Introduction
Pregnancy is a remarkable journey, a time of profound physical and emotional changes. For many women, this journey includes navigating the challenges of gestational diabetes – a condition that not only impacts their health but also the well-being of their unborn child. This guide is crafted to be your companion through this journey, offering insights, strategies, and support to empower you in managing your diabetes diet effectively during pregnancy.
Gestational diabetes, a condition characterized by elevated blood sugar levels during pregnancy, often brings with it concerns and questions. How will it affect my pregnancy? What can I eat? How do I balance my nutritional needs with managing my blood sugar? These questions are at the heart of the journey for many expectant mothers. Understanding gestational diabetes is not just about managing a diet; it’s about embracing a lifestyle that supports both you and your baby’s health.
The stakes are high, but so are the opportunities for positive change. Managing your diet during this critical time can have lasting benefits, going beyond the health of your pregnancy. It’s about setting the stage for a healthier life for you and your baby. Our guide delves into the nuances of dietary management, tailored to each trimester’s specific needs, and extends its focus to postnatal nutrition and recovery.
Beyond the basics of what to eat and what to avoid, this guide explores how to create a balanced meal plan, manage cravings, and maintain stable blood sugar levels. It also addresses the emotional and physical aspects of pregnancy with gestational diabetes, offering tips for overall wellness and strategies for postpartum recovery.
As you navigate the chapters of this guide, remember that each pregnancy is unique. Our goal is to equip you with knowledge, provide practical advice, and offer reassurance. Whether you are newly diagnosed or familiar with gestational diabetes, this guide aims to be a resource you can turn to for clarity and confidence, helping you manage not just your diet, but also embrace a healthy and joyful pregnancy journey.
Continuing from the introduction, the next section provides a comprehensive understanding of gestational diabetes, crucial for effectively managing the condition during pregnancy.
Understanding Gestational Diabetes
What is Gestational Diabetes?
Gestational diabetes mellitus (GDM) is a health condition that emerges during pregnancy. It is characterized by higher-than-normal blood sugar levels that are first recognized during pregnancy. Unlike Type 1 or Type 2 diabetes, gestational diabetes is typically temporary and primarily occurs when the body can’t produce enough insulin – a hormone crucial for controlling blood sugar levels – to meet the additional demands of pregnancy.
Why It Matters
The significance of managing gestational diabetes cannot be overstated. Uncontrolled blood sugar levels can lead to various complications, affecting both the mother and the baby. For the mother, these include an increased risk of high blood pressure, preeclampsia, and the likelihood of requiring a cesarean section. For the baby, potential complications include premature birth, higher birth weight, and a higher risk of developing type 2 diabetes later in life.
Diagnosis and Monitoring
Gestational diabetes is typically diagnosed through routine screening between the 24th and 28th weeks of pregnancy. However, if you have risk factors such as a family history of diabetes, obesity, or advanced maternal age, screening might be done earlier. Monitoring blood sugar levels becomes an integral part of your daily routine once diagnosed.
Risk Factors
Several factors can increase the risk of developing gestational diabetes, including:
- Age (women over the age of 25 are at a higher risk).
- Family or personal health history of diabetes.
- Excessive weight gain during pregnancy.
- Being overweight or obese prior to pregnancy.
- Ethnicity (higher risk among Asian, Hispanic, African American, and Native American populations).
Lifestyle and Gestational Diabetes
Lifestyle plays a crucial role in managing gestational diabetes. Diet and exercise are the cornerstones of managing blood sugar levels. A balanced, nutritious diet and regular, moderate exercise can help keep blood sugar levels within a healthy range. Additionally, lifestyle changes made during pregnancy can have lasting benefits, reducing the risk of developing type 2 diabetes in the future.
The Emotional Impact
Being diagnosed with gestational diabetes can be stressful and overwhelming. Concerns about your health and your baby’s well-being are common. It’s important to acknowledge these feelings and seek support. This can come from healthcare providers, support groups, or counseling, which can provide not only practical advice but also emotional support.
This section of the guide aims to provide a detailed understanding of gestational diabetes, highlighting its importance, diagnosis, risk factors, and the impact of lifestyle and emotional health. It’s designed to inform and reassure expectant mothers, offering a foundation of knowledge from which to build effective management strategies for their pregnancy journey.
