamucil lower cholesterol?
Yes, modestly, as part of a diet low in saturated fat. Notably, soluble fiber from psyllium can help reduce LDL over weeks when used consistently. Results vary with dose, diet quality, and adherence.
16) Can Metamucil lead to weight gain or water retention?
Unlikely. In fact, some people feel fuller and may snack less. That said, early bloating can feel like “puffiness.” Additionally, flavored products with added sugars contribute calories—check labels if that’s a concern.
17) Why do I feel more gassy than usual even after a week?
Sometimes the dose is still a bit high for your gut pace, or your meal pattern is overly fermentable at the same time. Accordingly, step down slightly, split the dose, and reassess after several days.
18) How long do the early Metamucil side effects last?
Typically a few days to about a week. Beyond that, most users settle. Importantly, persistent or severe symptoms are a signal to pause, reduce the dose, or consult a clinician.
19) Can I take Metamucil with other medications?
Psyllium’s gel can slow absorption when taken simultaneously. Therefore, many people separate fiber and oral meds by a couple of hours. For safety, follow your prescriber’s specific advice.
20) Who should not take Metamucil?
People with swallowing difficulties, known GI strictures, or a history of obstruction should seek medical guidance first. Likewise, anyone with severe or unexplained GI symptoms should get evaluated before starting.
21) What happens if I take too much Metamucil at once?
You may experience pronounced gas, cramping, or stool changes. Consequently, stop, hydrate, and restart later at a lower dose. If severe symptoms occur, discontinue and get professional advice.
22) Do Metamucil side effects differ if I take it on an empty stomach?
They can. Some find empty-stomach dosing intensifies bloating or cramping. Accordingly, try taking it with meals or a snack, and adjust based on comfort.
23) Can Metamucil trigger allergic reactions?
Rarely, yes. Signs include rash, hives, swelling, wheeze, or trouble breathing. In such cases, stop immediately and seek medical care. Beyond that, avoid re-exposure until you’ve been evaluated.
24) Does Metamucil help IBS or make it worse?
Often helpful. Specifically, soluble fiber like psyllium may improve overall IBS symptoms over time. Still, ramp slowly, observe your response, and tailor the dose to tolerance.
25) What’s the quickest way to reduce gas from Metamucil?
First, cut the dose by half. Next, split it into two or three smaller servings. Additionally, take it with meals, sip a full glass of water each time, and give your gut several days to adapt.
26) Can Metamucil cause stomach pain days after stopping?
Uncommonly, yes—usually related to other factors (diet shifts, low fluids, stress). In brief, resume balanced hydration and gentle meals; if pain persists, get it checked.
27) Will Metamucil make me poop immediately?
Not typically. Instead, expect steadier stool form over several days. Gradual consistency improvements are normal; sudden urgency suggests the dose may be high for your current tolerance.
28) Can I use Metamucil during intermittent fasting?
Many prefer to take it during eating windows to pair it with water and reduce GI sensations. Nevertheless, if you take it while fasting, monitor how your gut feels and adjust accordingly.
29) Why does my bloating feel worse at night?
Sometimes timing plus meal composition stacks fermentation later in the day. Therefore, consider shifting part of the dose earlier, reducing large late meals, and maintaining steady fluids.
30) What’s the bottom line on metamucil side effects?
In summary, mild gas, bloating, or cramps can occur—mostly in week one—and usually ease with hydration, smaller servings, and patience. More serious red flags (chest pain, trouble swallowing, breathing issues, severe pain, or allergic signs) require stopping and seeking care.
Further reading & sources on Side Effects of Metamucil
- Product labeling and warnings: Metamucil psyllium label on DailyMed
- Patient overview: MedlinePlus — constipation self-care (includes psyllium)
- IBS guideline recommending soluble fiber: ACG Clinical Guideline (IBS)
- Clinic explainer on fiber & bloating tips: Cleveland Clinic — Fiber basics
- Authorized health claim language: 21 CFR §101.81 (soluble fiber/psyllium & heart disease risk)
- Dietary fiber & LDL explained: Mayo Clinic — Cholesterol and fiber