In a world that never seems to slow down, stress and anxiety have become almost universal companions. Whether you’re juggling deadlines, battling burnout, or just trying to keep up with daily life, you may have heard about Ashwagandha—an ancient herb with a modern-day following.
But does Ashwagandha actually help with anxiety and stress? What does the research say? And what about real people—are they finding relief, or just another wellness trend?
Let’s go beyond the hype. In this comprehensive guide, I’ll break down what Ashwagandha is, the science behind it, the latest research (including what’s new in 2025), user experiences (the good, the bad, and the surprising), and practical advice for anyone considering this supplement.
What Is Ashwagandha?
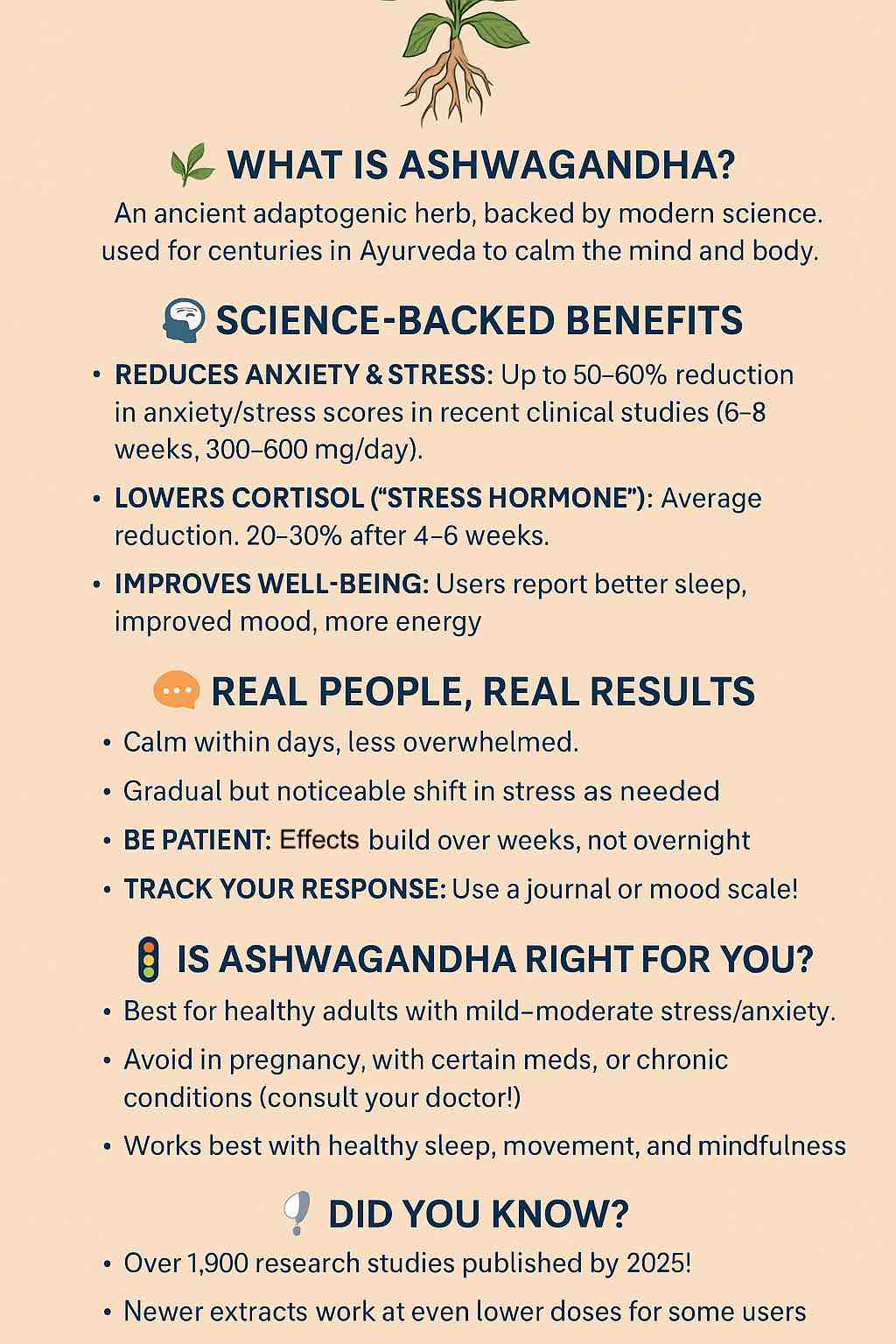
Ashwagandha (Withania somnifera), sometimes called “Indian ginseng” or “winter cherry,” is a shrub native to India and parts of Africa. In Ayurveda, it’s considered a powerful adaptogen—a substance that helps the body manage stress.