Building on the understanding of gestational diabetes, the next section delves into the critical aspect of dietary management during pregnancy. This part aims to provide a comprehensive approach to nutrition, addressing the unique needs and challenges faced by expectant mothers with gestational diabetes.
Dietary Management During Pregnancy
Essential Nutrients and Diet
A balanced diet is pivotal in managing gestational diabetes. It’s not just about controlling blood sugar levels but also ensuring that both the mother and the baby receive the necessary nutrients for healthy development:
- Carbohydrates: They are a crucial source of energy but need to be chosen wisely. Opt for complex carbohydrates like whole grains, legumes, and vegetables, which have a lower glycemic index and provide sustained energy release.
- Proteins: Essential for the growth and repair of tissues, including the development of the baby. Include a variety of sources, such as lean meats, poultry, fish, eggs, and plant-based proteins like lentils and beans.
- Fats: Focus on healthy fats that are vital for the baby’s brain development. Sources include avocados, nuts, seeds, and olive oil.
- Fiber: Fiber-rich foods aid in digestion and help manage blood sugar levels. Incorporate a variety of fruits, vegetables, and whole grains into your diet.
- Vitamins and Minerals: Key nutrients such as folic acid, iron, calcium, and vitamin D are essential. While prenatal vitamins can supplement dietary intake, it’s important to consume nutrient-rich foods.
Foods to Include and Avoid
Understanding which foods to include and which to limit is crucial:
- Include:
- Whole grains like quinoa, brown rice, and whole wheat products.
- Fresh vegetables, focusing on leafy greens and a variety of colors.
- Lean proteins, including chicken, fish, and plant-based options.
- Healthy fats, such as avocados, nuts, and olive oil.
- Low-glycemic fruits like berries, apples, and pears.
- Avoid or Limit:
- Sugary foods and beverages, including sweets and sodas.
- Refined carbohydrates like white bread and pasta.
- High-fat, fried, or greasy foods.
- Excessive caffeine and alcohol.
Meal Planning and Timing
Consistent meal timing and proper portion control are vital:
- Regular Meals and Snacks: Aim for three main meals and 2-3 smaller snacks throughout the day to maintain stable blood sugar levels.
- Portion Control: Be mindful of portion sizes, especially for carbohydrate-rich foods.
- Balanced Meals: Each meal should include a balance of carbohydrates, proteins, and healthy fats to ensure nutritional adequacy and manage blood sugar levels effectively.
Monitoring and Adjusting Your Diet
- Blood Sugar Monitoring: Regular monitoring helps you understand how different foods affect your blood sugar. This information is crucial in managing your diet effectively.
- Dietary Adjustments: Based on your blood sugar readings, you may need to adjust your carbohydrate intake or meal composition.
- Professional Guidance: Consult with a dietitian specializing in pregnancy diets for personalized meal planning and advice.
This section of the guide provides expectant mothers with practical and detailed guidance on managing their diet during pregnancy with gestational diabetes. It emphasizes the importance of a balanced diet rich in essential nutrients, the need for careful selection of foods, and the strategies for effective meal planning and blood sugar management. The focus is on empowering women with the knowledge and tools necessary to maintain both their health and their baby’s development.
Continuing from dietary management, the next section explores the specific nutritional needs and dietary adjustments required during each trimester of pregnancy for mothers with gestational diabetes. This part aims to provide tailored advice that addresses the evolving needs of both the mother and the developing baby throughout the pregnancy.
Addressing Specific Trimesters
First Trimester Focus: Laying the Nutritional Foundation
The first trimester is a critical period for fetal development, and dietary management plays a key role:
- Key Nutrients: Emphasize folic acid for preventing neural tube defects, along with iron, calcium, and vitamin D.
- Managing Morning Sickness: For women experiencing nausea, focus on small, frequent, and bland meals. Incorporate ginger or peppermint teas, which can help alleviate nausea.
- Blood Sugar Monitoring: Start monitoring blood sugar levels early to establish a baseline and make necessary dietary adjustments.
