Pregnancy is a season of transformation—not just for your body, but for your entire life. Every day, you are nourishing and shaping a tiny human, and while the world around you may feel overwhelming, the foods you choose can be a steady, empowering force. Among all the advice and prenatal checklists, two humble superfoods stand out for their reliability, versatility, and sheer nutrition: chia seeds and avocado.
If you’re hoping for glowing skin, steadier energy, healthy digestion, and the best possible start for your baby’s developing brain, you’ll love what these foods can do for you. This isn’t just theory—this is drawn from research, real stories, and practical, lived experience. Let’s go deep, but also make it real.
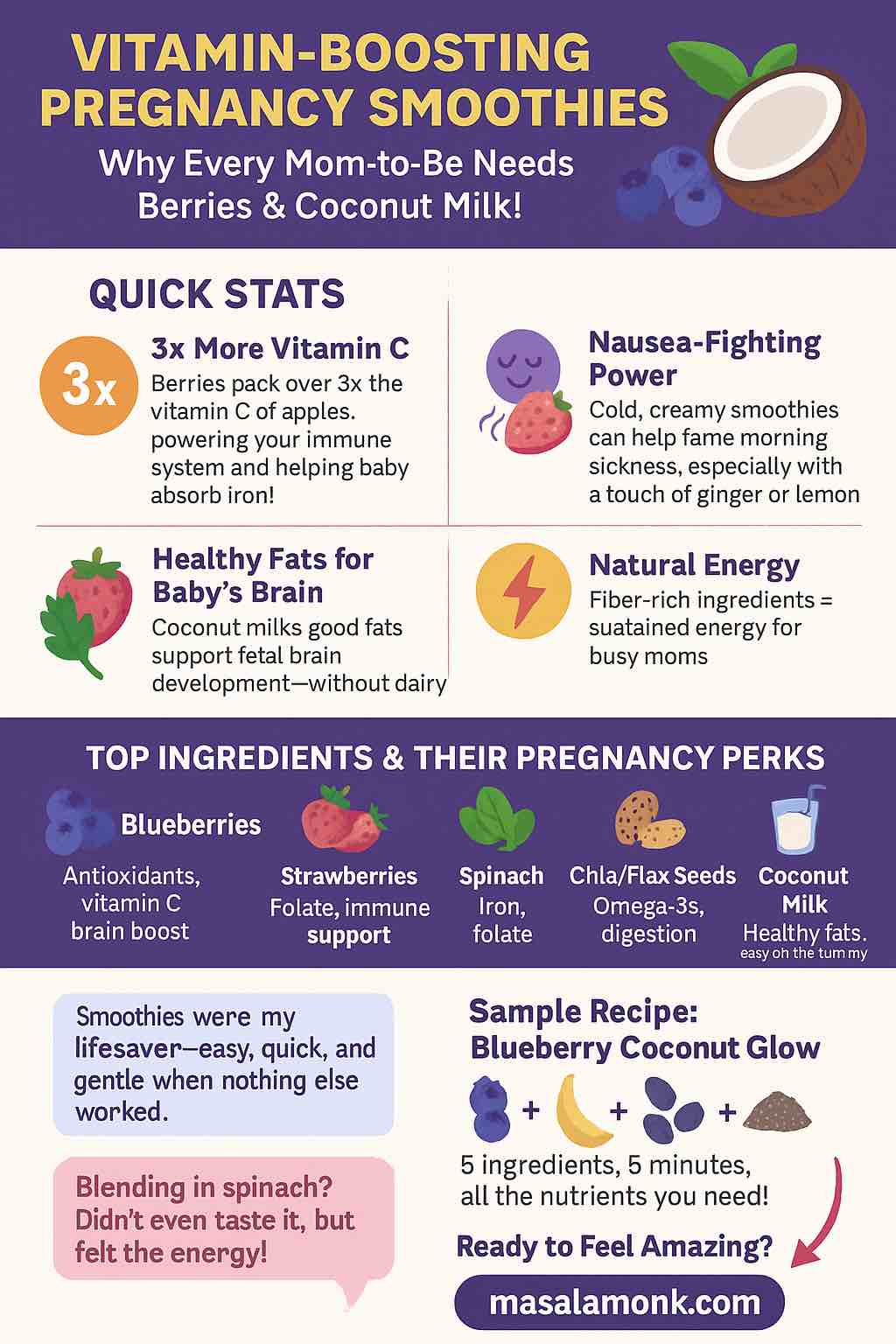
Why Omega-3s Matter (And Why Chia & Avocado Belong On Your Plate)
You’ve probably heard omega-3s are important, but maybe you’re not sure why. Here’s what’s happening behind the scenes as you nourish yourself:
- Your baby’s brain and eyes are made largely from fats, especially DHA and EPA—the “long-chain” omega-3s.