The root (and sometimes leaf) is used to make extracts, capsules, powders, and even gummies. You’ll find it in everything from nootropic stacks to bedtime teas. But the key question remains: Does it actually work for stress and anxiety?
The Science: What Do the Latest Studies Say?
Clinical Trials and Meta-Analyses
2025 marks a boom in Ashwagandha research, with over 1,900 studies published worldwide. Recent gold-standard clinical trials and meta-analyses (reviews of many studies) paint a clearer picture than ever:
- Consistent Stress & Anxiety Relief: Multiple randomized controlled trials show Ashwagandha extract—especially in standardized forms like KSM-66, Sensoril, Shoden, or Asvaman®—can reduce anxiety and stress scores by up to 50–60% over 6–8 weeks at doses of 300–600 mg/day.
- Cortisol Reduction: Most studies confirm significant reductions in serum cortisol (the “stress hormone”)—often 20–30% lower than baseline.
- Improvements in Wellbeing: Beyond stress and anxiety, users report better sleep, less fatigue, improved mood, and even mild cognitive boosts.
Key Recent Findings:
| Study / Review | Extract / Dose | Duration | Main Findings |
|---|---|---|---|
| Asvaman® 2025 | 300 mg 2x/day | 6 weeks | ↓Cortisol, ↑physical performance, better mood |
| Meta-analysis 2024 | 250–600 mg/day | 6–8 weeks | ↓Anxiety (HAM-A), ↓Perceived Stress (PSS), ↓Cortisol |
| Shoden Extract 2024 | 60–120 mg/day | 60 days | ↓HAM-A ~59%, ↓Cortisol ~67%, safe and effective |
How Does It Work?
Ashwagandha’s benefits are believed to stem from:
- HPA Axis Modulation: Helping regulate the body’s main stress system, lowering chronically high cortisol.
- GABA-like Activity: Some evidence it boosts calming neurotransmitters.
- Withanolides: Active compounds (especially withanolide glycosides) thought to drive most benefits.
What Real People Are Saying: Unfiltered User Experiences
Reddit, Forums, and Reviews
The Good:
- “It worked instantly … after a week, my anxiety eased significantly.”
- “Big decrease in stress … first week was pure bliss. I feel less overwhelmed.”
The Mixed:
- “I took it for two weeks and felt nothing. Maybe it’s just a trend.”
- “It reduced stress at first, but after a few weeks I felt numb and flat.”
The Cautions:
- “I felt emotionally numb and couldn’t feel happiness—fear and anxiety were gone, but so was joy.”
- Some reported worsened anxiety or panic after starting Ashwagandha.
Editorial test drives (Verywell, Glamour) often echo clinical data: noticeable improvement in stress and sleep after 2–4 weeks, but the effect isn’t always dramatic—and it can fade with continuous use.
Why the Mixed Results?
- Individual response: Genetics, baseline anxiety, other medications, and even gut health can influence how someone reacts.
- Product quality: Cheaper or underdosed products rarely deliver; standardized extracts (KSM-66, Sensoril, Shoden, Asvaman®) are more reliable.
- Dosing: More isn’t always better—some people benefit from as little as 60–120 mg, others need 300–600 mg, and a few experience side effects at any dose.
Safety, Side Effects, and What to Watch For
Short-term Ashwagandha is generally well tolerated:
- Mild side effects: Sleepiness, stomach upset, headache, rarely vivid dreams.
- Rare risks: Liver injury (extremely uncommon but reported), emotional flattening at high doses or long-term use.
DO NOT use if:
- You are pregnant or breastfeeding.
