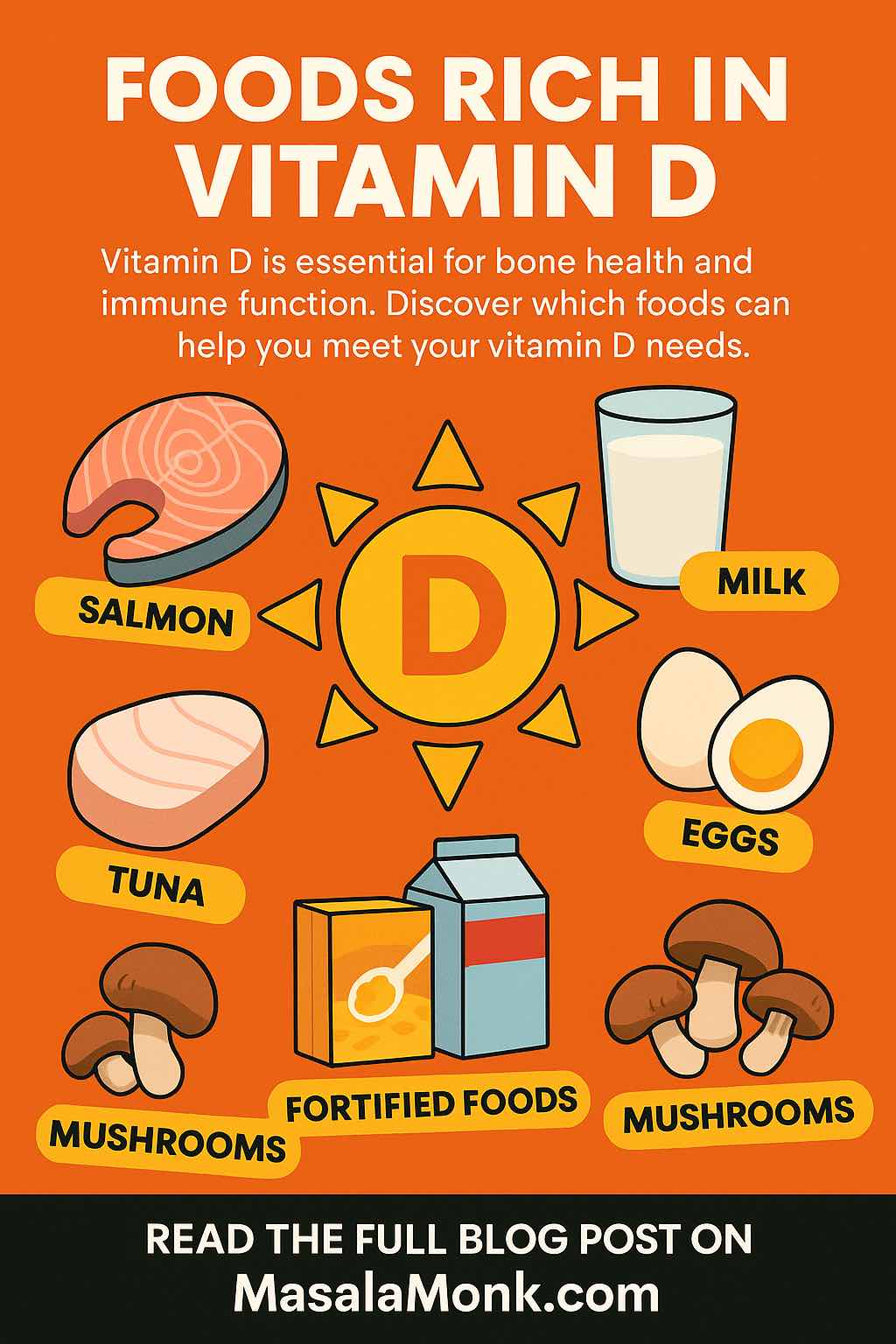
If you’ve ever wondered “Vitamin D comes from what food?” or “Which fruits have Vitamin D?”, you’re not alone. Many people are looking for dietary sources of Vitamin D, especially Vitamin D3, because they’ve heard it’s crucial for strong bones, immunity, and overall health — but aren’t sure which foods to eat.