- Your own body uses omega-3s to lower inflammation, keep your heart strong, and support mood swings (hello, hormones).
- Not all omega-3s are equal: Chia seeds provide ALA (alpha-linolenic acid, a plant omega-3), which your body can partly convert to DHA/EPA—but only in small amounts. That’s why experts recommend eating low-mercury fatty fish or taking an algae-based supplement for full coverage.
What about avocados? They’re not a direct omega-3 powerhouse, but their monounsaturated fats help your body absorb nutrients, and their folate is vital for preventing birth defects and supporting new cell growth.
Together, chia and avocado form a nutritional “dream team” that’s flexible, gentle, and genuinely satisfying.
Also read Glycemic index of Chia Seeds and their effectiveness on Blood Sugar
The Real Life Stories: What Pregnant Women Say
Every pregnancy is unique, but certain themes come up again and again in forums, blogs, and quiet conversations:
- “Chia seeds are my MVP!”
One mom on Reddit shared how chia pudding ended her pregnancy constipation, improved her hydration, and made her feel more energetic. “Gone are the constant dehydration and pee breaks… gone is the constipation (and discomfort that comes with it)!” she writes. - Avocado’s creamy comfort
In pregnancy groups, women describe avocado as a “food they could always keep down” when everything else triggered nausea. For many, avocado toast was a daily breakfast—sometimes the only one that felt “safe.” - Caution learned the hard way
Others warn against eating dry chia seeds: “I tried eating them sprinkled on oatmeal without soaking—my stomach was so uncomfortable!” The lesson? Always soak chia seeds so they expand before reaching your digestive tract.
Related Reads: Level Up Your Pregnancy Nutrition
Want to go even deeper with your pregnancy diet? Here are some carefully selected articles that can help you make the most of omega-rich seeds and creamy avocados:
1. Get the Facts on Chia Seeds and Pregnancy
Before adding a new superfood, it’s natural to wonder about safety and side effects. For a comprehensive look at why chia seeds are considered safe—and how much is best—check out Is it safe to eat Chia seeds during Pregnancy?. This post covers everything from daily portion guidelines to hydration tips for preventing digestive discomfort.
