Why You Should Care, Even If You Don’t Have Gout
Introduction: The Surprising Truth About Uric Acid
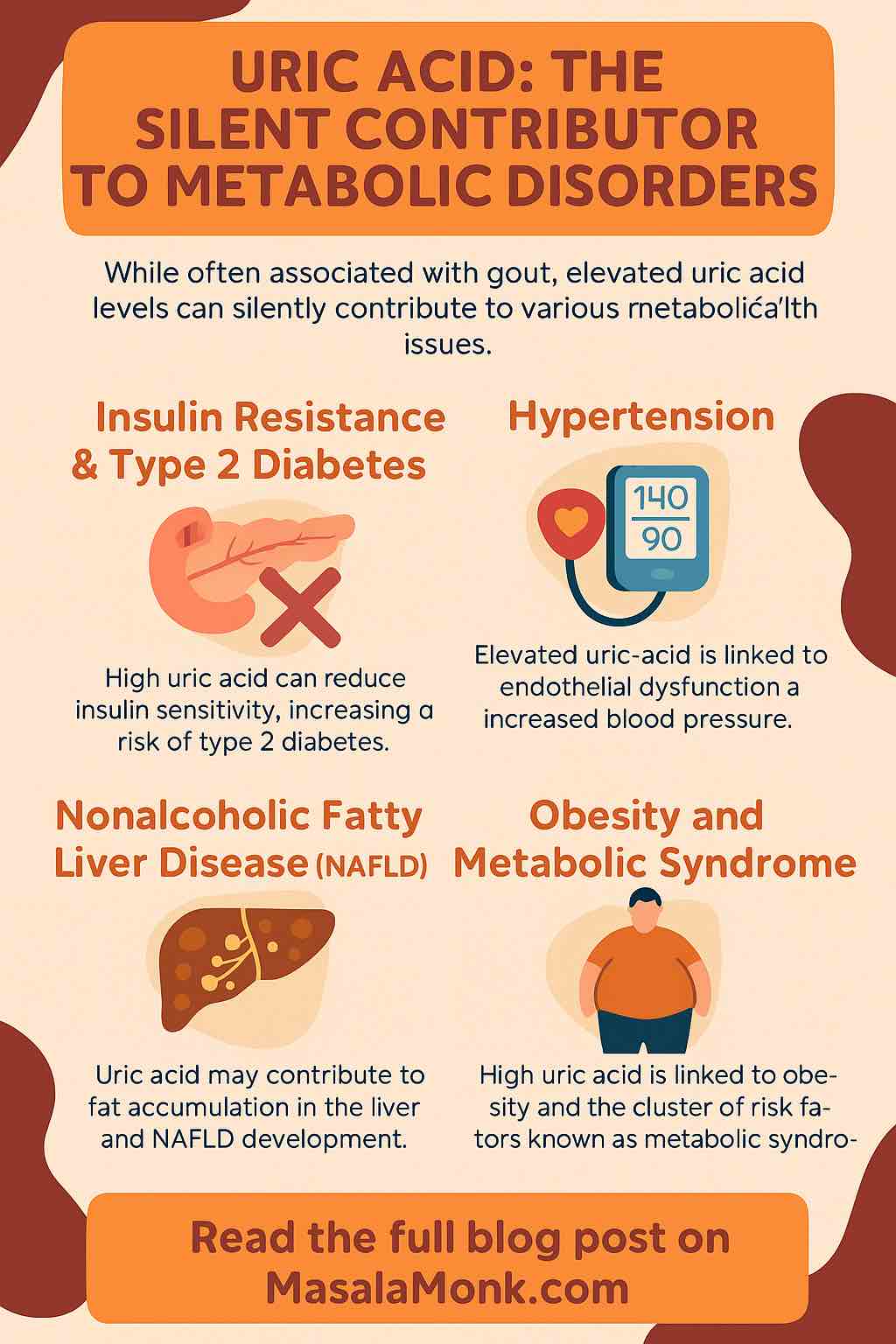
When you hear “uric acid,” you probably think of gout—the painful swelling in your big toe or joints that’s almost become a punchline in medical sitcoms. But what if I told you that uric acid is much more than just the “gout chemical?” What if it’s quietly contributing to some of the world’s most serious health problems—like diabetes, high blood pressure, fatty liver disease, and heart attacks—even in people who never develop gout?
