Ashwagandha, also known as Withania somnifera, has surged in popularity over recent years as a powerful adaptogen—herbs that help the body resist stress and promote overall balance. From boosting energy and reducing anxiety to enhancing cognitive function, this ancient Ayurvedic herb has been embraced worldwide. But with the rise in use, questions about its safety and side effects, especially concerning heart health and mental well-being, have come into sharper focus.
In this deep dive, we explore the latest scientific research from 2024 and beyond to give you a clear, evidence-based understanding of ashwagandha’s potential benefits and risks—particularly for your heart and mind.
What Is Ashwagandha?
Before diving into side effects, it helps to understand what makes ashwagandha special. Traditionally used in Ayurvedic medicine for thousands of years, ashwagandha is revered for its ability to:
- Lower stress hormones like cortisol
- Support immune function
- Improve energy and stamina
- Enhance memory and cognition
Modern research validates many of these claims, showing that ashwagandha’s bioactive compounds—like withanolides—have anti-inflammatory, antioxidant, and neuroprotective effects.
The Heart of the Matter: Ashwagandha and Cardiovascular Health
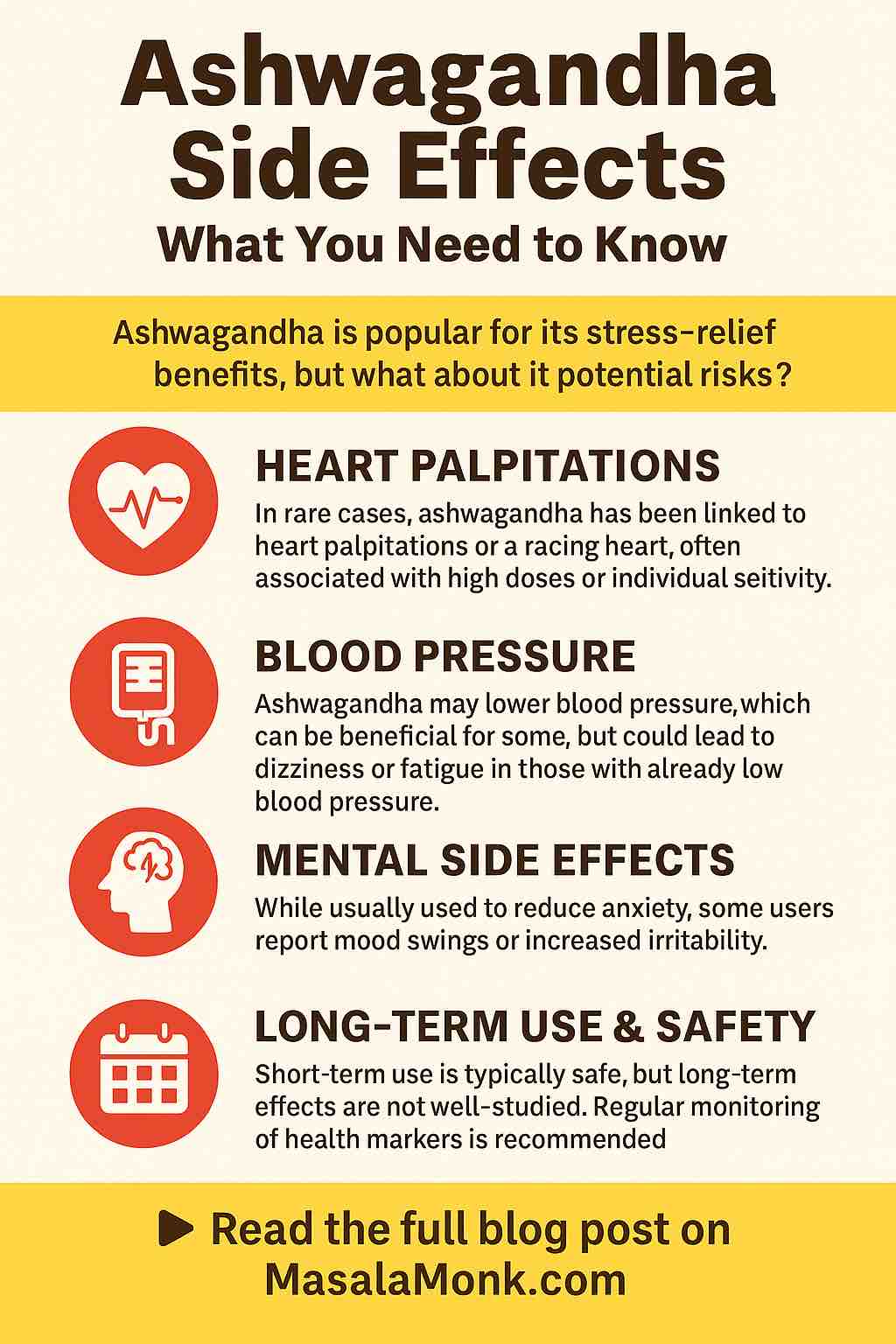
Can Ashwagandha Cause Bradycardia or Palpitations?
