Let’s set the vibe right away: if a single cup of tea could flatten your stomach by Friday, the internet would have run out of tea by Saturday. Green Tea for Weight Loss isn’t magic—it’s a nudge. But when you stack that nudge with the basics (a calorie deficit, some movement, decent sleep), the dial starts to move. Slowly? Yes. Reliably? Also yes.
Here’s everything you actually need: what green tea does (and doesn’t) do, how to brew it so it works for you, when to drink it for a gentle appetite edge, how matcha fits in, how to stay safe with extracts, and practical plans, recipes, and FAQs you can act on today. Let’s go.
Why Green Tea for Weight Loss Works (in real life)
First things first, the science in one breath: the catechins in green tea—especially EGCG—plus a bit of caffeine can gently increase energy expenditure and fat oxidation. It’s not a fat torch; it’s a quiet assist. The National Center for Complementary and Integrative Health has a good plain-English summary of where green tea helps, where it’s mixed, and when to be cautious with supplements. Read their overview once, and you’ll see why our approach here is “ritual first, hype never.” NCCIH overview on green tea. NCCIH
Now, here’s what matters for results:
- Expect modest changes on the scale from tea alone—think of it as background support rather than the main event. Over weeks, though, those small differences compound when you’re also eating to your goal and moving your body. As the NCCIH notes, product composition (how much catechin, how much caffeine) and your activity level influence outcomes. As that overview puts it, this is a nudge, not a shortcut.
- Where the magic shows up more visibly: your waistline. In a randomized trial, people who drank a catechin-rich tea while following an exercise plan saw greater reductions in total and subcutaneous abdominal fat versus the exercise-only group over 12 weeks. That’s the famous synergy: tea + movement. Randomized exercise study. PubMed
- Appetite effects are mild. For many people, a cup 30–60 minutes before a meal takes the edge off. For others, there’s no big difference. We’ll show you how to time it and test it.
So yes, Green Tea for Weight Loss works—just not the “lose 10 kg in 10 days” kind of “works.” It’s the grown-up version: consistent, modest, additive.
Medical Disclaimer
This article is educational and not medical advice. Green tea and green tea extracts can interact with medicines (e.g., beta-blockers like nadolol, statins like atorvastatin) and high-dose extracts carry rare liver risks. If you’re pregnant, breastfeeding, have liver disease, or take prescription meds, talk to your clinician first. Avoid extract dosing on an empty stomach; keep total EGCG well under 800 mg/day. Stop and seek care if you notice nausea, abdominal pain, dark urine, or unusual fatigue. Caffeine affects sleep, anxiety, and blood pressure—time your intake accordingly.
Last updated: 16 September 2025 (IST)
How to Use Green Tea for Weight Loss (simple, actionable)
You don’t need a lab, a kitchen scale, or a secret import source. You just need decent tea, hot water, and a repeatable routine. Pick one of these to start, then layer more if you enjoy them.
Option A — The Two-Cup Anchor (your everyday base)
- How much: 2–4 cups/day (about 400–600 ml total), spread from morning to mid-afternoon.
- Brew smart: Use 80–85°C water (not boiling), steep 2–3 minutes. This preserves catechins and keeps bitterness low.
- When to drink:
- 30–60 min before meals to experiment with a subtle appetite effect.
- 30–45 min before a walk or workout to ride the exercise synergy we just talked about (as that study found, this combo helps abdominal fat over time).
- Sleep matters: If caffeine makes you buzzy, keep your last caffeinated cup 6–8 hours before bed and switch to decaf green tea or a calming herbal in the evening.

Need flavor without sugar? Rotate spice infusions so the habit stays interesting:
- Try a week of these easy Green Tea & Spice Infusions for Weight Loss—ginger, cinnamon, mint, lemon… pick your mood.
- Love warmer notes? Brew a cup the cinnamon-green tea way or go aromatic with clove + cardamom. Variety helps adherence—adherence gets results.
