When you think of diabetes-friendly foods, okra (also known as bhindi or lady’s finger) may not be the first vegetable that comes to mind. Yet, this humble, mucilaginous pod is fast gaining attention in both kitchens and scientific circles for its potential to help manage blood sugar. With a growing body of new research, okra’s role in diabetes care is no longer just folk wisdom—it’s increasingly evidence-based.
But is okra really effective for people with diabetes? How should you use it? What do clinical trials say, and are there any cautions to keep in mind?
Let’s dig into the science, bust myths, and share practical tips you can use starting today.
Why is Okra Suddenly in the Spotlight for Diabetes?
Okra is a nutritional powerhouse: low in calories, rich in soluble fiber, antioxidants, vitamins C and K, folate, and a unique mix of plant compounds called polysaccharides and flavonoids. In India, it’s long been part of traditional remedies for blood sugar, but only recently have rigorous clinical trials started to confirm what folk medicine suspected.
What Does the Latest Research Say? (2024–2025 Highlights)
1. Okra Can Lower Blood Sugar—Especially Fasting Glucose
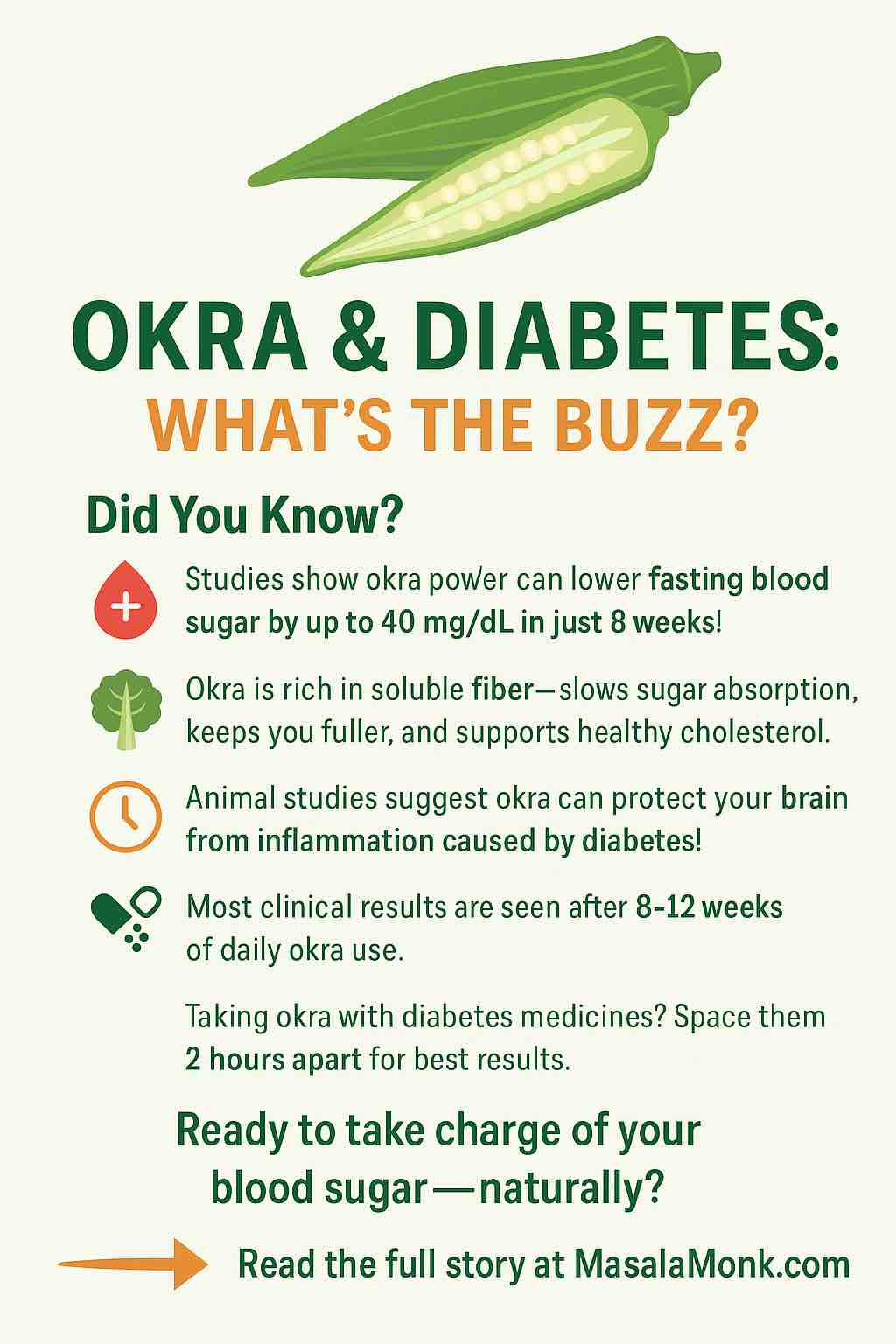
A meta-analysis published in December 2024 (analyzing 9 clinical trials and over 500 people) found that okra supplementation—mainly as powdered pods—led to:
- A significant reduction in fasting blood glucose (FBG) by an average of ~40 mg/dL after at least 8 weeks of use.