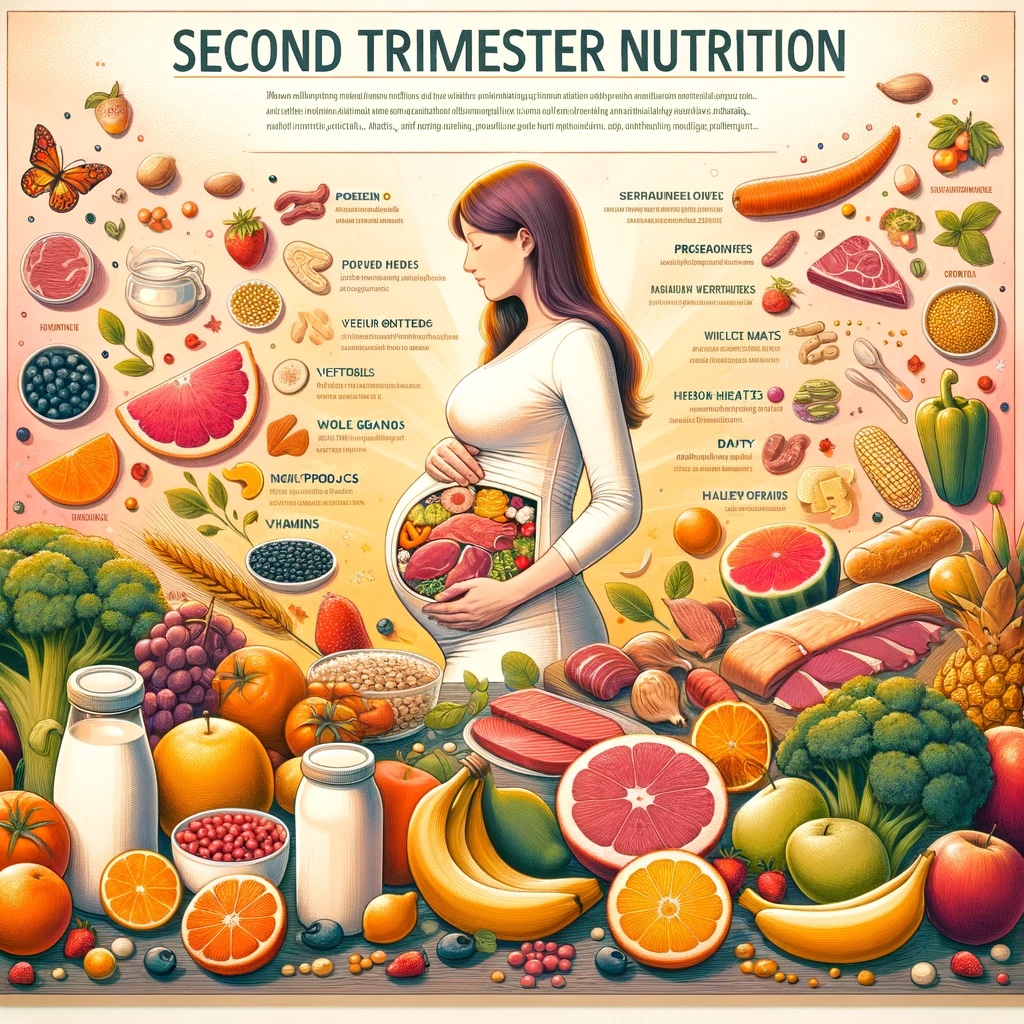
Second Trimester Adjustments: Supporting Growth and Development
During the second trimester, the baby’s growth accelerates, necessitating adjustments in the mother’s diet:
- Increased Caloric Intake: Slightly increase your calorie intake to support fetal growth, but focus on nutrient-dense foods.
- Balanced Meals: Ensure each meal is well-balanced with a mix of carbohydrates, proteins, and fats. Include a variety of fruits and vegetables for essential vitamins and minerals.
- Regular Blood Sugar Testing: Continue regular blood sugar monitoring and consult with your healthcare provider to adjust your diet or medication as needed.
Third Trimester Strategies: Preparing for Delivery
In the third trimester, the focus shifts to preparing for delivery and managing blood sugar levels:
- Complex Carbohydrates: Opt for complex carbs over simple sugars to maintain steady blood sugar levels.
- Protein-Rich Foods: Include adequate protein to support the final stages of fetal growth and your own muscle maintenance.
- Frequent, Smaller Meals: As the baby grows, you might find it more comfortable to eat smaller, more frequent meals. This can also help in managing blood sugar levels.
Dietary Considerations for Common Pregnancy Concerns
Each trimester may bring its unique challenges, such as increased risk of gestational hypertension or edema. Adjust your diet accordingly:
- Low Sodium Diet: For those experiencing gestational hypertension, a diet low in sodium can be beneficial.