One of the most frequently searched concerns around ashwagandha is its impact on heart rhythm and rate—terms like bradycardia (abnormally slow heart rate) and palpitations (irregular or rapid heartbeat) often come up. Here’s what the latest evidence says:
- Bradycardia:
While ashwagandha can promote relaxation by calming the nervous system, clinically significant bradycardia is rarely reported. Some animal studies show that ashwagandha mildly lowers heart rate by enhancing parasympathetic (rest-and-digest) activity, but this does not translate to dangerous slowing in most healthy adults. - Palpitations:
Occasional reports of heart palpitations exist but are very rare. They tend to be anecdotal and often linked to either high doses or sensitivity in certain individuals. It’s possible that some commercial products might contain impurities or stimulants causing these symptoms rather than the herb itself.
What About Blood Pressure?
Ashwagandha is often praised for its blood pressure–lowering effects:
- Multiple clinical studies have shown that ashwagandha can reduce both systolic and diastolic blood pressure, especially in people with elevated baseline values or stress-induced hypertension.
- However, this hypotensive effect means that people already taking blood pressure medication or those with naturally low blood pressure should exercise caution. Combining ashwagandha with other blood pressure–lowering agents may cause excessive drops in pressure, leading to dizziness or fainting.
Should You Be Concerned About Ashwagandha and Heart Health?
For most people, ashwagandha is heart-safe when used at recommended doses. However, those with underlying heart conditions, arrhythmias, or on cardiac medications should consult their healthcare provider before starting ashwagandha supplements.
Mental Side Effects: More Than Just Calm
Ashwagandha is widely used for its anxiety-reducing and mood-stabilizing properties, but what about negative mental side effects?
Anxiety and Stress Reduction
A comprehensive meta-analysis published in 2024 reviewed nine clinical trials involving over 500 participants and found that ashwagandha significantly lowered perceived stress and serum cortisol levels. Most people experience a calmer, more relaxed state without sedation.
Mood Swings and Irritability
Despite these benefits, a small number of users report mood swings or irritability after taking ashwagandha. These effects are generally:
- Mild and transient
- More likely with higher doses
- Possibly related to individual brain chemistry or interactions with other medications, such as antidepressants or thyroid drugs
Cognitive Function
Emerging studies hint that ashwagandha might support memory and cognitive function, but the evidence is still preliminary. More robust clinical trials are needed to confirm these cognitive benefits and rule out potential side effects such as brain fog or sedation.
Common Side Effects: What to Expect
Most ashwagandha users tolerate the herb well, but some mild side effects can occur:
- Gastrointestinal upset (nausea, diarrhea, stomach discomfort)
- Drowsiness or sedation
- Allergic reactions (rare)
- Headache or dizziness (rare)
Rare but Serious: Liver and Thyroid Effects
Though uncommon, there are isolated case reports of:
- Liver injury: Some individuals, especially with preexisting liver conditions, have experienced elevated liver enzymes after taking ashwagandha. Monitoring liver function during long-term use is prudent.
- Thyroid hormone alterations: Ashwagandha may increase thyroid hormone levels, which could be problematic for those with thyroid disorders. Always check with your healthcare provider if you have thyroid disease before starting.
