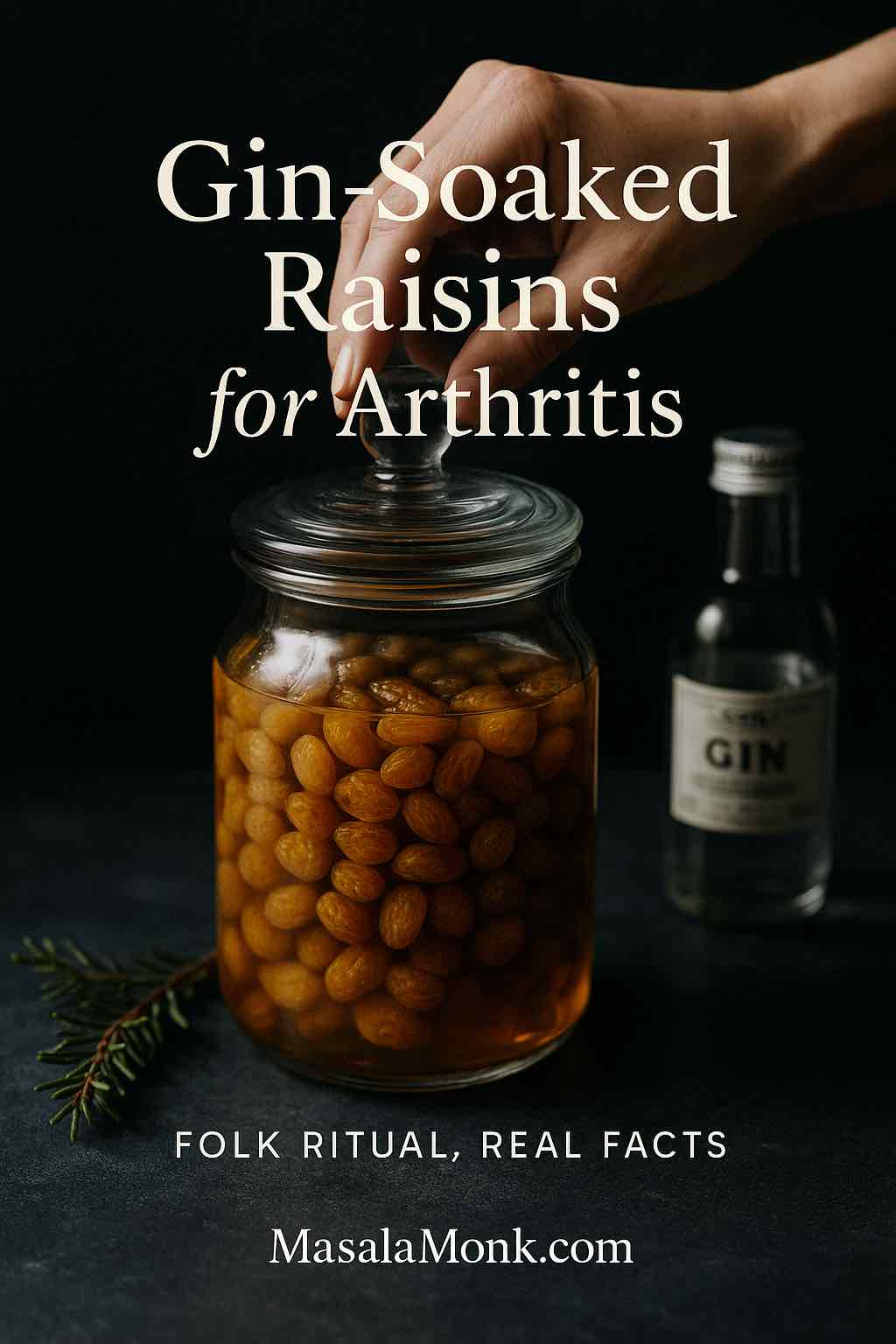
Many readers come to this topic with a simple question and a hopeful heart. Gin-Soaked Raisins for Arthritis sound like something a wise grandparent might pass down: a small jar on the kitchen shelf, a handful of golden fruit, a splash of gin, and a calm daily ritual. The story is warm and memorable. Nevertheless, tradition is one thing; dependable relief is another. This article respects the charm of the practice, explains how to prepare a jar properly, clarifies what evidence does—and does not—support it, and offers practical, evidence-based ways to care for your joints alongside any personal rituals you keep.
Also Read: What are the 5 Worst Foods to Eat if you have Arthritis?
