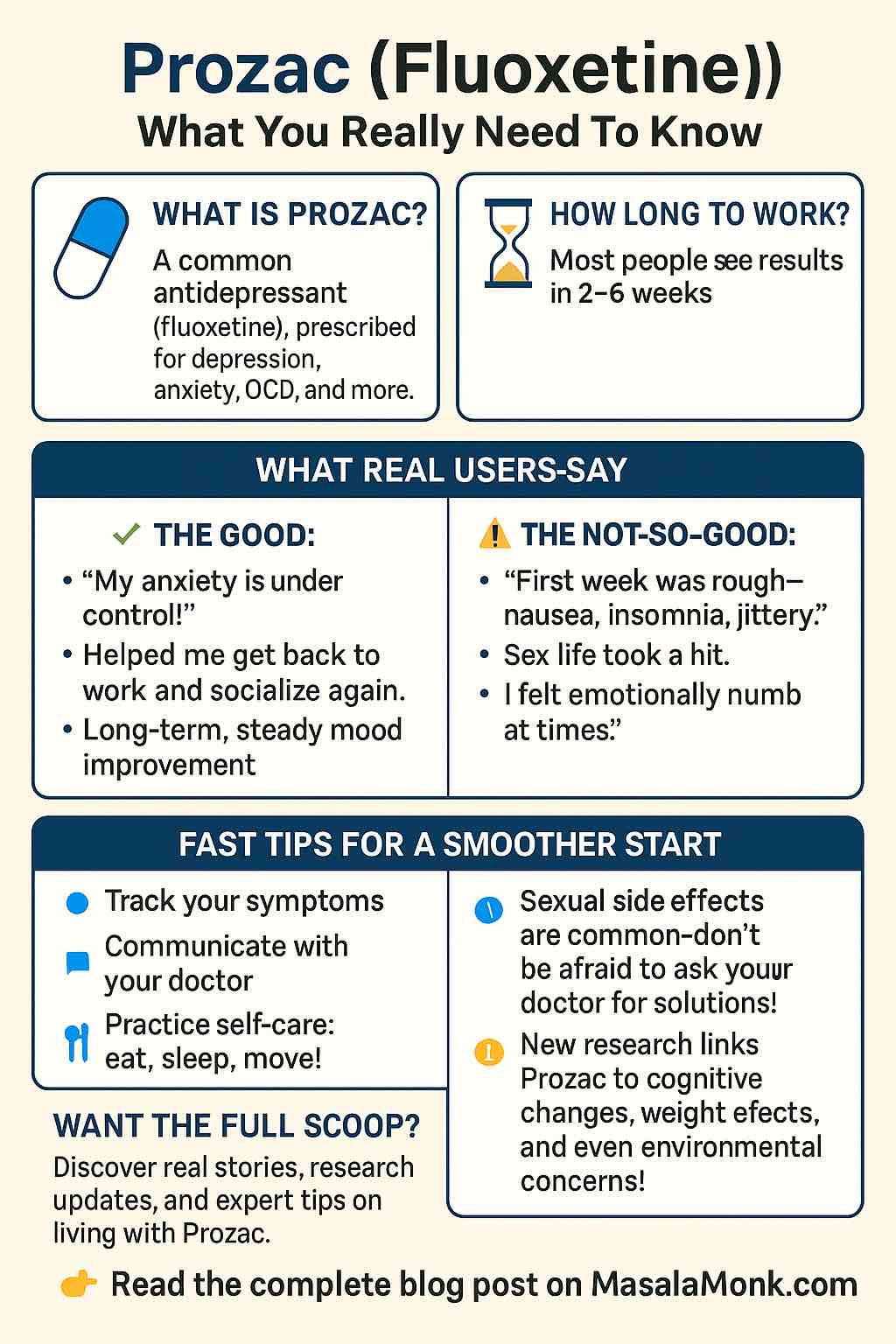
Prozac, also known by its generic name fluoxetine, is a name that comes up often in conversations about mental health. As one of the most widely prescribed antidepressants since the late 1980s, Prozac has helped millions manage depression, anxiety, OCD, and more. But beyond the clinical descriptions, what is it really like to live with Prozac? What do research and real user experiences tell us about the benefits, side effects, and practical tips for getting the most out of this medication?
Let’s dig deep—from the science to the stories.
Understanding Prozac: How Does It Work?