2. More Plant-Powered Omega-3 Ideas
If you’re looking for additional vegan snack inspiration, don’t miss 5 Omega-3 Rich Vegan Snack Ideas for Pregnant Women: Chia and Flaxseed Mixes. From chia puddings to flaxseed crackers, these snacks are perfect for on-the-go nourishment and easy meal prep.
The Science in 2025: More Than Just Hype
Recent research backs up what moms have known intuitively:
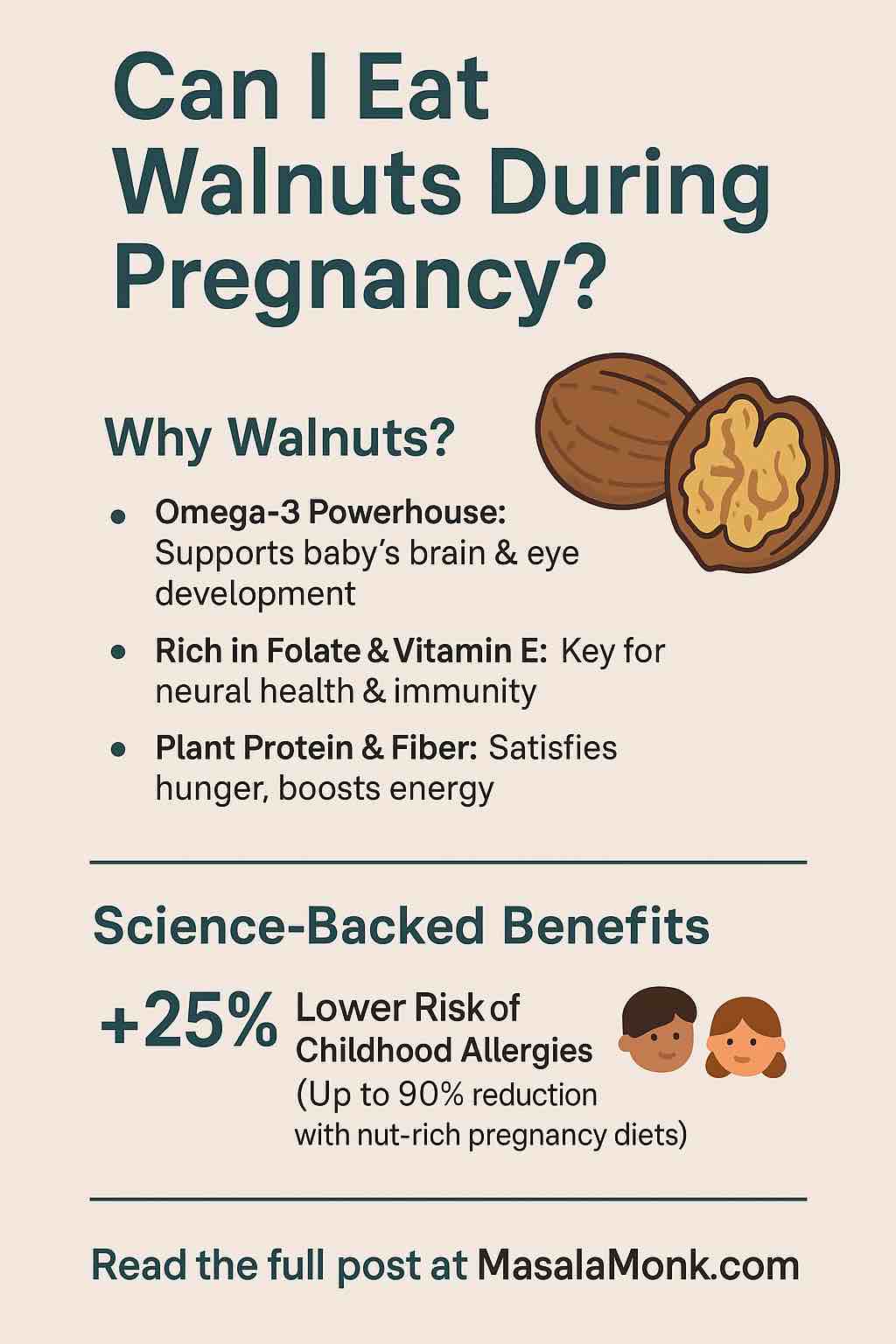
- Avocado and infant allergy protection:
A major 2025 Finnish study (KuBiCo) found that women who ate avocado regularly during pregnancy saw their babies’ risk of food allergies drop by nearly half. Scientists believe this is thanks to avocado’s folate, vitamin E, and healthy fats. - Omega-3s and healthy development:
Multiple studies confirm that moms who get enough omega-3s (especially DHA/EPA) see lower rates of preterm birth and improved early motor development in their babies. - Chia’s unique advantage:
While chia’s ALA omega-3 isn’t fully converted to DHA, it still helps balance inflammation, and its massive fiber content (about 10g per 2 tablespoons!) means smoother digestion—especially when prenatal vitamins and hormonal changes slow everything down.
How These Foods Fit Into Real Pregnancy Life
Let’s be honest: most of us don’t have the time or energy for complicated meal prep, especially when pregnancy symptoms are peaking. The beauty of chia and avocado is how seamlessly they fit into any routine:
- Quick breakfast win:
Throw chia seeds in almond milk before bed, and by morning you have pudding. Top with banana and a scoop of nut butter, or swirl in mashed avocado for creamy richness. - Snack magic:
Mash avocado with a little lemon and sea salt for an instant dip for whole grain crackers, or use as a spread for toast—topped with a sprinkle of soaked chia for crunch. - Energy booster:
Blend half an avocado, a handful of spinach, chia seeds (soaked), and your favorite frozen fruit with oat milk. The healthy fats slow sugar absorption, so you won’t crash mid-morning. - Lunch and dinner helper:
Toss sliced avocado and a sprinkle of chia over any salad, grain bowl, or soup. The flavors are mild enough to blend with nearly anything, and the nutrition boost is enormous.