- HbA1c (a long-term blood sugar marker) fell by about 0.4–0.5% in studies lasting over 2 months.
2. It Improves Lipids—And May Reduce Inflammation
The same review and several others in early 2025 found modest but meaningful improvements in cholesterol—especially total cholesterol (TC) and LDL (“bad” cholesterol). There’s also evidence for reduced inflammation, as seen by falling CRP (C-reactive protein) levels in clinical participants.
3. New Clues on How Okra Works
The benefits of okra aren’t magic—they’re rooted in science:
- High Soluble Fiber: The famous “slime” in okra slows carbohydrate absorption, preventing sugar spikes after meals.
- Polysaccharides & Flavonoids: Unique plant chemicals in okra help improve insulin sensitivity and support pancreatic cell health.
- Animal Studies: Okra’s compounds reduce brain inflammation and protect against obesity-related damage, suggesting benefits for both metabolism and brain health.
4. Short-Term vs. Long-Term Effects
A March 2025 trial found that short-term okra supplementation (2 months) increased insulin levels and insulin resistance (HOMA-IR)—without a big drop in blood sugar. This suggests that while the body is producing more insulin initially, it might take longer (8–12+ weeks) to see sustained improvements in blood glucose.
5. Okra Is Safe—But Interactions Are Possible
Most studies show no significant side effects, even when taken as a supplement. However, the thick mucilage may reduce absorption of oral diabetes drugs like metformin if taken together. Experts suggest separating your okra supplement/meal and medication by at least 2 hours.
How to Use Okra for Diabetes—Practical Guidance
What do the studies use?
- Most use 1–3 grams of okra pod powder daily, divided into two or three doses.
- Some use fresh okra (steamed, sautéed, or as “okra water”), but powders and capsules are easier for standardization.
Okra Water: The Home Remedy
One of the most popular home hacks—especially in India and Nigeria—is “okra water.”
How to make it:
- Wash and slice 2–4 medium okra pods lengthwise.
- Soak overnight in a glass of water (room temperature).
- In the morning, squeeze the pods to release the slime, discard them, and drink the water before breakfast.
Note: While this method is popular, clinical trials use dried powder for dose accuracy.
Okra Powder or Capsules: The Research Way
If you prefer supplements:
- Look for pure okra pod powder—check that there are no added sugars or fillers.
- Start with 1 gram (about ½ teaspoon) twice a day, increasing slowly to 3 grams total if tolerated.
- Take it 1–2 hours apart from other oral medications.
Culinary Okra: Delicious and Diabetic-Friendly
Okra is easy to include in daily meals:
- Sautéed Bhindi: Toss sliced okra with onions, tomatoes, and spices.
- Okra in Sambar: Adds texture to South Indian lentil stews.
- Roasted Okra: Cut pods, season, and roast for a crispy snack.
Cooking tip: Cooking reduces sliminess—if you dislike the texture, try dry-roasting or grilling.