Prozac is an SSRI (Selective Serotonin Reuptake Inhibitor). In plain language, it increases the amount of serotonin available in the brain—a chemical often linked to mood, well-being, and emotional balance. Doctors prescribe Prozac for:
- Major Depressive Disorder
- Anxiety Disorders
- Obsessive-Compulsive Disorder (OCD)
- Panic Disorder
- Bulimia Nervosa
- Premenstrual Dysphoric Disorder
But while the “how” of Prozac seems simple, the “what happens next” can be complex and varies for each individual.
Starting Prozac: What Real Users Say
Most people start Prozac with hope and some trepidation. Real user experiences from Drugs.com and WebMD reveal a pattern:
- First Week(s): Some users feel a spike in anxiety or insomnia. It’s not unusual to experience nausea, loss of appetite, headache, or gastrointestinal upset.
- Weeks 3–6: This is where many report a shift. The “cloud” begins to lift, and energy returns. Those who stick it out past the bumpy start often find benefits emerging steadily.
- Tip: Take Prozac in the morning if you notice sleep trouble. With food, if nausea is an issue.
“The first week was rough—I felt jittery and slept badly. But by week four, my anxiety had lessened, and I felt like myself again for the first time in years.”
— Real User Review
Benefits Beyond the Brochure
Fluoxetine isn’t just about fighting depression; it’s also credited with:
- Regaining social confidence: Users often describe a renewed ability to interact, socialize, and leave the house after months (or years) of isolation.
- Reducing panic attacks: Many with panic disorder report dramatic drops in the frequency and severity of attacks.
- Long-term stability: For some, Prozac is the steady hand on the tiller, keeping their mood on course year after year.
But it’s not all positive, and honest stories matter.
Side Effects: The Good, the Bad, and the Manageable
Common (Usually Early) Side Effects:
- Nausea
- Headache
- Sleep changes (insomnia or sleepiness)
- Loss of appetite or mild weight loss
- Dry mouth
- Sweating
- Dizziness
These often subside after a few weeks. If not, or if they’re severe, tell your doctor.
Sexual Side Effects (A Real Concern):
- Decreased libido
- Difficulty achieving orgasm (anorgasmia)
- Erectile dysfunction
This group of side effects is especially persistent. Some report that sexual dysfunction continues even after stopping Prozac—a phenomenon called Post-SSRI Sexual Dysfunction (PSSD). If this is a major concern, discuss options with your doctor. Sometimes, adjusting the dose, changing the timing, or adding another medication (like bupropion) can help.
“My mood was better, but my sex life disappeared. For me, that was a deal-breaker.”
— Real User Review
Mood Shifts and Emotional Blunting
Some users describe feeling “emotionally numb” or less able to cry or feel strong joy. While this can make negative emotions more bearable, it sometimes dulls positive feelings too. If emotional blunting becomes a problem, consult your provider—it may be possible to tweak your medication plan.
Rare but Serious Risks:
- Suicidal thoughts (especially in teens/young adults)
- Serotonin Syndrome (restlessness, confusion, fever, muscle rigidity—seek medical help immediately)
- QT prolongation and heart rhythm problems
- Seizures (rare, but higher risk if you have a seizure disorder)
- Hyponatremia (low blood sodium, mostly in older adults—watch for confusion, weakness, or seizures)
The Science: What’s New in 2024–2025?
Recent studies and clinical trials reveal new wrinkles:
- Cognitive impact: Research in 2024 suggests Prozac can improve cognitive function for people with depression or anxiety, but in healthy individuals, it may impair attention or memory. The effect is subtle and varies.
- Weight effects: Some studies show Prozac may help with weight loss or prevent weight gain, possibly by affecting fat cell metabolism. This effect is not universal.
- Environmental concerns: Prozac is now showing up in waterways, affecting fish and aquatic ecosystems. One study found male guppies exposed to Prozac had lower sperm vitality and altered behavior.
- Novel uses: Ongoing trials are testing Prozac for conditions like refractory constipation and even exploring neuroprotective properties for Alzheimer’s disease—but these uses aren’t yet standard.
Tips for Making Prozac Work for You
- Give It Time: SSRIs take time. Most people see improvement within 4–6 weeks. Don’t quit too soon.
- Track Your Symptoms: Keep a mood journal or use an app. Note side effects, mood changes, sleep, and energy.
- Communicate: Be honest with your provider about side effects and your quality of life. Adjustments can make a big difference.