Option B — Matcha: a stronger “green” for busy humans
Matcha is powdered whole green tea leaf, so you drink the leaf itself (hello, catechins). It’s an easy win if you like lattes or smoothies.
- Dose: ½–1 tsp (1–2 g) once or twice daily.
- Prep: Whisk with hot (not boiling) water for a straight cup; or blend into a matcha protein shake (recipe below) for better satiety and workout support.
- Timing: Morning for focus, early pre-workout for a gentle kick; decaf versions at night if you’re caffeine-sensitive.
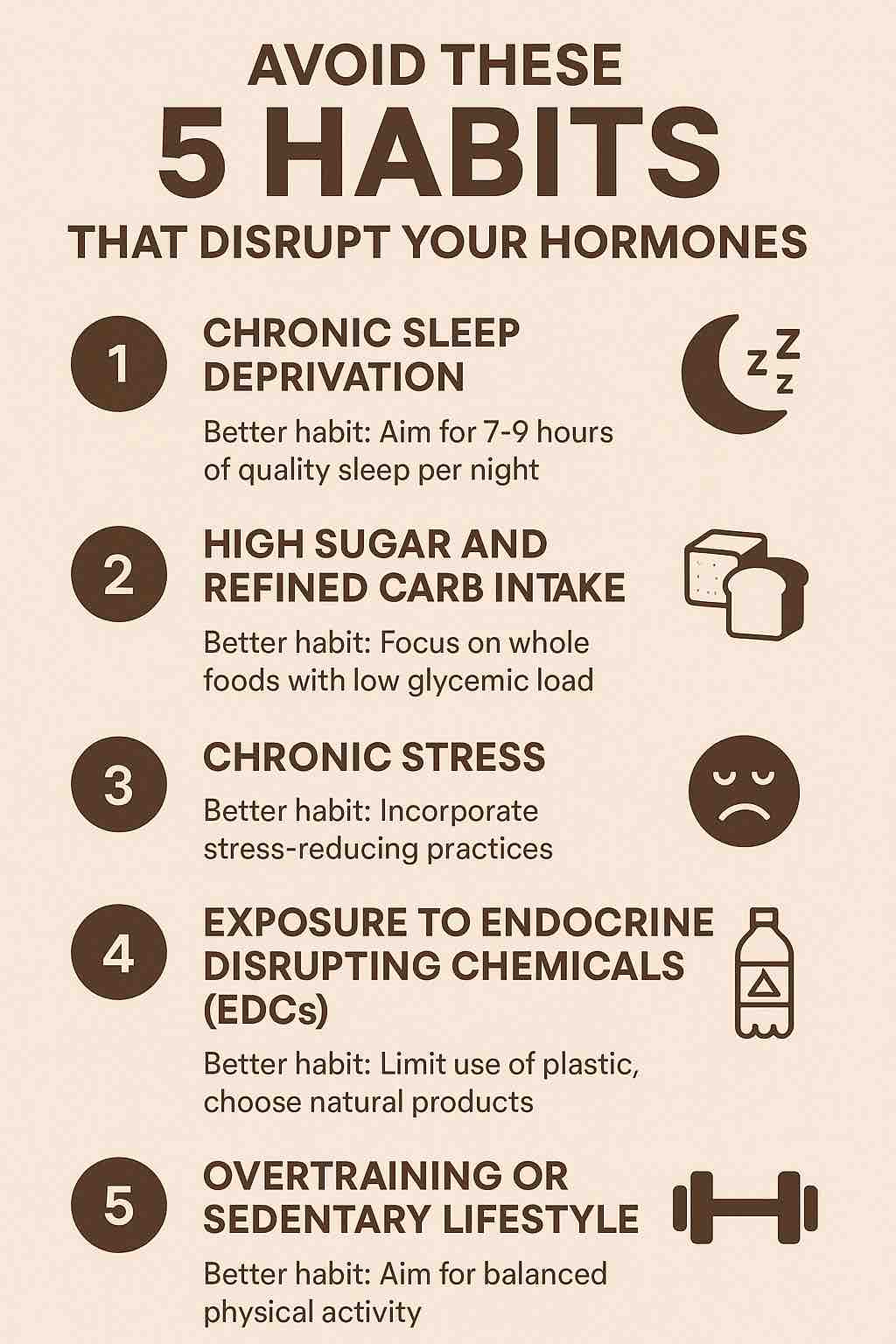
Managing stress while cutting? Smart move. For broader “tea + stress” help, see How Your Favorite Brew Can Help Manage Cortisol and 5 Herbal Teas That Help Lower Cortisol. Stress down, adherence up. Win-win.
Option C — Capsules/Extracts: advanced only (read safety before you buy)
If you struggle to get enough catechins from beverages, standardized green tea extract can be an option—but supplements are where safety needs guardrails.
- Typical labels: 200–300 mg EGCG per capsule. Most people split 1–2 caps/day with food.
- Safety lines you should actually know: The European Food Safety Authority concluded that doses ≥800 mg/day of EGCG from supplements were associated with statistically significant increases in liver enzymes; traditional brewed tea, on the other hand, is generally safe (rare idiosyncratic reactions can occur). Start low, avoid empty-stomach dosing, and stop if you feel unwell. EFSA scientific opinion. European Food Safety Authority
- The UK’s Committee on Toxicity reiterated caution with high-dose extracts and multi-herb stacks. TL;DR: go gentle, go with food, and don’t stack with mystery “fat burner” blends. UK COT 2024 background. cot.food.gov.uk
If you’re supplement-curious in general, browse NCCIH’s notes on interactions and who should be careful; it’s short and worth your time (as the overview explains).
Medical Disclaimer
This article is educational and not medical advice. Green tea and green tea extracts can interact with medicines (e.g., beta-blockers like nadolol, statins like atorvastatin) and high-dose extracts carry rare liver risks. If you’re pregnant, breastfeeding, have liver disease, or take prescription meds, talk to your clinician first. Avoid extract dosing on an empty stomach; keep total EGCG well under 800 mg/day. Stop and seek care if you notice nausea, abdominal pain, dark urine, or unusual fatigue. Caffeine affects sleep, anxiety, and blood pressure—time your intake accordingly.
Last updated: 16 September 2025 (IST)

“Okay, but what results can I expect?”
Let’s be very clear and very adult about expectations:
- On the scale: Green tea by itself leads to modest weight changes. It’s the kind of quiet helper you barely notice week to week… until you compare month to month, especially when paired with a reasonable calorie deficit and movement (as that overview states).
- At the waist: This is where Green Tea for Weight Loss shows up better. Over about 12 weeks, catechin-rich tea—especially when paired with exercise—has repeatedly led to small but meaningful reductions in abdominal fat in controlled trials (as the randomized exercise study found).
- Appetite: Some folks swear a pre-meal cup tames the mindless munching. Others shrug. Try it for a week and keep it if it helps.
Bottom line: treat tea like a daily ritual that keeps you pointed in the right direction.
Recipes you’ll actually make (and keep making)
Let’s make this effortless. Two hot, two cold; all quick.
Ginger + Green Tea (5 minutes, big flavor)
- 250 ml hot water (80–85°C)
- 1 tsp loose green tea (or 1 bag)
- 3–4 thin ginger slices
- Optional: lemon wedge
Steep 2–3 minutes, strain, sip. Simple. (And if you want a weekly rotation, peek at our Green Tea & Spice Infusions collection.)
Cinnamon Green Tea (comforting, subtly sweet)
- 250 ml hot water + 1 tsp green tea
- ½ small Ceylon cinnamon stick while steeping (2–3 min); remove stick
Prefer deeper spice? This walk-through is short and useful: Cinnamon-Green Tea.