Who Should Avoid Okra or Use Caution?
- Those with kidney stones: Okra is high in oxalates, which may worsen kidney stone risk.
- People on metformin or other oral diabetes drugs: Take okra and medication at least 2 hours apart to avoid absorption issues.
- Allergic reactions: Rare, but possible—start with a small dose.
Can Okra Replace My Diabetes Medications?
Absolutely not. Okra is best seen as a complementary tool—not a substitute for prescribed medications or healthy lifestyle changes. Think of it like adding a new member to your diabetes-fighting team: it works best with good nutrition, regular movement, and medical guidance.
What Are the Research Gaps and Next Steps?
While new studies are promising, researchers say:
- Larger, longer trials (6+ months) are needed, especially on HbA1c and real-world outcomes.
- Standardized dosing (pod powder vs. seed extract, fresh vs. dried) needs more study.
- Impact on brain health and diabetes complications is a new area of research—watch this space!
Frequently Asked Questions (FAQ)
1. Can okra really help lower blood sugar in diabetes?
Yes, multiple clinical studies show that regular okra intake—especially powdered okra pod—can significantly lower fasting blood sugar (FBG) and modestly reduce HbA1c when used for at least 8 weeks. However, it is most effective as an adjunct to, not a replacement for, standard diabetes treatments.
2. How much okra should I take for diabetes management?
Most research uses 1–3 grams of okra pod powder per day, split into two or three doses. For “okra water,” people often soak 2–4 pods overnight and drink the water in the morning. Always start low and monitor for side effects.
3. Which is more effective—okra powder, capsules, or okra water?
Clinical trials mainly use powdered okra pod, which provides a standardized dose. Okra water is popular but less consistent in dose. Capsules are convenient if they contain pure okra powder.
4. How soon can I expect results after starting okra?
Most studies report noticeable changes in fasting blood sugar and cholesterol after 8–12 weeks of consistent use.
5. Can I use okra if I am on diabetes medications like metformin or sulfonylureas?
Yes, but okra’s high fiber content may slow absorption of some oral medications. It’s best to take okra at least 2 hours apart from your medicines. Consult your healthcare provider before starting.
6. Are there any side effects or risks of using okra?
Okra is generally safe. Rarely, it may cause digestive upset (bloating, gas) or allergic reactions. Because it’s high in oxalates, people prone to kidney stones should use caution.
7. Will okra help with cholesterol or heart health?
Yes, recent studies show that okra can lower total and LDL (“bad”) cholesterol. This makes it a heart-friendly food choice, especially for people with diabetes.
8. Is okra safe for children or pregnant women with diabetes?
There’s little clinical data for children or pregnant women. While dietary okra is generally safe, supplements or large doses should be avoided without medical advice.
9. Can eating cooked okra in meals give the same benefits as supplements?
Cooking and eating okra as part of regular meals provides fiber and antioxidants. While the clinical effects may not be as potent as standardized powder doses, it still supports blood sugar control and overall health.
10. Should I stop my diabetes medication if my blood sugar improves after using okra?
No. Never stop or change any prescribed medication without your doctor’s guidance. Okra is best used as a complementary approach to your existing diabetes care plan.
The Takeaway
Okra isn’t just a crunchy side dish or slimy veggie—it’s a science-backed, practical tool to help lower fasting blood sugar, improve cholesterol, and possibly protect your brain. For people living with diabetes, adding okra to the menu (or taking it as a supplement) could be a smart, safe, and tasty move—especially when combined with medical advice.
“Let food be thy medicine,” Hippocrates said. Okra might just be the new-old example the world needs.
Ready to Try Okra?
- Start with a daily okra dish or morning okra water.
- If using supplements, opt for pure pod powder and check with your healthcare provider—especially if you take other medications.
- Stay tuned for more research—and let your plate be part of the solution!
References
- Frontiers in Nutrition, 2024
- Bohrium Clinical Trial, 2025
- NDTV – Okra & Brain Health, 2025
- Examine.com Meta-analysis
- VeryWell Health – Okra Water
Have you tried okra for your health? Share your experiences or questions below!