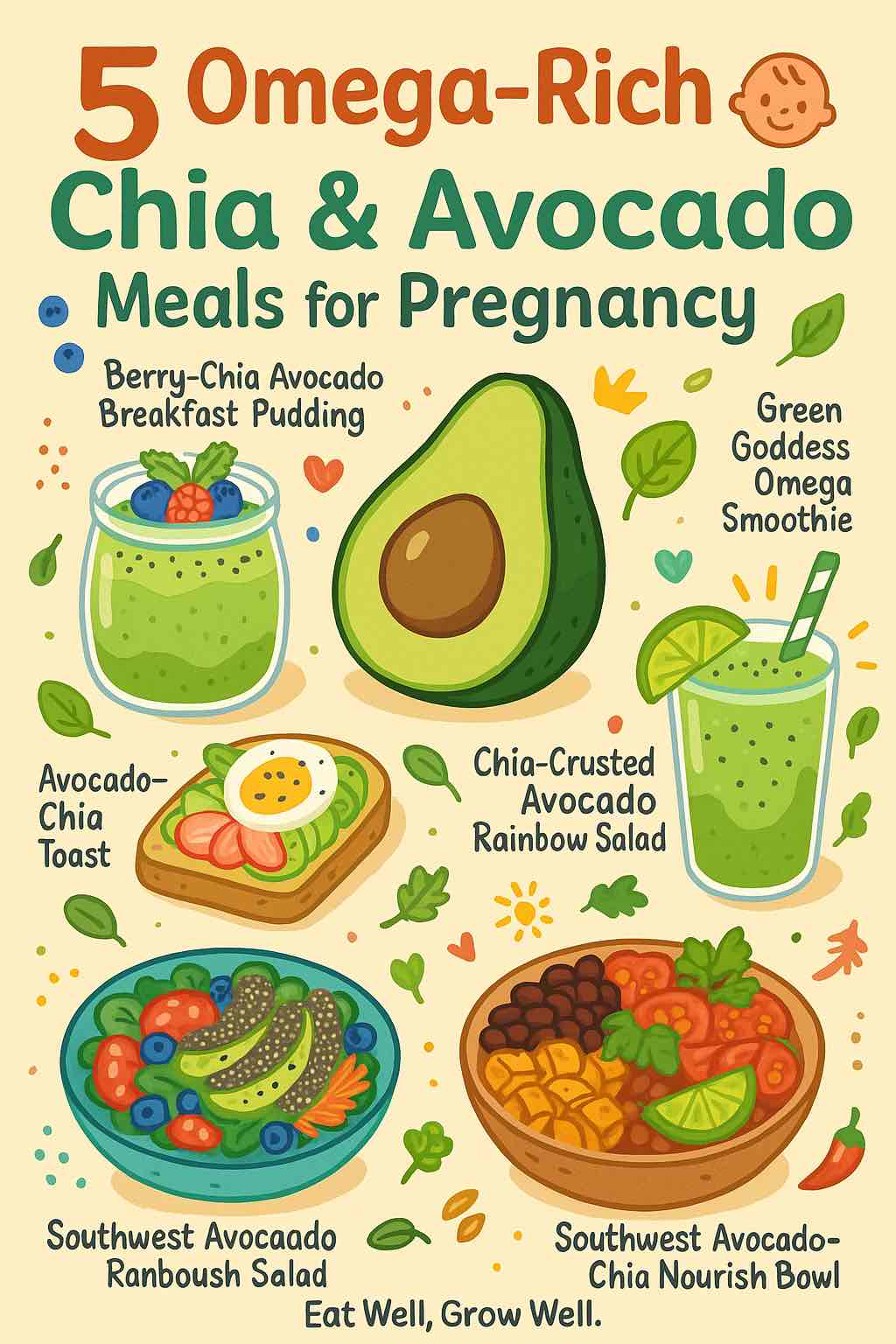
Five Creative, Omega-Rich Chia & Avocado Meals You’ll Actually Crave
One of the best things about chia and avocado is how easy they are to work into real life, no matter how unpredictable pregnancy makes your appetite. Whether you’re dealing with morning sickness, wild cravings, or that third-trimester “nothing fits in my stomach” feeling, these meals are adaptable, nourishing, and genuinely satisfying.
1. Berry-Chia Avocado Breakfast Pudding
Why you’ll love it:
This pudding is as easy as it is nourishing—a “set it and forget it” breakfast that feels like dessert but fuels you for hours. The chia thickens overnight, while the avocado adds silky texture and healthy fats. Perfect for mornings when you wake up hungry (or just want something cold and gentle).