- Hydration: Increase water intake to help reduce edema and maintain overall hydration.
- Fiber-Rich Foods: To combat constipation, which can be a concern in pregnancy, ensure a diet high in fiber.
Postpartum Nutrition
After delivery, the dietary focus shifts to healing and recovery:
- Nutrient-Rich Diet: Continue to consume a balanced diet rich in all essential nutrients to aid in recovery and, if breastfeeding, to support milk production.
- Caloric Needs: If breastfeeding, your caloric needs may be higher. Focus on nutrient-dense calories.
- Gradual Weight Loss: If weight loss is a goal post-pregnancy, aim for a gradual approach rather than rapid weight loss, especially if breastfeeding.
This section is designed to guide expectant mothers through each stage of pregnancy, providing specific nutritional advice tailored to the unique requirements of each trimester and postpartum period. It emphasizes the importance of a balanced diet and regular monitoring to manage gestational diabetes effectively while supporting the health and well-being of both mother and baby.
Building upon the trimester-specific dietary guidance, this section delves into the crucial aspects of physical activity, stress management, and overall wellness during pregnancy for mothers with gestational diabetes. This comprehensive approach aims to provide holistic care that goes beyond dietary management, addressing the physical and emotional well-being of expectant mothers.
Physical Activity and Wellness During Pregnancy
Physical Activity and Gestational Diabetes
Incorporating safe physical activity into your routine is essential for managing gestational diabetes:
- Recommended Exercises: Low-impact exercises like walking, swimming, and prenatal yoga are beneficial. They improve blood sugar control and overall well-being without overly straining the body.
- Exercise Guidelines: Aim for at least 150 minutes of moderate-intensity exercise per week. However, always consult with your healthcare provider before starting any new exercise routine.
- Monitoring During Exercise: Be aware of how your body and blood sugar levels respond to exercise. Adjust intensity and duration based on your comfort and medical advice.
Stress Management Techniques
Managing stress is crucial as it can impact blood sugar levels:
- Relaxation Practices: Techniques such as deep breathing, meditation, and mindfulness can help manage stress. Consider prenatal massages or acupuncture after consulting with your healthcare provider.
- Support Systems: Lean on support systems – family, friends, or support groups for expectant mothers. Sharing experiences and concerns can significantly reduce stress.
- Professional Counseling: If stress becomes overwhelming, consider speaking with a professional counselor who specializes in pregnancy and stress management.
Sleep and Rest
Adequate rest and good sleep quality are vital during pregnancy:
- Sleep Hygiene: Maintain a regular sleep schedule and create a comfortable, restful sleeping environment. Limit screen time before bed and consider relaxation techniques to improve sleep quality.
- Napping: Short naps can help combat fatigue, especially during the later stages of pregnancy when sleeping can be more challenging.
- Discuss Sleep Concerns: If you experience persistent sleep issues, discuss them with your healthcare provider. Conditions like sleep apnea can affect blood sugar control and may require medical intervention.
Preparing for Childbirth and Postpartum
The final stages of pregnancy should also include preparations for childbirth and the postpartum period:
- Childbirth Education Classes: These classes can provide valuable information on the birthing process, pain management techniques, and what to expect during labor and delivery.
- Postpartum Care Plan: Develop a postpartum care plan that includes considerations for your physical and emotional recovery, especially in managing gestational diabetes post-delivery.
- Breastfeeding Plans: If you plan to breastfeed, consider consulting a lactation specialist. Breastfeeding can impact blood sugar levels and dietary needs.
Emotional Wellness and Mental Health
Addressing emotional well-being is as important as physical health:
- Acknowledging Emotional Changes: Pregnancy can be an emotional rollercoaster. Acknowledge and accept these feelings as a normal part of the journey.
- Mental Health Check-Ins: Regular check-ins with yourself or a mental health professional can help in identifying any concerns, such as prenatal or postpartum depression.
- Building a Support Network: Cultivate a strong support network for emotional and practical support during pregnancy and after childbirth.
This section provides a holistic view of managing gestational diabetes, emphasizing the importance of physical activity, stress management, adequate rest, preparation for childbirth, and emotional wellness. It underscores the need for a comprehensive approach that addresses the physical, emotional, and mental health aspects of pregnancy, ensuring a healthier and more comfortable journey for expectant mothers with gestational diabetes.