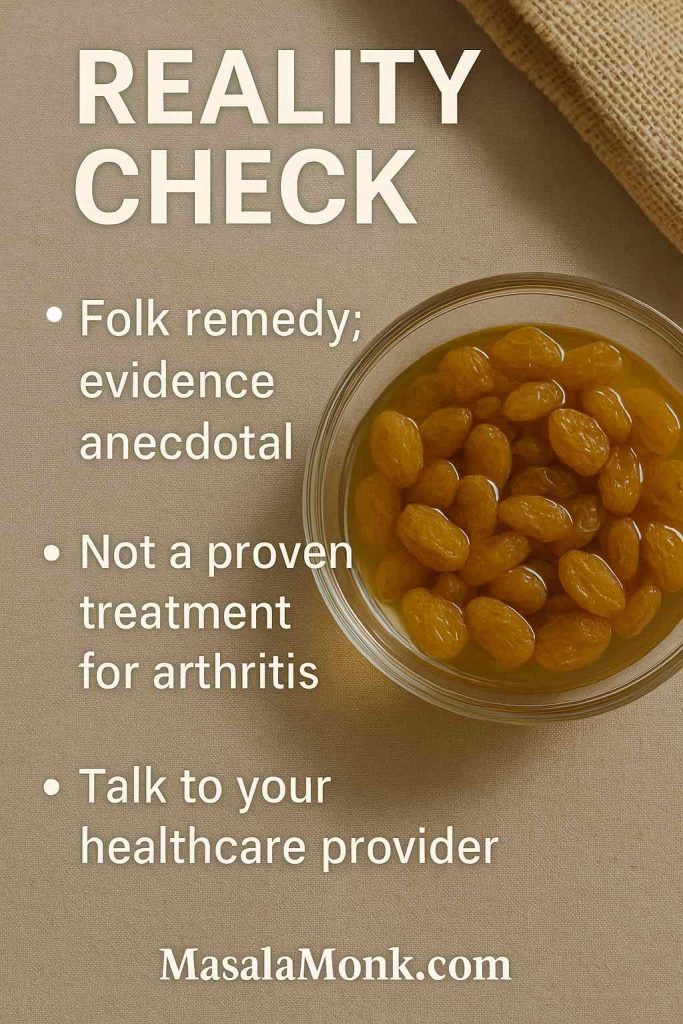
What Makes Gin-Soaked Raisins for Arthritis a Folk Ritual
Stories like this survive because they feel human. They are tactile, flavorful, and easy to remember. You cover golden raisins with gin, you wait, and you eat a modest portion every day. Some people report comfort. Others simply enjoy the taste and the habit. Even so, authoritative sources describe the remedy as unproven. The Arthritis Foundation: 10 arthritis food myths groups gin-soaked raisins with other popular ideas that lack clinical backing. Independent overviews reach similar conclusions; see Healthline’s review of gin-soaked raisins and Medical News Today on gin-soaked raisins for balanced summaries.

Even so, the appeal is understandable. First, the ritual itself can feel soothing. Second, laboratory work on juniper—the botanical that defines gin—has noted anti-inflammatory signals in models. Interesting, yes. Conclusive for daily life, no. Consequently, Gin-Soaked Raisins for Arthritis should be seen as culture, not cure. With that frame in mind, you can still make a tidy batch, enjoy it safely, and keep expectations realistic.
Also Read: Probiotics and Gut Health: Their Role in Reducing Inflammation
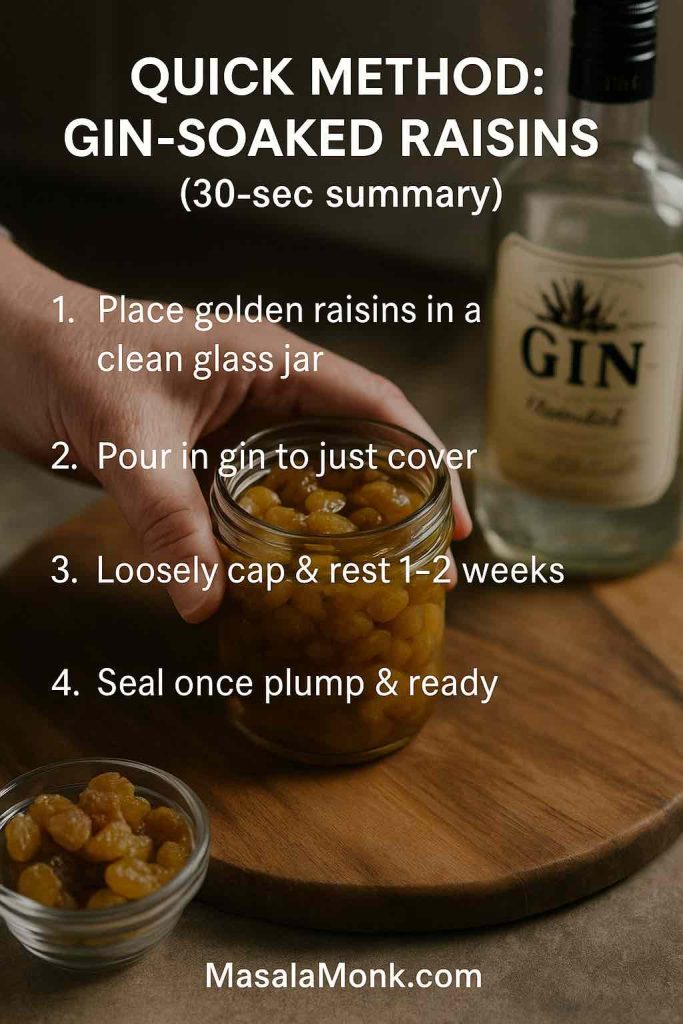
Preparing Gin-Soaked Raisins for Arthritis: A Calm, Step-by-Step Method
You’ll need
- 1 cup golden raisins (often labeled yellow or white raisins; also called sultanas)
- Enough gin to just cover the fruit (a juniper-forward London Dry works well)
- A clean glass jar with a lid
Method
- Add the fruit. Tip the golden raisins into a clean, dry glass jar.
- Pour the gin. Add just enough gin to barely submerge the raisins. Avoid a deep pool; a light cover is ideal.
- Let them rest. Cover loosely and place the jar out of direct sunlight at room temperature. Leave it for 1–2 weeks. Stir every few days so surface alcohol dissipates evenly while the raisins plump.
- Seal the jar. Once the aroma softens and the fruit looks full, seal the lid.
- Use modestly. The folk pattern suggests about 7–10 raisins per day with food. That number comes from tradition rather than science, so treat it as a guideline, not a dose.