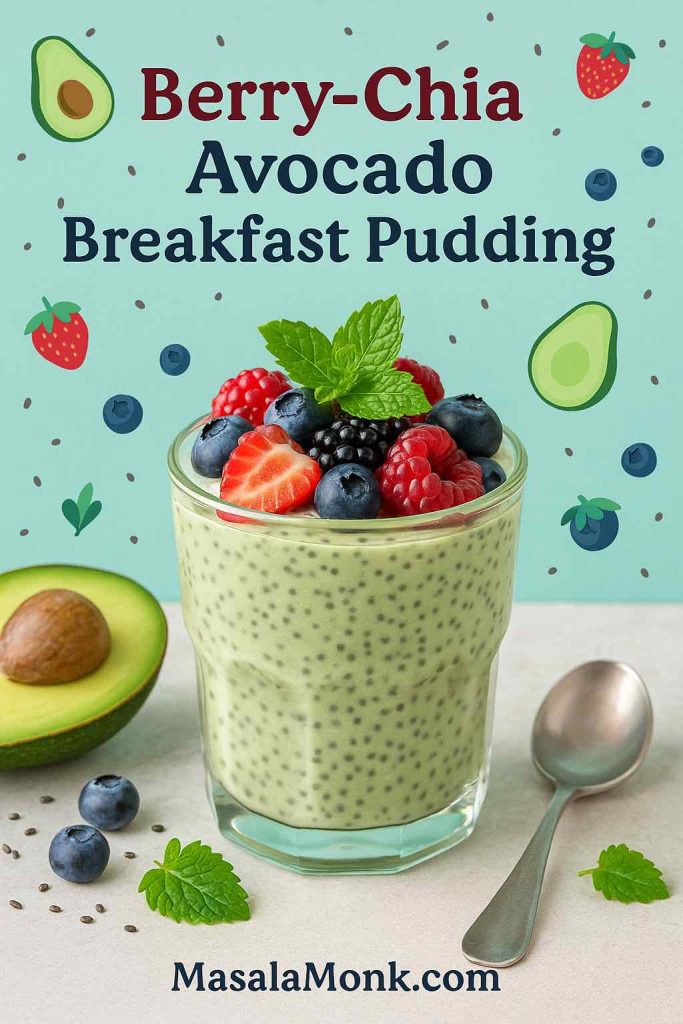
How to make it:
- In a jar or bowl, mash half a ripe avocado until creamy.
- Add 3 tablespoons chia seeds, 1 cup plant-based milk (almond, oat, or soy), a splash of vanilla, and a drizzle of honey or maple syrup.
- Stir well, cover, and refrigerate overnight (or at least 4 hours).
- In the morning, give it another good stir. Top with fresh berries, banana slices, or even a swirl of nut butter.
Real-life tip:
Make a few jars at once for grab-and-go breakfasts. If mornings are tough, you can even eat this as a midnight snack or soothing late-night mini-meal.
2. Avocado-Chia Power Toast
Why you’ll love it:
A pregnancy staple that’s endlessly customizable. The combination of fiber-rich bread, creamy avocado, and the tiny crunch of chia seeds keeps you full, supports digestion, and balances blood sugar. Plus, it’s quick—just five minutes from fridge to table.

How to make it:
- Toast your favorite whole-grain bread until crisp.
- Smash half an avocado with a squeeze of lemon juice and a pinch of salt, then spread thickly onto your toast.
- Sprinkle with 1 tablespoon chia seeds (pre-soaked for easier digestion, if you like).
- Top with extras: sliced boiled egg for protein, tomato or radish for freshness, or even a sprinkle of chili flakes if you crave heat.
Real-life tip:
If you’re rushing out the door, wrap your toast in parchment for a truly portable breakfast. You can also prep the smashed avocado and chia the night before.
3. Green Goddess Omega Smoothie
Why you’ll love it:
A lifesaver when your appetite is low, your nausea is high, or you just want a cool, refreshing way to sneak in veggies and healthy fats. The avocado makes it velvety, the chia boosts your omega-3s, and the banana/berries add just enough sweetness.
How to make it:
- In a blender, combine 1 cup baby spinach or kale, half a ripe avocado, 1 tablespoon soaked chia seeds, ½ banana, and 1 cup plain yogurt or dairy-free kefir.
- