Greek yogurt has taken grocery store shelves by storm over the last decade, marketed as everything from a high-protein breakfast to a gut-friendly snack. But is Greek yogurt really a smart choice if you have diabetes—or are at risk for it?
Let’s dig into the science, compare types of yogurt, and give you practical tips on how to include Greek yogurt in your diabetes-friendly meal plan.
🥄 What Makes Greek Yogurt Different?
Greek yogurt is strained to remove much of the liquid whey, resulting in a thick, creamy texture. This process makes it:
- Higher in protein (about twice that of regular yogurt)
- Lower in carbohydrates (because some lactose is strained away)
- Denser in nutrients like calcium, potassium, and B-vitamins
But that’s not the whole story: Whether Greek yogurt is healthy for people with diabetes depends on what kind you choose, how much you eat, and what you pair it with.
🧬 What Does the Latest Research Say?
🔬 Prevention: Greek Yogurt Lowers Risk of Diabetes
- Recent reviews (2024, Critical Reviews in Food Science and Nutrition) show:
Regular yogurt eaters (at least 80–125 g per day—about half a cup) have a 14% lower risk of developing type 2 diabetes compared to non-yogurt eaters. - Mechanisms at play:
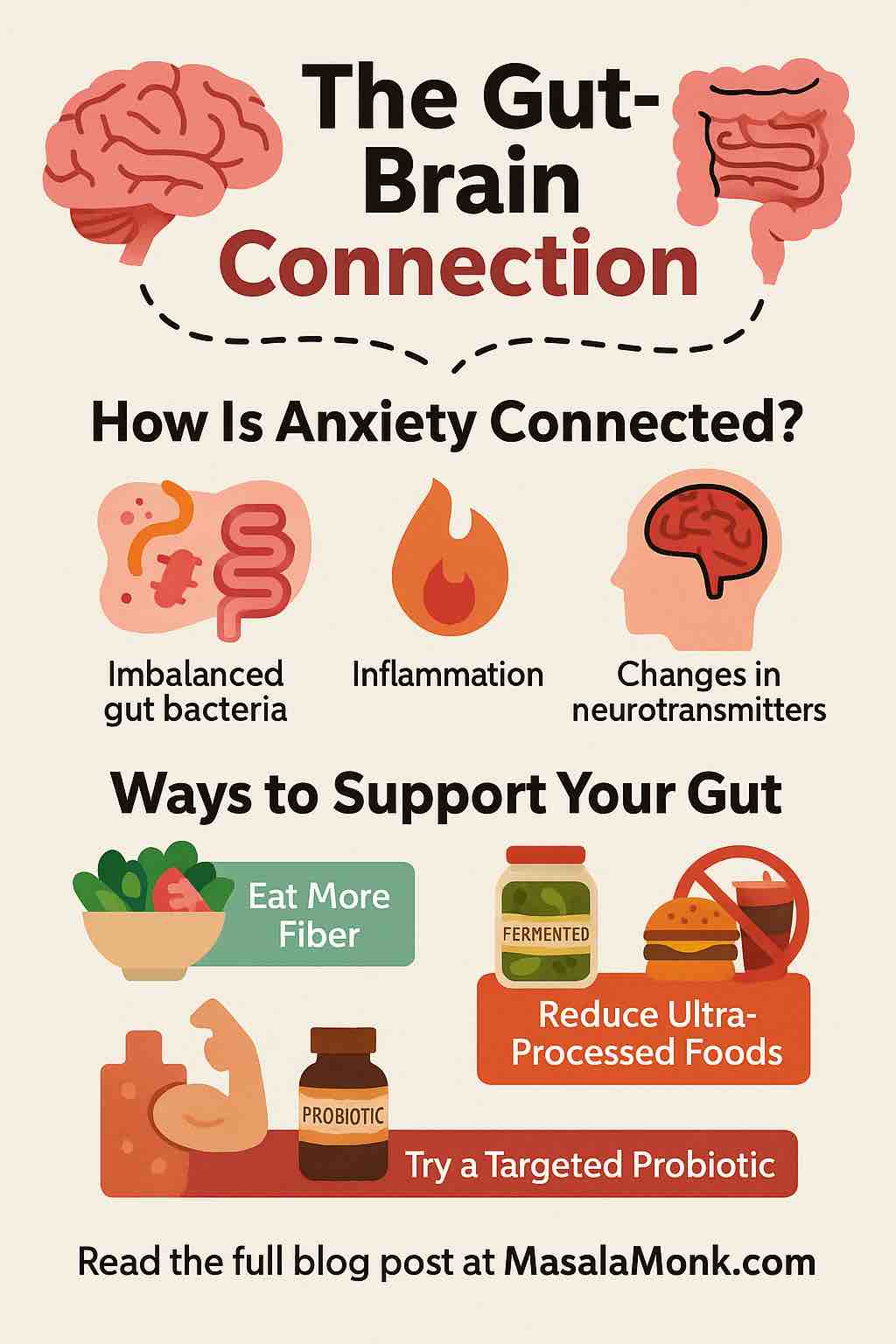
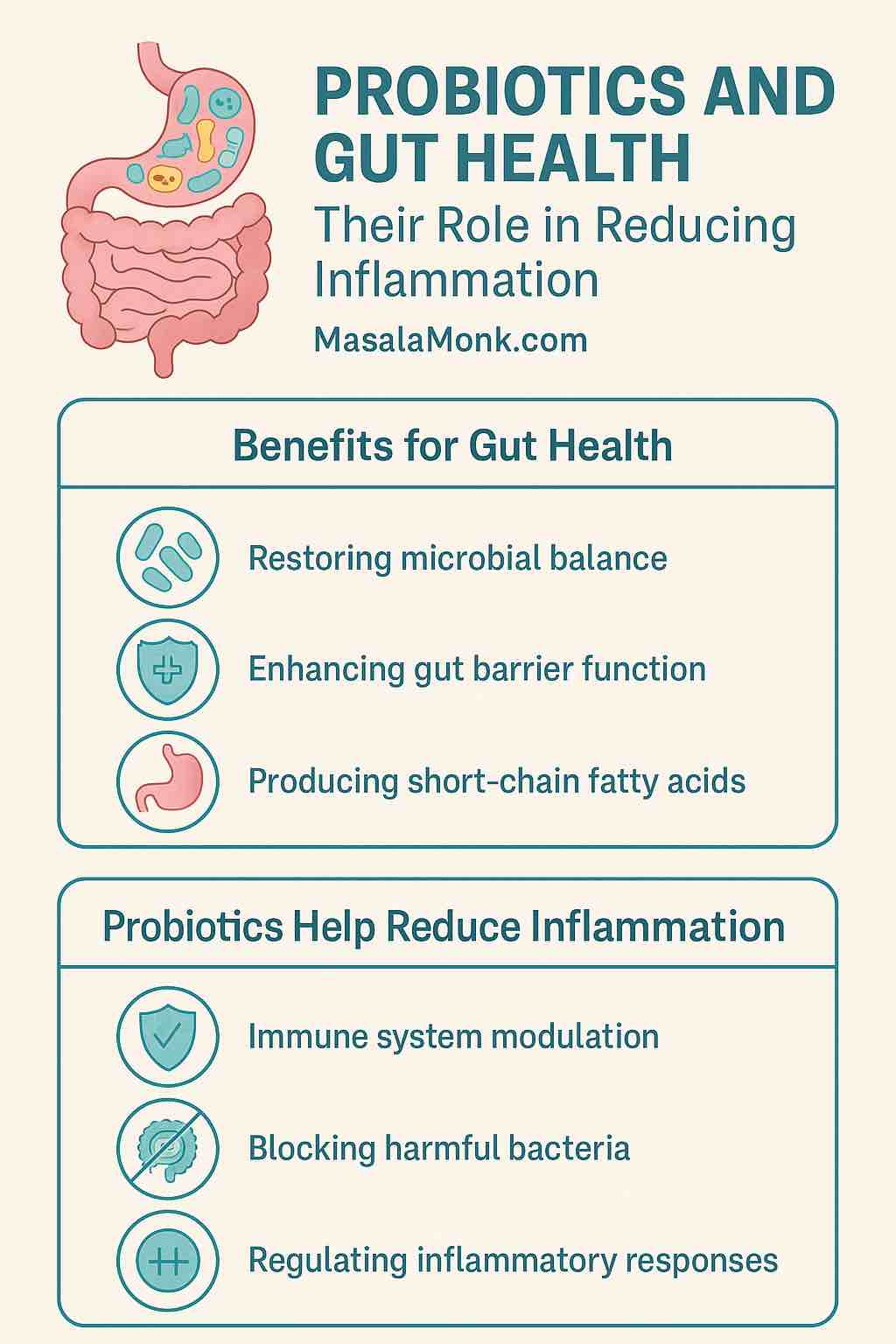
- Probiotics (live “good” bacteria) in yogurt help reduce inflammation and improve insulin sensitivity.
- High protein slows digestion and reduces blood sugar spikes after meals.
🩺 Management: Better Blood Sugar Control in Diabetics
- Clinical trials (2025, ScienceDirect):
People with type 2 diabetes who added full-fat Greek yogurt (200 g daily, about ¾ cup) saw improved fasting glucose and lower HbA1c after just 12 weeks. - The power of probiotics:
Yogurt enriched with Lactobacillus and Bifidobacterium species provided extra benefit in blood sugar and gut health.
🏛️ Official Guidance: FDA Allows Diabetes Health Claim