This gentle pace suits most home kitchens. If you prefer to test the practice without committing to a large amount, halve or quarter the ingredients and keep the same steps. Meanwhile, resist the urge to rush evaporation with heat or sun; gentler conditions keep flavor more balanced and reduce risk.
Also Read: What Is Inflammation? Body’s Double-Edged Sword
Choosing Fruit: Golden, Yellow, “White,” or Dark Raisins?
Supermarket labels can be confusing. “Golden,” “yellow,” and sometimes “white” all refer to sultanas, which are processed a bit differently from classic dark raisins. They are typically treated with sulfur dioxide to preserve their lighter color and a soft, fruit-forward character. For a clear, kitchen-friendly explainer, see Martha Stewart: golden vs. regular raisins. By contrast, dark raisins are usually sun-dried, which deepens color and intensifies a toffee-like note. You can use either style for Gin-Soaked Raisins for Arthritis; however, the classic version favors golden raisins because the texture plumps attractively and the flavor stays bright.

If you enjoy exploring dried-fruit nutrition more broadly, these two deep dives move away from pain claims and back toward everyday health: black raisins (munakka) benefits and soaked black raisins benefits.
Picking a Spirit: Which Gin Style Works Best?
Here the rule is simple. Choose a juniper-forward London Dry. That style brings a clean pine-citrus profile that pairs well with the raisin’s honeyed sweetness. The brand is your call. Use something you’d happily drink in a gin and tonic. The goal is flavor, not pharmacology, so there’s no need to chase rare bottles.
Storing Gin-Soaked Raisins for Arthritis Safely and Sensibly
Once the fruit has plumped and the jar is sealed, storage matters. Keep the jar cool, dark, and dry. In temperate weather, a pantry cupboard is fine. In hot or humid conditions, shift the jar to the refrigerator. These habits echo established guidelines for shelf-stable foods; for reference values used in institutional settings, consult USDA FNS dry-storage guidance.