Here’s the truth: sunlight is our best source of Vitamin D, but not everyone gets enough sun exposure year-round. That’s where food comes in. Unfortunately, there are very few natural food sources of Vitamin D — and even fewer plant-based ones — so knowing exactly where to find it matters.
This guide will give you:
- A clear list of natural Vitamin D3-rich foods
- Fortified foods to help fill the gap
- Insight into fruits and vegetables (and why they’re tricky)
- Tips for absorbing Vitamin D better from food
Read More: Vitamin D and Weight Loss
In case you think or know you are deficient, consider Top-Rated Vitamin D Supplements Available on Amazon India
Why Vitamin D Matters
Vitamin D plays several critical roles:
- Bone health: Helps your body absorb calcium and phosphorus
- Immunity: Supports the immune system’s defense against infections
- Muscle function: Important for strength and balance
- Mood: Linked to brain health; deficiencies have been associated with depression
For most healthy adults, the recommended daily allowance (RDA) is:
- 600 IU (15 mcg) for ages 1–70
- 800 IU (20 mcg) for ages 71+
(U.S. NIH & Indian Council of Medical Research guidelines align closely)
Read More: The Ergocalciferol Effect: 5 Vitamin D2-Rich Recipes for Healthy Bones
Natural Animal-Based Sources of Vitamin D3
Vitamin D3 (cholecalciferol) is the form found in animal foods. It’s generally more effective at raising and maintaining your blood vitamin D levels than D2 (the form found in some plant foods).
Top natural D3-rich foods:
| Food | Serving | Vitamin D (IU) | Notes |
|---|---|---|---|
| Cod liver oil | 1 Tbsp | 1,360 IU | Potent source; also high in vitamin A |
| Rainbow trout (cooked) | 3 oz | 645 IU | Mild flavor, versatile |
| Sockeye salmon (cooked) | 3 oz | 570 IU | Wild-caught higher than farmed |
| Light tuna (canned in water) | 3 oz | 231 IU | Convenient pantry staple |
| Sardines (canned in oil) | 3 oz | 164 IU | Eat with bones for calcium boost |
| Egg yolk | 1 large | 44 IU | Vitamin D is in the yolk, not the white |
| Beef liver | 3 oz | ~42 IU | Also rich in vitamin A, iron |
Why these foods matter:
If you eat animal products, a few servings of fatty fish per week plus eggs can significantly improve your vitamin D intake without supplements.
Do consider Top-Rated Vitamin D Supplements Available on Amazon India
Plant-Based & Fortified Sources
If you follow a vegetarian or vegan diet, natural options are very limited. Most plant-based vitamin D comes from fortified foods.
Key options:
| Food | Serving | Vitamin D (IU) | Notes |
|---|---|---|---|
| Mushrooms (UV-treated) | 1 cup raw | 300–1,100 IU | Vitamin D2, not D3, but still useful |
| Fortified soy milk | 1 cup | 119 IU | Check labels for “vitamin D added” |
| Fortified almond/rice/oat milk | 1 cup | 100–107 IU | Works in tea/coffee like dairy |
| Fortified orange juice | 1 cup | 100–117 IU | Not all brands are fortified |
| Fortified breakfast cereals | 1 serving | ~80 IU | Often with added iron and B vitamins |
| Fortified yogurt | 8 oz | ~116 IU | Dairy and plant-based types exist |
Fruits & Vegetables — The Surprising Truth
Natural vitamin D is virtually absent from fruits and vegetables. The only exceptions are:
- UV-exposed mushrooms (technically fungi, not plants)
- Fortified fruit juices (added vitamin D)
So if you see lists of “Vitamin D fruits,” they’re usually referring to fortified products — not naturally occurring vitamin D.
Read More: Are You at Risk of Vitamin D Deficiency? You might want to consider Top-Rated Vitamin D Supplements Available on Amazon India
Assess Your Vitamin D Intake
While our article explores various natural sources of Vitamin D and emphasizes the importance of maintaining adequate levels for optimal health, understanding your personal Vitamin D intake and synthesis is equally crucial. To help you evaluate your current Vitamin D status and identify potential areas for improvement, we’ve developed an interactive Vitamin D Deficiency Risk Assessment Tool.