Matcha Protein Shake (satiety + muscle-friendly)
- 1 tsp matcha
- 200 ml chilled milk/alt-milk
- 20–30 g whey/plant protein
- Ice + optional handful spinach
Blend 20 seconds. Breakfast, nailed.
Iced “Flat Tummy” Refresher (pre-meal ritual)
- Brew 2 cups green tea; chill
- Add lemon, mint, and ice
Drink before lunch for a small satiety nudge. Habit + timing = quiet win.
Matcha vs Green Tea for Weight Loss (which should you choose?)
Short version: both work if you use them. Matcha often has more catechins per serving because you consume the whole leaf; regular brewed green tea is gentler and endlessly sippable. Choose based on your routine:
- Crave a morning ritual and like lattes or smoothies? Matcha wins.
- Prefer many small sips through the day? Brewed green tea is your friend.
- Sensitive to caffeine? Use decaf versions later in the day (keep the ritual, protect sleep).
If stress and sleep are getting in the way (they always do), rotate in evening herbals from this cortisol-friendly short list. Better sleep = better appetite control tomorrow.
Safety & Side Effects of Green Tea for Weight Loss (quick but essential)
- Brewed tea (most people): Generally safe. Watch your caffeine cutoff time. As the NCCIH overview notes, green tea can interact with certain meds (e.g., nadolol, atorvastatin), so check with your clinician if you’re on prescriptions, pregnant, or breastfeeding. NCCIH overview.
- Extracts/capsules: This is where rare liver issues show up, especially at higher doses and in multi-herb stacks. Keep supplemental EGCG well under 800 mg/day, take with food, avoid empty-stomach dosing, and stop immediately if you notice nausea, abdominal pain, dark urine, or unusual fatigue. As the EFSA opinion concluded, ≥800 mg/day is the range where liver enzymes rise in trials; and as the UK COT background notes, concentrated extracts are the main concern—not your normal brewed tea. EFSA opinion; UK COT 2024.
Green Tea for Weight Loss: A 12-Week Blueprint (repeat as needed)
This plan respects how the body changes—gradually. It’s light on rules, heavy on rhythm.
1–2 Weeks : Build the ritual (keep it easy)
- Pick Option A (Two-Cup Anchor) or Option B (Matcha).
- Set phone alarms for Cup 1 (mid-morning) and Cup 2 (pre-walk/workout).
- Walk 8–10k steps/day (break it into chunks—three 10-minute walks count).
- Lift 2–3×/week (20–30 minutes: push/pull/legs; simple beats perfect).
3–6 Weeks : Layer tiny improvements (small hinges, big doors)
- Keep your two tea anchors.
- Add pre-meal timing before your largest meal (tea 30–60 min prior).
- Protein to 1.6–2.2 g/kg target body weight; fiber to 25–35 g/day.
- Bedtime: consistent, screens down, decaf or herbal after dinner.
Also Read: The Science of Protein: Maximizing Muscle Growth and Recovery
7–12 Weeks : Turn the dial (just a click or two)
- Add a third cup on higher-hunger afternoons (or a decaf if it’s late).
- Introduce one interval or hill session weekly (short, honest effort).
- Track waist and photos more than the scale; as the exercise study found, abdominal fat shifts are the tell here.
Want food scaffolding? Start with 5 Foods that Reduce Belly Fat and Spinach—Nutrition, Benefits & 5 Practical Ways. Plant-heavy, protein-forward—boringly effective.
Curious about ACV as a sidekick? Keep expectations realistic and try ACV on an Empty Stomach, or, if you’re supplement-curious, skim ACV Gummies: Pros, Cons & FAQs. Use what helps you adhere; skip what doesn’t.
Frequently Asked (Real) Questions about Green Tea for Weight Loss
1) Is green tea an appetite suppressant?
Sort of, sometimes. Many people notice a gentle reduction in appetite if they drink a cup 30–60 minutes before meals. Others don’t. That’s why we test. Keep it if it helps.