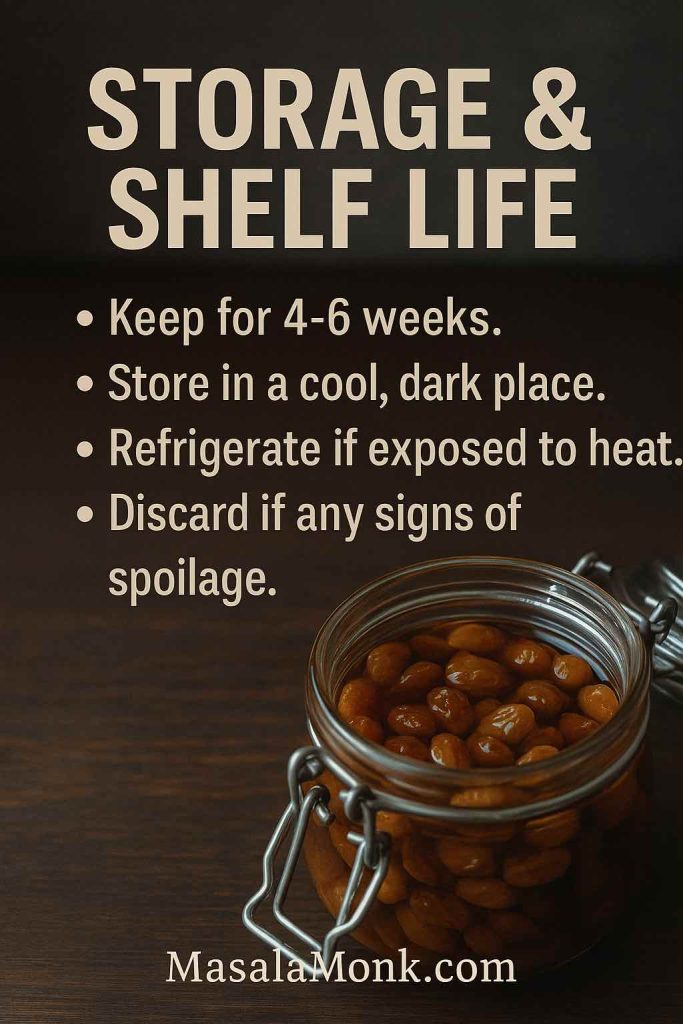
How long should a homemade batch last? As a home project, it will never have the controls of a commercial product, so plan to enjoy it within about 4–6 weeks. Industry standards for raisin moisture help explain why drier fruit stores better; if you’re curious about the background, read USDA raisin grades & moisture limits. If the jar ever fizzes, smells off, or shows visible mold, discard it without tasting. Conversely, if the fruit gradually dries out, add a splash of gin, close the lid, and let it rest for 24 hours before eating.
Also Read: Cherries and Arthritis: Are Cherries Good for Arthritis?
How Evidence Frames Gin-Soaked Raisins for Arthritis
Good decisions start with clear information. Major organizations do not recommend Gin-Soaked Raisins for Arthritis as treatment. The Arthritis Foundation: 10 arthritis food myths explains the lack of clinical support in plain language. Independent editors echo this view in Healthline’s review of gin-soaked raisins and Medical News Today on gin-soaked raisins, noting that controlled trials are missing and that anecdotal reports cannot confirm cause and effect.
So what about the chemistry? Juniper contains compounds with anti-inflammatory activity in lab and animal models. That remains interesting academic work, yet it does not prove that raisins briefly soaked in gin will reduce joint pain in daily life. Accordingly, the remedy can be appreciated as a culinary custom, while clinical care continues on sturdier ground.
Potential Upsides Without Over-Promising
Let’s be fair. Gin-Soaked Raisins for Arthritis offer a few gentle positives unrelated to cure claims. The ritual is simple. The flavor can be delightful. A small, predictable habit sometimes supports consistency with other good choices: regular walks, light mobility exercises, and steadier meal patterns. Moreover, a friendly kitchen project can reduce anxiety around health changes by giving the day a small anchor. These are meaningful lifestyle benefits, even though they are not the same as pain relief.
That distinction matters. It keeps the joy of the jar and the strength of a medical plan in healthy balance.
Side Effects and Who Should Avoid Gin-Soaked Raisins for Arthritis
Because the method merges dried fruit and alcohol, a few cautions are essential.
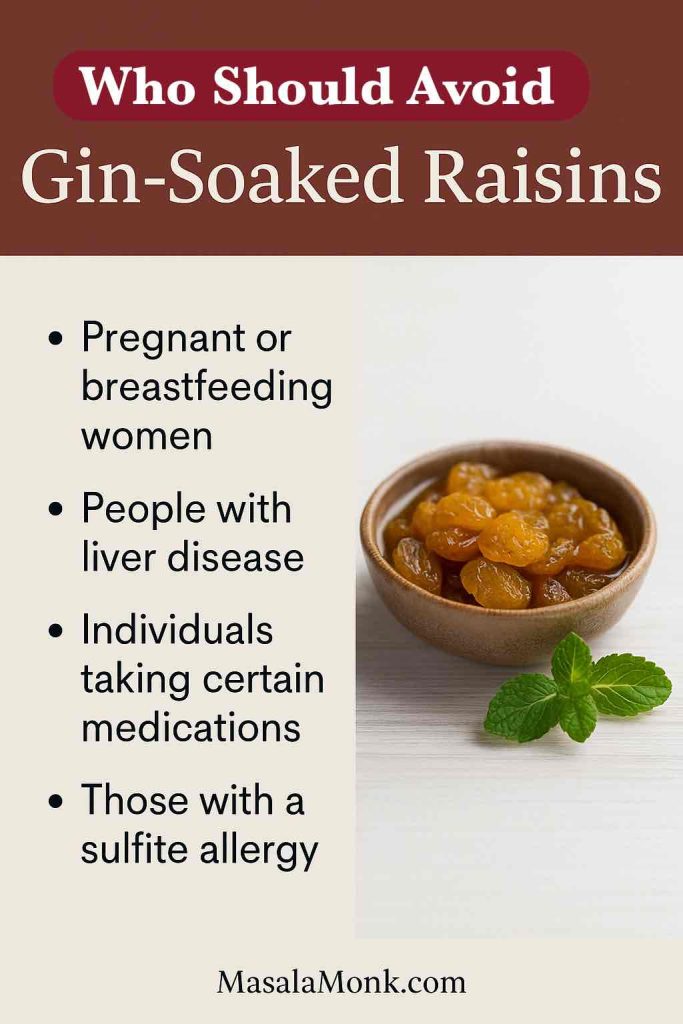
- Alcohol exposure. Even after resting, traces of alcohol can remain. Avoid this preparation if you are pregnant, in alcohol recovery, on certain medications, or if alcohol is otherwise contraindicated for your health.
- Sugar load. Raisins are naturally high in sugar. If you live with diabetes or track carbohydrates, count the raisins and monitor your response.
- Sulfites. Golden raisins often list sulfur dioxide on their labels. Ingredient lines vary by brand, but a common example is shown here: Sun-Maid golden raisins ingredients. If you have sulfite sensitivity or certain forms of asthma, this matters.
- Juniper caution (theoretical). Concentrated juniper preparations raise questions in some herbal contexts; your kitchen jar is a very different exposure, yet sensitivity varies. When uncertain, skip the remedy and seek professional guidance.
If you’re evaluating other widely shared ideas about food and joint pain, these explainers help separate custom from consensus: apple cider vinegar for arthritis & joint pain and tomatoes and arthritis: the truth.
Building a Stronger Everyday Plan Around Your Joints
Rituals can live beside robust care, but they shouldn’t replace it. In practice, a durable plan tends to rest on four pillars:
Movement you can maintain. Gentle activity decreases stiffness, protects function, and lifts mood. Short, regular sessions beat rare, heroic efforts.
Medication as prescribed. From anti-inflammatories to DMARDs and biologics, work with your clinician to find the right regimen. Adjustments take time, and steady follow-up matters.
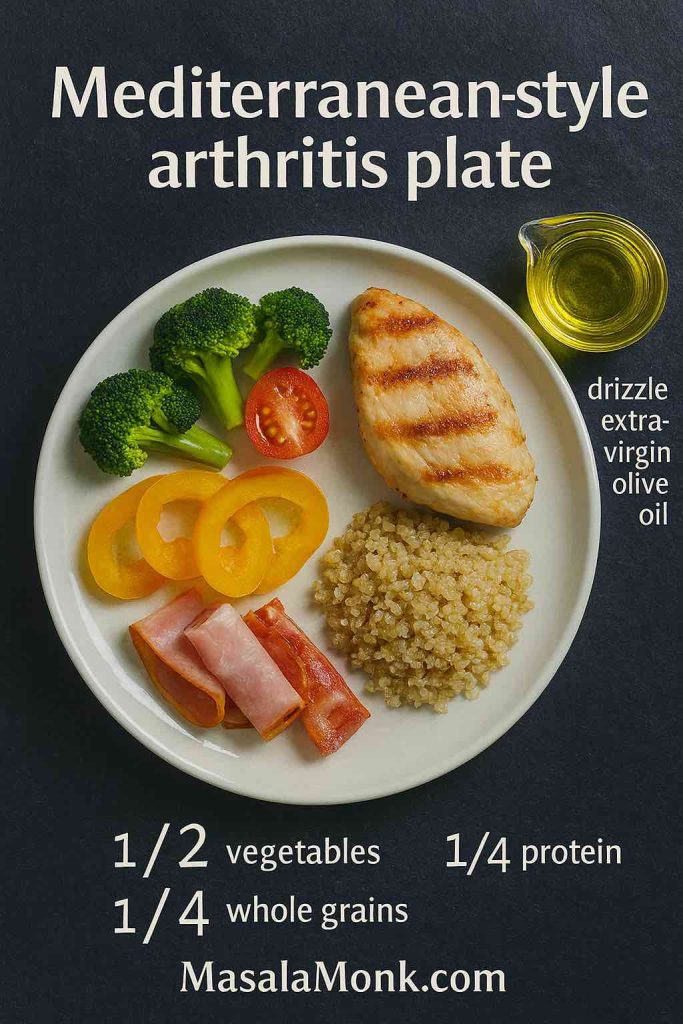
Nutrition with a long view. Favor whole foods, adequate protein, and sources of healthy fats—especially omega-3s. For accessible guidance, start with how omega-3 fatty acids help fight chronic inflammation and build menus with unpacking the health benefits of oily fish. If you prefer a stepwise approach, how to follow an anti-inflammatory diet lays out simple swaps.