Let’s dig deeper into the science, bust some myths, and discover practical steps you can take today to protect your metabolic health.
Section 1: What is Uric Acid, Really?
Uric acid is a natural waste product. Every day, as your body breaks down purines (building blocks of DNA found in your cells and certain foods), uric acid is created in your blood. Normally, your kidneys filter it out and you excrete most of it in your urine.
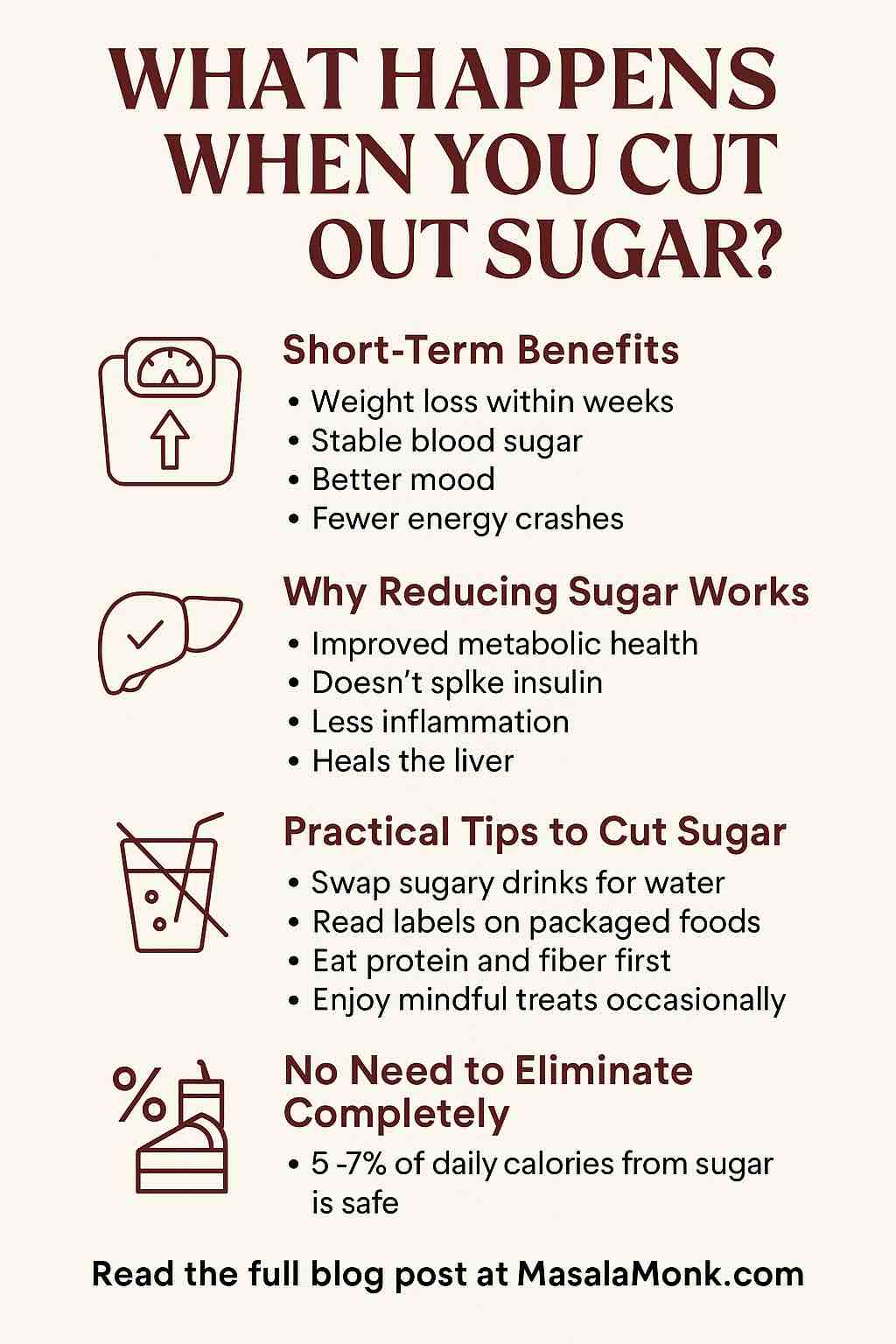
But in modern life, with our sugar-loaded drinks, processed foods, and sedentary lifestyles, many people produce more uric acid than their bodies can remove. This leads to hyperuricemia—chronically elevated uric acid levels, even if you feel perfectly fine.