2) What’s the “best” green tea for weight loss?
The one you’ll drink daily. Practically speaking, matcha tends to deliver more catechins per serving (whole leaf), while brewed green tea wins on sip-ability. You don’t need to overthink it.
3) Will this flatten my stomach?
No drink targets belly fat in isolation—but over about 12 weeks, catechin-rich tea paired with exercise has produced small reductions in abdominal/visceral fat in controlled studies. That’s why our plan treats tea as a pre-workout ritual as often as a pre-meal one (as that study found).
4) Can I stack green tea with other “fat burners”?
You can, but should you? Most stacks add side effects faster than they add benefits, and concentrated blends are where safety issues pop up. If you want “stronger,” do it safely and sanely: a standardized extract with food, staying well under 800 mg/day EGCG (as the EFSA opinion concluded). And only if you’re already nailing the basics.
5) What about decaf—is it worth it?
Decaf green tea keeps the ritual, hydration, and some polyphenols. You lose the small caffeine boost, but if it protects sleep, it may help you more overall. Use decaf after lunch and herbals at night—your future self will thank you.
6) Can I combine green tea with ACV, cinnamon, ginger, etc.?
Absolutely—if it helps you stick to the plan. Try the spice infusions linked above for taste without sugar, or the matcha protein shake for actual fullness. If it feels like a treat, you’ll keep doing it.
7) Any interactions or “don’ts”?
Yes—green tea can interact with some meds (e.g., nadolol, atorvastatin), and high-dose extracts carry liver risk, especially on an empty stomach or in multi-herb stacks. If you take prescriptions, are pregnant/breastfeeding, or have liver concerns, talk to your clinician first (as the NCCIH overview advises).
Green Tea for Weight Loss: Quick Reference (pin this)
- Brewed green tea: 2–4 cups/day; 80–85°C, 2–3 min steep; last caffeinated cup 6–8 h before bed.
- Matcha: ½–1 tsp (1–2 g) once or twice daily; whisk (not boiling water) or blend into a protein shake.
- Timing: 30–60 min pre-meal for appetite testing; 30–45 min pre-workout for the exercise synergy.
- Extracts (advanced): 200–300 mg EGCG/cap; keep total well under 800 mg/day; with food; stop if unwell.
- Evening: switch to decaf or calming herbals for better sleep (and better appetite control tomorrow).
- Food frame: protein + fiber + plants. For easy ideas, see 5 Foods that Reduce Belly Fat and Spinach—5 Practical Ways.
Sources
- General usefulness, interactions, and safety context: NCCIH overview on green tea. NCCIH
- Abdominal/visceral fat + exercise synergy: Randomized trial: catechin beverage + exercise → greater abdominal fat loss over 12 weeks. PubMed
- Supplement safety & liver considerations (EGCG thresholds): EFSA scientific opinion on green tea catechins; UK COT 2024 background statement. European Food Safety Authority+1
Final word (and then go brew)
“Green Tea for Weight Loss” really means: a small, daily ritual that helps you make better choices, train a little more consistently, and feel a little more in control. That’s the stuff that adds up. Brew your first cup, take a 10-minute walk after lunch, and repeat tomorrow. Boring? Maybe. Effective? Absolutely.
Medical Disclaimer
This article is educational and not medical advice. Green tea and green tea extracts can interact with medicines (e.g., beta-blockers like nadolol, statins like atorvastatin) and high-dose extracts carry rare liver risks. If you’re pregnant, breastfeeding, have liver disease, or take prescription meds, talk to your clinician first. Avoid extract dosing on an empty stomach; keep total EGCG well under 800 mg/day. Stop and seek care if you notice nausea, abdominal pain, dark urine, or unusual fatigue. Caffeine affects sleep, anxiety, and blood pressure—time your intake accordingly.
Last updated: 16 September 2025 (IST)