Recovery habits. Sleep and stress skills amplify everything else. A regular wind-down routine, a brief stretch, or a warm shower can nudge the nervous system toward calm. If you enjoy a soothing mug in the evening, turmeric-ginger-cinnamon tea benefits offers a kitchen-friendly option with a pleasant, cozy flavor.
With these anchors in place, Gin-Soaked Raisins for Arthritis can remain what they are: a small cultural practice, folded into a wider, evidence-based rhythm.
Also Read: Best Fish Oil Supplements on Amazon India
When Curiosity Meets Caution: A Practical Way to Try the Jar
If you remain curious, approach the project as a mindful tasting rather than a treatment. Make a half batch. Store it correctly. Eat a few raisins with a meal. Notice how you feel over several weeks while keeping your regular care unchanged. If you observe no benefit, thank the jar for the experiment and move on without regret. If you enjoy the flavor and the ritual, you can keep a small jar in the pantry or the refrigerator and treat it like any other homemade preserve you rotate now and again.
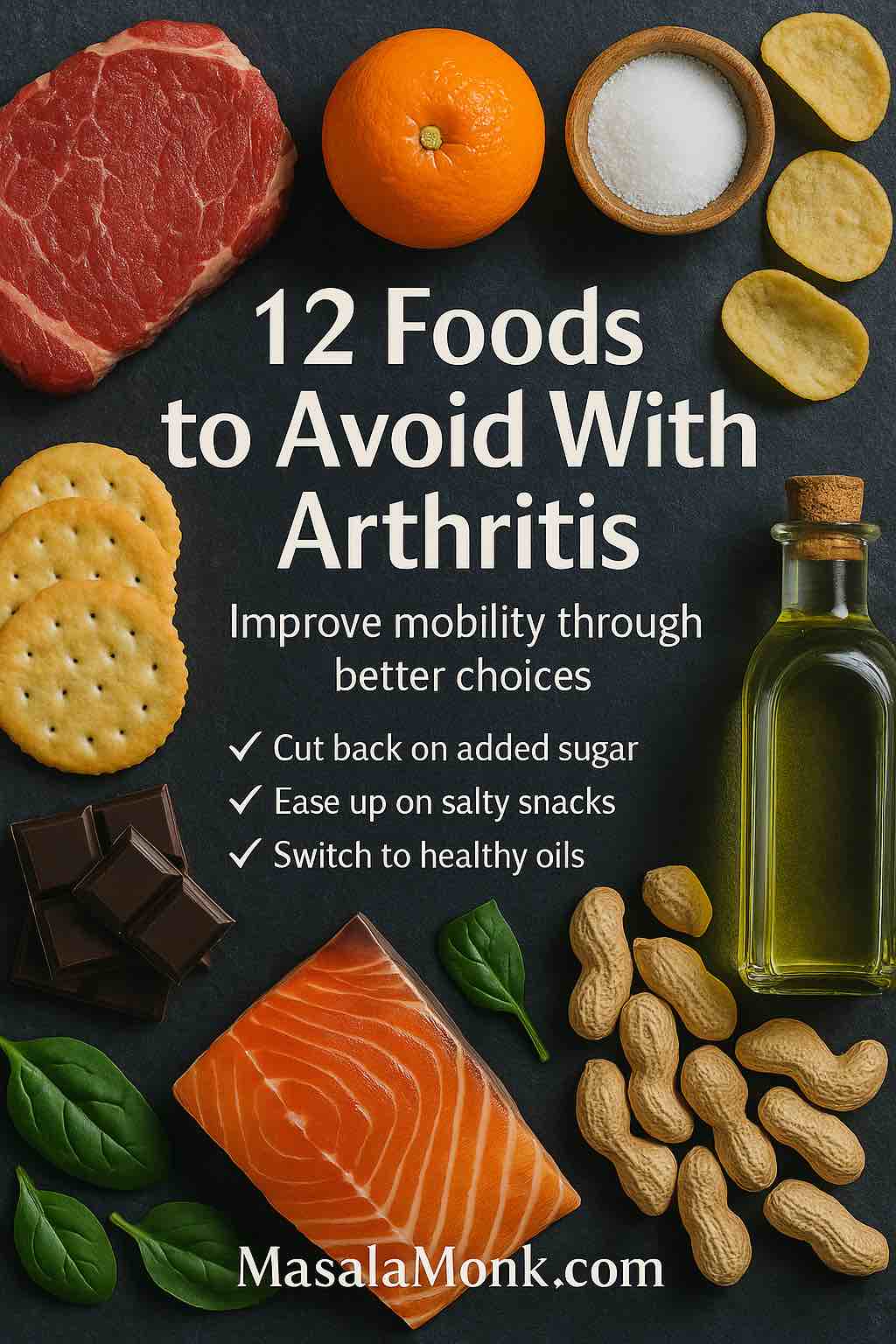
For a broader perspective on dietary patterns that may aggravate symptoms, explore foods to avoid with arthritis. It’s practical, not preachy, and it pairs well with the gradual upgrades suggested in how to follow an anti-inflammatory diet.