In 2024, the U.S. FDA approved a qualified health claim:
“Eating at least 2 cups of yogurt per week may reduce the risk of type 2 diabetes.”
Note: Applies to all yogurts, but especially those without added sugars.
🥗 How Greek Yogurt Supports People With Diabetes
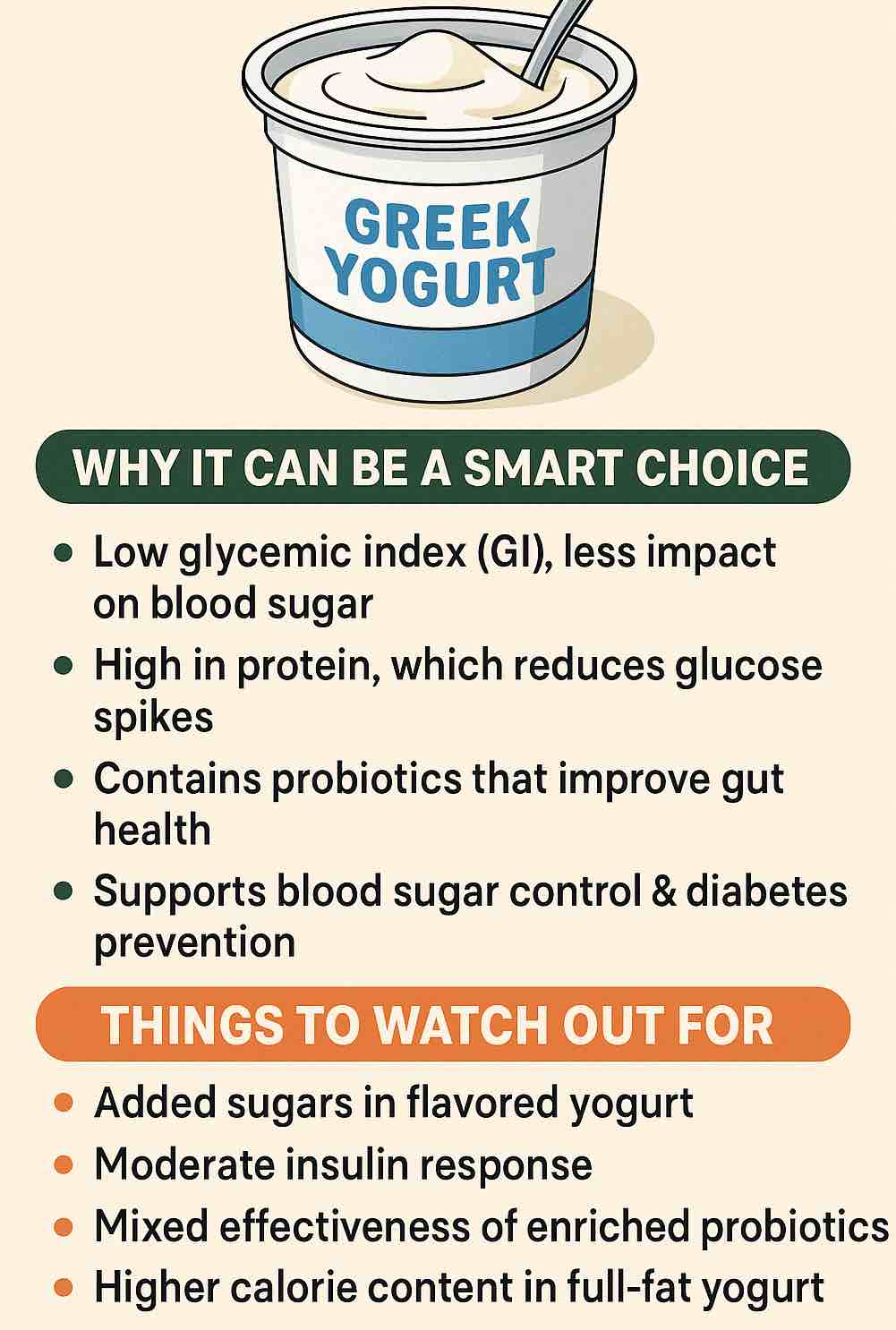
1. Low Glycemic Index (GI)
- Plain Greek yogurt has a GI of 27–41 (low is <55), so it won’t spike your blood sugar like white bread or sugary snacks.
2. High in Protein
- 15–20 g protein per cup keeps you full, curbs appetite, and slows sugar absorption.
3. Source of “Good” Fats
- Full-fat versions help you feel satisfied and may offer extra blood sugar benefits—just be mindful of portion size and total daily calories.
4. Packed With Probiotics
- “Live and active cultures” support gut health, which new research links to better blood sugar regulation and reduced inflammation.
5. Easy to Pair for Balanced Meals
- Pairs perfectly with berries, nuts, and seeds for a nutrient-dense, filling, and low-GI meal.
⚠️ What to Watch Out For
- Hidden Sugars: Flavored yogurts often have 2–4+ teaspoons of added sugar per serving—stick to plain!
- Read the Label: Aim for ≤15 g carbs and ≤10 g sugar per serving.
- Fat Content: Full-fat is fine for most, but check with your doctor if you have heart disease or are watching saturated fat.
- Individual Response: Test your blood sugar after eating new foods—everyone’s body is a little different.
🛒 How to Shop for the Best Greek Yogurt
- Choose Plain, Unsweetened Greek Yogurt
Look for “live and active cultures” on the label. - Pick Your Fat Level
- Full-fat (whole milk): Creamiest, most satisfying—may be best for blood sugar control.
- Low-fat or nonfat: Lower in calories, but still high in protein.
- Your best choice depends on your overall eating pattern and health profile.
- Watch the Ingredients List
- Should be short: Milk, cream, live cultures.
- Avoid: Sugar, syrup, “fruit on the bottom,” artificial sweeteners if possible.