Why Use the Vitamin D Assessment Tool?
Our lifestyles, dietary habits, and even the amount of sunlight we receive can significantly impact our Vitamin D levels. This tool is designed to offer personalized insights based on your specific circumstances, including:
- Personal Lifestyle: Factors such as sun exposure and outdoor activities.
- Dietary Habits: Your regular intake of Vitamin D-rich foods and supplements.
- Risk Level: An estimation of your risk for Vitamin D deficiency and practical suggestions for improvement.
By understanding your risk level, you can make informed decisions about dietary choices, sun exposure, and whether to consult a healthcare provider for further advice.
How to Use the Tool
Simply answer a few questions about your daily habits and lifestyle. The tool will then calculate your estimated risk of Vitamin D deficiency and provide tailored recommendations for enhancing your Vitamin D intake.
Vitamin D Deficiency Risk Assessment
Your Personalized Assessment Results
The assessment takes just a few minutes to complete and could be a crucial step towards improving your overall health and well-being. Remember, while this tool offers valuable insights, it's always a good idea to consult with a medical professional for personalized health advice.
Vitamin D Fortified Foods, India-Specific Sources & Absorption Tips
Fortified Foods — Why They Matter
Because very few foods naturally contain Vitamin D, fortification has become an important public health tool worldwide. This means vitamin D is added to commonly eaten foods to help prevent deficiency.
In India, where vitamin D deficiency is widespread due to limited sun exposure for many lifestyles, the Food Safety and Standards Authority of India (FSSAI) has actively promoted fortification through the +F symbol. You’ll often find fortified vitamin D in:
- Packaged milk and curd
- Edible oils
- Wheat flour and rice (in some programs)
- Salt (as part of multi-micronutrient fortification)
You might like to read: Vitamin B12 Rich Foods to Eat
Common Vitamin D Fortified Foods
These foods may be fortified in different amounts — always check the label for IU or micrograms (µg):
| Food | Typical Serving | Vitamin D (IU) if fortified |
|---|---|---|
| Cow’s milk (low-fat/skim) | 1 cup | ~115–117 IU |
| Plant-based milks (soy, almond, oat, rice) | 1 cup | 100–144 IU |
| Yogurt | 8 oz | 100–120 IU |
| Breakfast cereals | 1 serving | 80–100 IU |
| Orange juice (100%, fortified) | 1 cup | 100–117 IU |
| Margarine & spreads | 1 tsp | 40–50 IU |
| Cheese (fortified varieties) | 1 oz | 40–60 IU |
| Cooking oil (fortified) | 1 Tbsp | ~20–40 IU |
Absorption Tips — Getting the Most from Vitamin D Foods
Vitamin D is fat-soluble, which means your body absorbs it best when eaten with fat.
Tips to maximize absorption:
- Pair fortified orange juice with nuts or avocado toast
- Enjoy grilled salmon with a drizzle of olive oil
- Add a side of full-fat yogurt to a fruit plate
- Cook UV-treated mushrooms in ghee or coconut oil
- Make oatmeal with fortified soy milk and nut butter
Also Consider: Top-Rated Vitamin D Supplements Available on Amazon India
Why Vitamin D3 Form Matters
- Vitamin D3 (cholecalciferol) — found in animal products and some fortified foods — raises blood vitamin D levels more effectively than D2 in most people.
- Vitamin D2 (ergocalciferol) — found in mushrooms and plant sources — still contributes but may require higher intake to match the same blood levels as D3.