Quick Fact: You can have high uric acid and no gout symptoms for years. But “silent” damage may still be happening in your body.
Section 2: How Uric Acid Silently Damages Your Metabolic Health
1. Insulin Resistance and Type 2 Diabetes
Research now shows uric acid does more than just float in your blood. At high levels, it interferes with insulin’s ability to help your cells take in sugar. Over time, this leads to insulin resistance, the root of type 2 diabetes.
How?
- Uric acid reduces the production of nitric oxide, which is vital for healthy blood vessels and proper insulin function.
- It increases inflammation and oxidative stress, damaging cells from the inside out.
2. Hypertension (High Blood Pressure)
Did you know that high uric acid can raise your blood pressure—sometimes even before your cholesterol or sugar numbers go bad?
- Uric acid makes your blood vessels stiff and narrow.
- It triggers the “renin-angiotensin” system, a hormonal process that increases blood pressure.
3. Fatty Liver Disease (NAFLD)
Even if you don’t drink alcohol, you could be at risk for nonalcoholic fatty liver disease (NAFLD). Uric acid increases the amount of fat stored in liver cells and promotes inflammation, making your liver sluggish and sick.
4. Obesity and Metabolic Syndrome
It’s a vicious cycle:
- Obesity raises uric acid.
- Uric acid increases inflammation and makes it easier for your body to store fat, especially around your belly.
- This cluster of risks—obesity, high blood pressure, high sugar, and abnormal cholesterol—is known as metabolic syndrome.
5. Heart Disease
Chronic high uric acid doesn’t just stop at diabetes and hypertension—it quietly increases your risk for heart attacks and strokes.
Section 3: Why Is Uric Acid So Easily Overlooked?
Doctors have long focused on uric acid only when it causes gout or kidney stones. But modern research shows even “high-normal” levels (well below the gout threshold) can drive chronic disease. In fact, studies suggest we might be missing opportunities to prevent major illnesses by ignoring uric acid until symptoms appear.
Tip: You don’t need gout to be harmed by high uric acid.
Section 4: How Do You Know If Your Uric Acid Is High?
A simple blood test called serum urate measures your level.
- Normal range: Roughly 3.5–7.2 mg/dL (may vary by lab and gender).
- Concerning: Many experts now think risks increase above 5.5–6 mg/dL, especially if you have other risk factors.
Ask your doctor to check your uric acid level—especially if you have high blood pressure, abnormal blood sugar, or fatty liver.
Section 5: What Raises Uric Acid? (And How You Can Lower It)
Dietary Factors That Raise Uric Acid:
- Sugary Drinks: Especially those with fructose (soda, fruit juices, energy drinks).
- Alcohol: Beer and spirits are particularly risky.
- High-purine Foods: Red meats, organ meats (liver, kidney), anchovies, sardines, and some seafood.
- Processed Foods: Chips, pastries, and anything high in added sugar.
Lifestyle Risks:
- Being overweight or obese.
- Chronic dehydration.
- Sedentary lifestyle.
- Certain medications (diuretics, aspirin).
Practical Steps to Lower Uric Acid and Protect Your Metabolic Health
1. Rethink Your Drinks
- Replace sugary beverages with water, unsweetened tea, or black coffee.