🥣 Smart Ways to Enjoy Greek Yogurt If You Have Diabetes
- Breakfast Bowl:
Top ½–1 cup plain Greek yogurt with a handful of berries, a tablespoon of chia seeds or nuts, and a sprinkle of cinnamon. - Savory Snack:
Stir in lemon juice, garlic, and fresh herbs—use as a veggie dip or sandwich spread. - Smoothie Base:
Blend with unsweetened almond milk, spinach, berries, and a scoop of protein powder. - Swirl into Soups and Stews:
Adds creaminess without the carbs of flour or cornstarch. - Dessert Fix:
Mix with a little vanilla extract and serve with a few fresh strawberries.
🏁 Bottom Line: The Verdict on Greek Yogurt for Diabetes
Plain Greek yogurt—with live cultures, minimal added sugar, and your choice of fat level—is one of the most diabetes-friendly foods out there.
It’s backed by new research for prevention, helps manage blood sugar, and has an FDA health claim to boot. Enjoy it regularly as part of a healthy, balanced diet.
Ready to give it a try?
Start with small servings, see how your body responds, and get creative with your add-ins. Your gut, your blood sugar—and your taste buds—will thank you.
References & Further Reading
- FDA: Yogurt & Reduced Risk of Type 2 Diabetes (2024)
- Meta-Analysis: Yogurt Intake and Diabetes Risk (2025)
- Greek Yogurt and Diabetes: Newest Trials (2025)
- USDA: Yogurt & Glycemic Control
- Healthline: Yogurt and Diabetes
Always consult your healthcare provider or registered dietitian before making major changes to your meal plan.
🧠 FAQs: Quick Answers
1. Is Greek yogurt safe for people with diabetes?
Yes. Plain Greek yogurt is low in carbohydrates, high in protein, and has a low glycemic index, making it safe and supportive for people managing diabetes when eaten in moderation.
2. Does Greek yogurt raise blood sugar levels?
Not significantly. Unsweetened Greek yogurt causes a much smaller rise in blood sugar compared to sweetened yogurts or high-carb snacks, thanks to its low carbohydrate and high protein content.
3. Is full-fat or nonfat Greek yogurt better for diabetes?
Both can be healthy choices. Recent research suggests full-fat Greek yogurt may have extra benefits for blood sugar control and satiety, but choose what fits your nutrition and heart health goals.
4. How much Greek yogurt can I eat per day if I have diabetes?
A typical serving is ½–1 cup (100–200 g) per day. This amount fits well within most diabetes meal plans and matches the intake seen in studies showing benefits.
5. Should I avoid flavored Greek yogurts?
Yes, in most cases. Flavored varieties often contain significant added sugars that can spike blood sugar. Choose plain Greek yogurt and add your own fresh fruit or flavorings.
6. What should I look for on the Greek yogurt label?
Check for:
- Carbohydrates: ≤15 g per serving
- Sugars: ≤10 g per serving
- Ingredients: Milk, cream, and live cultures (avoid added sugars, syrups, artificial flavors)
7. Can Greek yogurt help prevent type 2 diabetes?
Yes. Studies show regular yogurt consumption (including Greek yogurt) is linked to a lower risk of developing type 2 diabetes, especially when combined with a healthy lifestyle.
8. Is Greek yogurt a good source of probiotics?
Absolutely. Most Greek yogurts contain live cultures that promote gut health and may help improve insulin sensitivity and inflammation.
9. Can I eat Greek yogurt if I am lactose intolerant?
Possibly. Greek yogurt contains less lactose than regular yogurt, and many people with lactose intolerance can tolerate small servings. Try a small amount to see how you react.
10. What are healthy ways to enjoy Greek yogurt with diabetes?
Top with fresh berries, nuts, seeds, or cinnamon for a satisfying, balanced snack. Use as a base for dips, sauces, or smoothies—always avoid adding sugar or sweet syrups.