Expanding further, this section emphasizes the importance of planning for postpartum recovery and long-term health, particularly for mothers who have experienced gestational diabetes. This comprehensive approach covers postnatal nutrition, physical recovery, mental health, and strategies to reduce the risk of future health complications.
Postpartum Recovery and Long-Term Health Planning
Postnatal Nutritional Care
After childbirth, nutrition continues to play a crucial role, especially for mothers who have had gestational diabetes:
- Balanced Diet for Recovery: The focus should be on a nutrient-rich diet that aids in healing and provides the energy needed for the demands of new motherhood.
- Breastfeeding Considerations: If breastfeeding, the nutritional intake needs to be adjusted to meet increased caloric and hydration needs. Prioritize foods rich in calcium, iron, and protein.
- Weight Management: Gradual weight loss through a balanced diet and regular physical activity is recommended. Avoid crash diets, especially if breastfeeding, as they can impact milk supply and quality.
Physical Recovery and Exercise
Physical recovery post-childbirth varies for each individual:
- Postpartum Exercise: Gradually reintroduce exercise into your routine, focusing initially on light activities like walking or pelvic floor exercises. Always get clearance from your healthcare provider before starting any postpartum exercise.
- Rest and Physical Health: Allow your body time to rest and recover. Pay attention to any signs of postpartum complications and seek medical advice as needed.
Mental Health and Emotional Well-being
The postpartum period can be challenging mentally and emotionally:
- Awareness of Postpartum Depression: Be aware of the signs of postpartum depression and seek help if you experience persistent sadness, anxiety, or mood swings.
- Self-Care: Prioritize self-care activities that promote relaxation and stress relief. This can include reading, taking baths, or engaging in hobbies.
- Support Networks: Maintain a strong support network. Connecting with other new mothers, either in person or through online forums, can provide valuable emotional support and shared experiences.
Reducing Future Health Risks
Having gestational diabetes increases the risk of certain health issues in the future:
- Regular Health Screenings: Schedule regular health check-ups, including blood sugar monitoring, to check for the development of type 2 diabetes or other health issues.
- Healthy Lifestyle: Continue to follow a healthy lifestyle, including a balanced diet and regular exercise, to reduce the risk of developing type 2 diabetes and other health conditions.
- Family Health Education: Educate your family about healthy living to encourage a supportive environment and reduce the risk of diabetes in children.
Long-Term Health Monitoring and Care
Long-term health monitoring is crucial for mothers who have had gestational diabetes:
- Ongoing Medical Consultations: Regular consultations with your healthcare provider are important to monitor your overall health and manage any arising health concerns.
- Awareness of Body Changes: Stay attuned to changes in your body and health, and do not hesitate to seek medical advice for any concerns.
- Lifestyle Adjustments as Needed: Be prepared to make lifestyle adjustments based on health assessments and medical advice.
This section focuses on the critical period following childbirth, addressing the need for comprehensive postpartum care and the importance of long-term health planning. It provides guidance on postnatal nutrition, physical and mental health recovery, strategies to reduce the risk of future health conditions, and the importance of ongoing health monitoring and care. This approach is designed to empower new mothers with the knowledge and resources needed for a healthy postpartum recovery and long-term well-being.
Moving towards the conclusion of our comprehensive guide, this section is dedicated to summarizing the key points and providing closure, encapsulating the journey from understanding and managing gestational diabetes during pregnancy to embracing a healthy postpartum life and future wellness.
Conclusion and Moving Forward: Embracing a Healthy Future
Recap of the Journey
Our journey through understanding and managing gestational diabetes has covered extensive ground:
- We began by demystifying gestational diabetes, understanding its implications during pregnancy and the importance of early diagnosis and monitoring.
- We navigated through the complexities of dietary management, emphasizing the balance of nutrients vital for both mother and baby, and tailored strategies for each trimester.
- The guide highlighted the importance of physical activity, stress management, and emotional wellness during pregnancy, underlining these as key components of a holistic approach to managing gestational diabetes.
- We delved into the postpartum phase, discussing nutritional care, physical and emotional recovery, and strategies for long-term health and wellness.