Closing Thought: Keep the Warmth, Protect the Future
Kitchens carry memories. A grandparent’s jar of Gin-Soaked Raisins for Arthritis may stand beside pickles, preserves, and spice blends that define a family table. Honor that history. At the same time, protect your future comfort with habits that have stood up to careful scrutiny. Move often. Eat in a way that calms inflammation over many months, not just one. Sleep enough to heal. Work with your clinician the way you’d maintain a garden—patiently, consistently, and with a willingness to adjust.
If you want one small action today, plan two fish meals this week using ideas from unpacking the health benefits of oily fish. Or remove a common trigger using foods to avoid with arthritis. If a gentle evening drink helps you unwind, brew a mug guided by turmeric-ginger-cinnamon tea benefits. Then, if curiosity still calls, prepare a small jar of Gin-Soaked Raisins for Arthritis, store it well, and enjoy it for what it is: a pleasant ritual living peacefully beside proven care.
FAQs
1) What exactly are Gin-Soaked Raisins for Arthritis?
They’re simply golden raisins covered with a small amount of gin, left to rest until plump, and then eaten in tiny daily portions. It’s a long-standing kitchen tradition—more about comfort and ritual than clinical treatment.
2) Do Gin-Soaked Raisins for Arthritis actually help with joint pain?
Evidence is mostly anecdotal. Some people feel better; others notice no change. In practice, treat the jar as a gentle ritual you may enjoy, not as a replacement for medical care.
3) How do I make a reliable first batch?
For starters, place golden raisins in a clean glass jar and pour in just enough gin to barely cover them. Loosely cap the jar and rest it at room temperature, away from sunlight, for 1–2 weeks. When the aroma softens and the raisins look plump, seal the jar.
4) How many should I eat per day?
As a rule, people take 7–10 raisins daily with food. Begin on the low end, notice how you feel, and adjust—or stop—accordingly.
5) How long should the raisins soak in gin?
Typically 1–2 weeks. Meanwhile, stir every few days so surface alcohol disperses and the texture evens out. Seal once they’re pleasantly plump.
6) What kind of gin works best?
Choose a juniper-forward London Dry style. It keeps the flavor bright and classic. Brand matters less than that clean, pine-citrus character.
7) Must I use golden raisins, or can I swap in dark ones?
Golden raisins (often called sultanas) are traditional because they plump softly and taste light. That said, dark raisins will work; the flavor will simply be deeper and the bite chewier.
8) Are “golden,” “yellow,” and “white” raisins different for this method?
They’re usually names for the same style of sultana. Labels vary, yet the preparation—cover, rest, and seal—stays the same for Gin-Soaked Raisins for Arthritis.
9) What’s the serving routine that people follow?
Many eat a small portion once daily, often in the morning with breakfast or in the evening with a snack. Consistency matters more than the exact time.
10) How long do Gin-Soaked Raisins for Arthritis keep?
In most home kitchens, plan on 4–6 weeks. Keep the jar sealed, cool, and dark. In warm or humid weather, refrigeration is the safer choice.
11) How do I store them to avoid waste?
After sealing, place the jar in a cool cupboard; if the room feels hot or damp, move it to the fridge. Always use a clean spoon and close the lid promptly.
12) What are the signs I should throw the batch away?
If you notice fizzing, an off smell, or any visible mold, discard immediately. When in doubt, it’s better to be cautious.