Creative Ways to Add Vitamin D Foods to Your Day
- Breakfast: Scrambled eggs with fortified cheese + fortified cereal with soy milk
- Lunch: Sardine salad with olive oil dressing + a glass of fortified orange juice
- Snack: Fortified yogurt topped with walnuts
- Dinner: Grilled trout with sautéed UV-treated mushrooms
- On-the-go: Protein smoothie with fortified almond milk and peanut butter
Might like to read: Best Fish Oil Supplements on Amazon India
Vitamin D Foods and Fruits List + FAQs (2025)
Comprehensive Vitamin D Foods, Fruits & Vegetables Table
(Values are approximate per typical serving — check labels for fortified foods)
| Food / Beverage | Standard Portion | Vitamin D (IU) | Notes |
|---|---|---|---|
| Cod liver oil | 1 Tbsp | 1,360 | Extremely rich; also high in vitamin A |
| Rainbow trout, cooked | 3 oz | 645 | Mild flavor, versatile |
| Sockeye salmon, cooked | 3 oz | 570 | Wild usually higher than farmed |
| Light tuna, canned in water | 3 oz | 231 | Easy pantry staple |
| Sardines, canned in oil | 3 oz | 164 | Also gives calcium if eaten with bones |
| Mackerel, cooked | 3 oz | 360 | Popular in coastal cuisines |
| Egg yolk | 1 large | 44 | Vitamin D is in the yolk |
| Beef liver, cooked | 3 oz | 42 | Rich in nutrients but acquired taste |
| Mushrooms (UV-treated) | 1 cup raw | 300–1,110 | Plant-based source (vitamin D2) |
| Fortified cow’s milk | 1 cup | 115–117 | Common in India’s +F program |
| Fortified soy milk | 1 cup | 119 | Dairy-free alternative |
| Fortified almond/rice/oat milk | 1 cup | 100–107 | Check brand’s label |
| Fortified yogurt | 8 oz | 100–120 | Dairy & plant-based types available |
| Fortified orange juice | 1 cup | 100–117 | Not naturally occurring — added D |
| Fortified breakfast cereals | 1 serving | 80–100 | Often paired with fortified milk |
| Fortified margarine/spreads | 1 tsp | 40–50 | Used in some packaged products |
| Fortified cooking oil | 1 Tbsp | 20–40 | Common in FSSAI +F initiative |
FAQs About Vitamin D in Food
1. Which fruit is highest in vitamin D?
No fruit naturally contains significant vitamin D. Fortified orange juice is the most common “fruit” source — about 100 IU per cup.
2. Is there vitamin D in vegetables?
Almost none naturally, except for UV-treated mushrooms (technically fungi). They can provide a large boost.
3. What’s the difference between vitamin D2 and D3 in food?
D3 comes from animal sources (and some fortified foods) and generally raises blood levels more effectively. D2 comes from plant/fungal sources like mushrooms.
4. How can vegetarians get enough vitamin D from food?
Rely on fortified plant milks, fortified cereals, fortified juices, and UV-treated mushrooms.
5. Is cooking fish bad for vitamin D?
Cooking methods like baking, grilling, or steaming preserve most vitamin D. Deep frying may cause greater losses.
6. Do bananas have vitamin D?
No — bananas, like most fruits, contain no vitamin D.
7. How much vitamin D do I need daily?
Most adults: 600 IU (15 mcg); adults over 70: 800 IU (20 mcg).
8. Can I get enough vitamin D from food alone?
It’s possible, but challenging. Many people need a mix of food, sunlight, and supplements.
9. What is vitamin D fortified food?
A food with vitamin D added during manufacturing, such as fortified milk, plant milks, cereals, and juices.
10. Is too much vitamin D from food dangerous?
Toxicity is rare from food alone — it’s more of a risk with high-dose supplements.
Quick Checklist: Meeting Your Vitamin D Needs
- ✅ Include fatty fish (trout, salmon, sardines) in meals a few times per week
- ✅ Add fortified milk or plant milk to daily beverages
- ✅ Use fortified cereals and juices for breakfast variety
- ✅ Enjoy UV-treated mushrooms in stir-fries or soups
- ✅ Pair vitamin D foods with healthy fats for better absorption
- ✅ Check labels for +F fortification in India
Also Read What Is Fish Oil Good For? Benefits, Side Effects, and More
💡 Final Tip:
Sunlight is still your most natural vitamin D source — aim for moderate exposure when possible, and use food and fortified options to fill the gap.
📖 Read more nutrition guides at MasalaMonk.com for science-backed tips, tasty recipes, and practical wellness advice.