🧪 Summary of Findings
| Concern | Summary |
|---|---|
| Bradycardia | Rare reports; limited specific studies. |
| Heart Palpitations | Infrequent; often related to high doses or individual sensitivity. |
| Blood Pressure | May lower blood pressure; caution with antihypertensive medications. |
| Anxiety & Mood | Potentially reduces anxiety; some report mood swings or irritability. |
| Cognitive Function | Limited evidence of enhancement; further research needed. |
| Gastrointestinal | Common mild side effects; typically transient. |
| Liver Function | Rare liver injury cases; monitoring recommended during prolonged use. |
| Thyroid Function | May affect thyroid hormones; consult healthcare provider if thyroid issues exist. |
| Pregnancy/Breastfeeding | Not recommended due to potential risks. |
Safety in Special Populations
- Pregnancy and Breastfeeding:
Not recommended due to potential risks to the fetus or infant. There isn’t enough safety data to support use during these periods. - Medication Interactions:
Ashwagandha can interact with sedatives, immunosuppressants, thyroid medications, and blood pressure drugs. Inform your healthcare provider if you are taking any medications.
Practical Tips for Safe Ashwagandha Use
- Start Low, Go Slow: Begin with the lowest effective dose and monitor your body’s response.
- Choose Quality Products: Opt for supplements tested for purity to avoid contaminants that could cause side effects.
- Consult a Professional: Especially important if you have heart issues, thyroid conditions, or take medications.
- Monitor Symptoms: Keep track of any unusual sensations like palpitations, dizziness, mood changes, or digestive discomfort.
- Avoid During Pregnancy: Until more is known, steer clear if pregnant or breastfeeding.
Final Thoughts: Is Ashwagandha Right for You?
Ashwagandha remains a promising natural remedy with a good safety profile for most individuals. The latest research in 2024 reinforces its benefits in stress reduction, blood pressure management, and potential cognitive support. However, the possibility of side effects—especially concerning heart rate and mental health—means it’s essential to use it thoughtfully.
By staying informed, choosing reputable products, and consulting healthcare professionals, you can harness the benefits of this ancient herb while minimizing risks.
Have you tried ashwagandha? Share your experiences or questions in the comments below—we’d love to hear how it’s worked for you!
🧠 Frequently Asked Questions (FAQs)
1. Can ashwagandha cause heart palpitations or a racing heart?
In rare cases, users have reported heart palpitations or a racing heartbeat, typically linked to higher doses or individual sensitivity. Clinical evidence does not suggest this is a common effect, but those with existing heart conditions should consult a doctor before use.
2. Does ashwagandha lower or raise blood pressure?
Ashwagandha may lower blood pressure by reducing stress and improving circulation. While beneficial for those with high blood pressure, it can cause dizziness or fatigue in individuals with already low blood pressure or those on antihypertensive medications.
3. Is ashwagandha safe for people with heart conditions?
Generally, yes—when used under medical supervision. However, people with arrhythmias, bradycardia, or those on cardiovascular medications should seek professional guidance to avoid potential interactions.
4. Can ashwagandha cause anxiety or mood swings?
While it’s typically used to reduce anxiety and promote calm, a small subset of users have reported increased irritability or mood swings. These effects are usually mild and may result from individual responses or drug interactions.
5. Does ashwagandha affect thyroid function?
Yes. Ashwagandha can increase thyroid hormone levels, which may benefit hypothyroid individuals but can cause complications for those with hyperthyroidism or who take thyroid medication. Always check thyroid function regularly if using long-term.
6. Is ashwagandha safe for long-term use?
Short-term use (up to 8–12 weeks) is generally well tolerated. For long-term use, monitor liver and thyroid function, and consider taking breaks (cycling) under the supervision of a healthcare provider.
7. Can I take ashwagandha with prescription medications?
Ashwagandha can interact with sedatives, thyroid meds, blood pressure medications, immunosuppressants, and SSRIs. Always disclose supplement use to your doctor before combining with prescriptions.
8. Is it safe to take ashwagandha daily?
Yes, most clinical studies use daily doses ranging from 250–600 mg of a root extract standardized to withanolides. Still, individual tolerance and health status must be considered. Start low and monitor.
9. What are the most common side effects of ashwagandha?
Common side effects include digestive discomfort, drowsiness, and mild headaches. These usually resolve with dosage adjustment or discontinuation. Serious side effects like liver injury are extremely rare.
10. Should I avoid ashwagandha during pregnancy or breastfeeding?
Yes. Due to limited safety data and potential effects on hormones and fetal development, ashwagandha is not recommended during pregnancy or breastfeeding.