- You have hormone-sensitive conditions, thyroid disorders, or are on sedatives, SSRIs, or immunosuppressants—without consulting your doctor.
Long-term safety (>3 months) is less well studied. Consider cycling or breaks, and always source high-quality, third-party-tested products.
Practical Tips: How to Use Ashwagandha Safely and Effectively
- Choose a reputable extract: Look for KSM-66, Sensoril, Shoden, or Asvaman®—preferably root-only for anxiety.
- Start low, go slow: Begin with 100–300 mg daily, increasing only if needed after 1–2 weeks.
- Be patient: Expect real results in 2–6 weeks, not overnight.
- Track your progress: Use a journal, stress scale, or an app. Monitor for both positive effects and unwanted side effects.
- Cycle if needed: Many users take breaks (e.g., 1 week off every 4–6 weeks) to maintain sensitivity and minimize emotional flattening.
- Combine with lifestyle basics: Ashwagandha works best alongside exercise, sleep hygiene, and mindfulness—not as a substitute.
- Consult a professional: Especially if you’re on medication or have a complex health history.
Final Thoughts: Is Ashwagandha Right for You?
Ashwagandha isn’t a miracle cure, but it’s a promising, well-tolerated option for many people seeking relief from stress and anxiety. The key is to treat it like any other wellness tool—with awareness, moderation, and a dose of healthy skepticism.
If you’re curious, start with a reputable brand, track your experience, and combine it with lifestyle changes for best results. And remember: what works wonders for one person may be a dud for another—listen to your body, and don’t be afraid to experiment (safely).
Sources & Further Reading
- Verywell Health – Ashwagandha for Anxiety
- PubMed – 2024 Meta-Analysis
- Glamour – Real User Story
- Reddit r/Anxiety
- WebMD User Reviews
Have you tried Ashwagandha? Share your experience in the comments below!
Frequently Asked Questions (FAQs)
1. How long does it take for Ashwagandha to start working for anxiety or stress?
Most people notice initial effects within 1–2 weeks, but consistent, significant benefits usually develop after 4–6 weeks of daily use.
2. What’s the best Ashwagandha dosage for anxiety or stress relief?
Most clinical research supports 300–600 mg per day of a high-quality, standardized extract (like KSM-66, Sensoril, or Shoden). Some newer extracts (e.g., Shoden, Asvaman®) may work at lower doses (60–120 mg).
3. Are there any side effects I should watch for?
Ashwagandha is generally well tolerated, but possible side effects include sleepiness, stomach upset, diarrhea, headache, or vivid dreams. Rarely, users report emotional dullness or liver concerns. Discontinue if you experience adverse effects.
4. Can I take Ashwagandha with my prescription medications?
Ashwagandha may interact with medications for anxiety, depression (SSRIs, benzodiazepines), thyroid, blood sugar, or immunosuppression. Always consult your doctor before combining Ashwagandha with prescription drugs.
5. Is Ashwagandha safe for long-term use?
Short-term use (up to 3 months) appears safe for most healthy adults. There’s not enough research to confirm long-term safety, so consider periodic breaks and always monitor for symptoms.
6. Does Ashwagandha work instantly or is it more subtle?
Some people feel calmer within hours, but most experience gradual relief over weeks. Effects are generally subtle and build over time rather than feeling dramatic or “medicinal.”
7. Can Ashwagandha help with sleep?
Many users and studies report better sleep quality, especially when Ashwagandha is taken in the evening, but some may feel sedated or drowsy, especially at higher doses.
8. Who should not take Ashwagandha?
Avoid if pregnant or breastfeeding, if you have hormone-sensitive cancers, active thyroid issues, autoimmune diseases, or liver problems. Consult a healthcare provider for personalized advice.
9. How do I know if my Ashwagandha supplement is high quality?
Look for extracts standardized to at least 5% withanolides and verified by third-party testing (e.g., NSF, USP, ConsumerLab). Choose well-known brands using KSM-66, Sensoril, Shoden, or Asvaman®.
10. Can Ashwagandha be used alongside therapy or other stress management techniques?
Absolutely! Ashwagandha works best as part of a broader approach, including healthy sleep, exercise, mindfulness, and professional therapy—not as a replacement for them.