- Lifestyle Counts: Good sleep, regular meals, and exercise can boost your recovery. Don’t rely solely on medication.
- Monitor for Interactions: Let your doctor know about all supplements and medications you’re taking. Prozac interacts with many drugs, especially other antidepressants, painkillers (like tramadol), blood thinners, and migraine medications.
- Don’t Stop Abruptly: Prozac’s long half-life makes withdrawal symptoms rare, but stopping suddenly can still cause problems. Taper off under medical supervision.
When Prozac Isn’t Right
Prozac is not for everyone. Some people experience only side effects, or their mood doesn’t improve. Others might find a different SSRI, SNRI, or non-SSRI antidepressant works better. That’s not a failure—it’s a step closer to what will work for you.
Real-Life FAQs
How do I know if Prozac is working?
You should notice an improved mood, better sleep, more motivation, or less anxiety. It’s subtle—a gradual lifting, not a sudden high.
Is it normal to feel worse before better?
Yes. Many users experience a spike in anxiety or low mood in the first two weeks before improvements start.
Can I drink alcohol?
It’s best to avoid alcohol, especially early on, as it can worsen side effects and reduce Prozac’s effectiveness.
Will Prozac change my personality?
You’ll still be you, but hopefully less burdened by depression or anxiety. Emotional blunting is possible for some; if it’s bothersome, discuss it with your doctor.
The Bottom Line
Prozac (fluoxetine) has helped millions find their way out of depression and anxiety, but the journey is not without bumps. The key is patience, communication, and customization—and remembering that your experience is unique. If you’re considering Prozac, talk openly with your provider, know what to expect, and trust that finding the right treatment is a process, not a single decision.
Have you taken Prozac? What was your experience? Share your story in the comments below—your voice could help someone else on their path.
Disclaimer: This blog is for educational purposes and does not replace professional medical advice. Always consult your healthcare provider before making changes to your medication.
10 Prozac (Fluoxetine) FAQs
1. How long does Prozac take to work?
Most people begin to notice improvements within 2–4 weeks, with full effects often seen at 6–8 weeks. Don’t be discouraged if you don’t feel better right away—it’s common for benefits to appear gradually.
2. What are the most common side effects, and do they go away?
The most common early side effects include nausea, headache, insomnia, fatigue, dry mouth, and sometimes increased anxiety. These typically subside after 1–3 weeks. If they persist or are severe, talk to your healthcare provider.
3. Will Prozac affect my sex life?
Many people report sexual side effects such as decreased libido, difficulty achieving orgasm, or erectile dysfunction. These effects can persist and, in rare cases, continue after stopping Prozac. Discuss options with your doctor if this becomes a problem.
4. Is it safe to take Prozac with other medications or supplements?
Prozac interacts with many drugs—including other antidepressants, painkillers (like tramadol), migraine meds, blood thinners, and some supplements (like St. John’s Wort). Always inform your provider about everything you’re taking to avoid dangerous interactions.
5. Can Prozac make anxiety or depression worse before it gets better?
Yes, it’s not uncommon to experience increased anxiety, agitation, or low mood in the first 1–2 weeks before improvement begins. If symptoms become severe, especially thoughts of self-harm, seek medical help immediately.
6. Should I take Prozac in the morning or evening?
Most people take Prozac in the morning to avoid insomnia, but if it makes you drowsy, evening might be better. Adjust the timing to suit your response, and check with your doctor.
7. What should I do if I miss a dose?
Take the missed dose as soon as you remember, unless it’s almost time for your next dose. Don’t double up. Missing one dose is rarely a problem due to Prozac’s long half-life, but regularity is best for effectiveness.
8. Is it safe to drink alcohol while on Prozac?
Alcohol can increase side effects like drowsiness, dizziness, and impair judgment. It may also worsen depression or anxiety. It’s best to limit or avoid alcohol while taking Prozac.
9. Can I stop Prozac suddenly if I feel better?
No—don’t stop Prozac abruptly. Even though withdrawal is less common than with other antidepressants, stopping suddenly can cause mood changes or other symptoms. Always taper under a doctor’s supervision.
10. Who should avoid Prozac or use it with caution?
People with a history of bipolar disorder, seizure disorders, bleeding problems, or certain heart conditions (like long QT syndrome) should use Prozac cautiously. It may not be suitable during pregnancy or breastfeeding—always discuss risks and benefits with your provider.