- Limit alcohol, especially beer.
2. Choose Wisely at Mealtime
- Go for lean proteins: eggs, chicken, tofu, legumes.
- Eat more vegetables, whole grains, and healthy fats (avocado, nuts, olive oil).
- Limit red meat and processed snacks.
3. Move More
- Regular physical activity improves uric acid clearance and insulin sensitivity.
- Even daily brisk walks can help.
4. Maintain a Healthy Weight
- Losing just 5–10% of your weight can significantly lower uric acid and improve all aspects of metabolic health.
5. Stay Hydrated
- Drinking enough water helps flush uric acid through your kidneys.
6. Review Your Medications
- Ask your doctor if any of your meds may be increasing uric acid, and if alternatives exist.
Section 6: The Future—Will We Treat Metabolic Syndrome by Targeting Uric Acid?
Exciting new research is underway. Early trials show that uric acid–lowering drugs (like allopurinol) may help reduce blood pressure, improve insulin sensitivity, and protect the liver—even in people with no gout. But more large-scale studies are needed before these become standard care.
Section 7: When to Seek Medical Advice
- If you have a family history of gout, heart disease, diabetes, or fatty liver.
- If you already have high blood pressure, prediabetes, or abnormal cholesterol.
- If you experience joint pain or sudden swelling, especially in your big toe.
Don’t wait for pain—get checked, get informed, and take action early.
Conclusion: Uric Acid—From Afterthought to Metabolic Villain
Uric acid isn’t just about gout. It’s a powerful, underappreciated force in modern metabolic disease. By paying attention to your diet, staying active, and getting regular check-ups, you can keep uric acid in check—and give yourself the best shot at a healthier, longer life.
Takeaway:
Ask for a uric acid test. Rethink your sugary drinks. Move your body daily. Your future self will thank you!
FAQs: Uric Acid and Metabolic Disorders
1. What is uric acid and why does it matter?
Uric acid is a waste product formed when your body breaks down purines from food and cell turnover. While it’s usually excreted in urine, high levels can silently contribute to metabolic problems—even if you never get gout.
2. What is considered a high uric acid level?
Generally, a blood uric acid level above 6 mg/dL (women) or 7 mg/dL (men) is considered high, but research shows that risks for metabolic disorders may rise even at lower “high-normal” levels.
3. Can I have high uric acid without any symptoms?
Yes. Most people with elevated uric acid have no symptoms until they develop gout or kidney stones. Meanwhile, silent damage to your metabolism, blood vessels, and liver may still occur.
4. How does uric acid cause insulin resistance or diabetes?
High uric acid interferes with insulin’s action and promotes inflammation and oxidative stress, which contribute to insulin resistance—a precursor to type 2 diabetes.
5. What foods increase uric acid the most?
Sugary drinks (especially those with fructose), red meat, organ meats, shellfish, and alcoholic beverages (especially beer) are top offenders. Processed foods and dehydration also play a role.
6. Are there foods that help lower uric acid?
Yes! Cherries, coffee (in moderation), low-fat dairy, whole grains, and plenty of water can help. Fruits and vegetables (except high-purine ones like asparagus and spinach, which are less impactful than animal sources) are beneficial.
7. Does losing weight help lower uric acid?
Absolutely. Losing even 5–10% of your body weight can significantly reduce uric acid and improve overall metabolic health.
8. Should I ask my doctor to test my uric acid even if I feel fine?
If you have risk factors like obesity, high blood pressure, fatty liver, family history of gout, or prediabetes, it’s wise to get your uric acid checked—even without symptoms.
9. Can medications help lower uric acid and improve metabolic health?
Yes, certain medications (like allopurinol and febuxostat) are used for gout and can lower uric acid. Emerging evidence suggests they may also help with blood pressure, insulin resistance, and liver health, but more studies are needed for people without gout.
10. How quickly can lifestyle changes lower uric acid?
Positive changes—like improving diet, increasing water intake, and moving more—can lower uric acid in a matter of weeks to months. Consistency is key for long-term benefits.