13) Can I revive raisins that seem dry after a few weeks?
Yes. Add a small splash of gin, reseal the jar, and let it rest for about 24 hours. Then reassess the texture before eating.
14) Are there side effects I should consider?
Possibly. Even after resting, trace alcohol may remain. Raisins are naturally high in sugar, and golden raisins often contain sulfites. If you’re sensitive to alcohol, sugar, or sulfites, proceed carefully—or skip the practice.
15) Who should avoid Gin-Soaked Raisins for Arthritis altogether?
Anyone who is pregnant, in alcohol recovery, advised to avoid alcohol, or sensitive to sulfites should avoid them. Likewise, if you have concerns about interactions or conditions, talk with your clinician first.
16) Can this ritual replace my current arthritis treatment?
No. Gin-Soaked Raisins for Arthritis are a cultural custom. Keep following your prescribed plan, and view the jar—if you use it—as an optional add-on for enjoyment only.
17) How can I try them without overcommitting?
Make a half or quarter batch. Taste a few raisins with a meal for a couple of weeks. If you enjoy the ritual and feel fine, continue; otherwise, let it go without regret.
18) What if I want the flavor but less sugar?
Keep portions small, pair your raisins with protein or fiber (like yogurt or nuts), and track how your body responds. Conversely, if sugar is a major concern, it’s reasonable to skip the jar.
19) Why do some people swear by Gin-Soaked Raisins for Arthritis?
Ritual itself can be soothing. Moreover, the flavor is pleasant, the routine is simple, and feeling in control helps. Still, personal stories aren’t the same as proof, so keep expectations modest.
20) Any last guidance for a calm, sensible approach?
Start small. Store carefully. Pay attention to how you feel. Most importantly, keep Gin-Soaked Raisins for Arthritis in their lane—as a warm, easy ritual that can live alongside, not instead of, the treatments that truly support your long-term comfort.
Further Reading (References and Sources)
- Arthritis Foundation: 10 arthritis food myths — Start here to see how leading clinicians frame popular nutrition claims, including gin-soaked raisins, with plain-language explanations and practical takeaways.
- Healthline’s review of gin-soaked raisins — Next, examine a concise, medically reviewed overview that summarizes what’s known (and unknown), plus common questions people ask before trying the remedy.
- Medical News Today on gin-soaked raisins — Then, scan a balanced breakdown of anecdotal reports versus clinical evidence, along with safety notes and alternatives you can discuss with your clinician.
- Martha Stewart: golden vs. regular raisins — Afterward, dig into a clear kitchen explainer on how golden (sultana) raisins differ from dark raisins—processing, texture, and flavor—so your jar turns out as expected.
- USDA FNS dry-storage guidance — Meanwhile, ground your storage routine in official recommendations for cool, dry conditions, with handy temperature ranges and moisture tips for pantry items.
- USDA raisin grades & moisture limits — When you want context for shelf life, this standard outlines how moisture and quality are defined in the trade—useful background for judging homemade batches.
- Sun-Maid golden raisins ingredients — To verify sulfites in real labels, glance at a typical ingredient list so you know what “sulfur dioxide” looks like on packaging if sensitivity is a concern.
Related Reading on MasalaMonk
- Foods to avoid with arthritis — Begin with a practical list of common triggers and easy swaps; each item comes with plain reasoning so you can change your plate without guesswork.
- Apple cider vinegar for arthritis & joint pain: myths vs facts — Next up, sort folklore from evidence on another much-loved kitchen remedy, including what helps, what doesn’t, and how to stay safe.
- How omega-3 fatty acids help fight chronic inflammation — Then, explore why omega-3s matter for joint comfort, how much to aim for, and simple ways to hit your targets with real food.
- Unpacking the health benefits of oily fish — After that, get menu ideas, preparation tips, and nutrient highlights so fish nights are both delicious and purposeful.
- How to follow an anti-inflammatory diet — Meanwhile, map out a week of eating with a straightforward framework: pantry staples, shopping cues, and plate-building guidance.
- Turmeric-ginger-cinnamon tea benefits — If you enjoy a warm evening ritual, this piece offers a gentle, aromatic option plus tips for balanced spice blends.
- Wellness shots with turmeric & ginger — For a brighter start to the day, browse quick-shot recipes with measured spice levels and make-ahead notes for busy mornings.
- Black raisins (munakka) benefits — Whenever you want to compare raisin varieties, this guide covers flavor, nutrition, and realistic ways to use them beyond folklore.
- Soaked black raisins benefits — Finally, circle back to everyday nutrition with soaking tips, portion pointers, and serving ideas that fit neatly into a balanced routine.