Embracing a Healthy Postpartum Life
The postpartum period is a time of recovery, adjustment, and new beginnings:
- Prioritize nutritional balance and physical well-being to aid recovery and meet the demands of motherhood, especially if breastfeeding.
- Acknowledge and address mental and emotional health, understanding that postpartum changes can be profound and seeking support when needed.
Planning for Long-Term Wellness
Gestational diabetes is not just a pregnancy-related condition; it’s a signal to prioritize long-term health:
- Maintain regular health screenings and medical consultations to monitor for potential development of type 2 diabetes or other related health issues.
- Continue practicing a healthy lifestyle—balanced diet, regular exercise, stress management, and emotional well-being—to reduce future health risks.
- Educate and involve your family in healthy living practices, fostering an environment that supports wellness for everyone.
Conclusion: A Journey of Empowerment and Health
As we conclude this guide, it’s important to recognize that managing gestational diabetes is more than just a temporary challenge—it’s an opportunity to embark on a path of health and wellness that extends far beyond pregnancy. The journey through gestational diabetes is unique for each individual, but the underlying goal remains the same: to ensure the best possible health outcomes for both mother and child.
Remember, you are not alone on this journey. Leverage the support of healthcare professionals, family, friends, and support networks. Embrace the learning and changes with a positive outlook, and view them as stepping stones to a healthier future.
In closing, take pride in the strength and resilience you’ve shown in managing gestational diabetes. Let this experience be a catalyst for continued health and wellness, not just for yourself, but for your entire family. Here’s to a healthy, empowered, and vibrant life ahead!
This concluding section wraps up the guide, offering a recap of the journey and emphasizing the importance of continued health and wellness post-gestational diabetes. It serves to inspire and motivate expectant and new mothers, reinforcing the message of empowerment, support, and long-term health commitment.
FAQs: Managing Diabetes Diet During Pregnancy
- What is gestational diabetes and how is it different from other types of diabetes?
Gestational diabetes is a form of diabetes that occurs during pregnancy and typically resolves after childbirth. Unlike Type 1 or Type 2 diabetes, it’s primarily caused by hormonal changes during pregnancy that affect insulin effectiveness. - When are women usually tested for gestational diabetes?
Women are generally tested for gestational diabetes between the 24th and 28th weeks of pregnancy. However, if there are high-risk factors, such as a family history of diabetes or previous gestational diabetes, testing may be done earlier. - Can I still have a healthy pregnancy with gestational diabetes?
Absolutely. Many women with gestational diabetes have healthy pregnancies and babies. It requires careful monitoring of blood sugar levels, a balanced diet, and regular physical activity. - What kind of diet should I follow if I have gestational diabetes?
Focus on a balanced diet rich in complex carbohydrates, fiber, lean proteins, and healthy fats. Avoid foods high in simple sugars and saturated fats. Portion control and meal timing are also important to manage blood sugar levels. - Are there any physical activities that are safe during pregnancy with gestational diabetes?
Yes, activities like walking, swimming, and prenatal yoga are generally safe and beneficial. However, it’s important to consult with your healthcare provider before starting any exercise routine. - How can gestational diabetes affect my baby?
Unmanaged gestational diabetes can lead to complications such as higher birth weight, premature delivery, and increased risk for breathing and other problems at birth. Long-term, it can increase the child’s risk of developing obesity and type 2 diabetes. - What happens to gestational diabetes after childbirth?
Gestational diabetes usually resolves after childbirth. However, it’s important to get tested for diabetes postpartum as there’s an increased risk of developing type 2 diabetes later in life. - How can I manage my emotional well-being while dealing with gestational diabetes?
Managing emotional well-being involves stress reduction techniques like meditation or yoga, seeking support from family, friends, or support groups, and if needed, professional counseling. - Will I need medication to manage gestational diabetes?
Not everyone will require medication. Many women manage gestational diabetes through diet and exercise alone. However, some may need medication or insulin therapy as prescribed by their healthcare provider. - Can gestational diabetes be prevented?
While not all cases can be prevented, maintaining a healthy weight, eating a balanced diet, and regular exercise before and during pregnancy can reduce the risk of developing gestational diabetes.
Blog Tags:
gestational diabetes, pregnancy nutrition, diabetes diet, healthy pregnancy, prenatal care, postpartum recovery, blood sugar management, pregnancy exercise, emotional wellness during pregnancy, long-term health after pregnancy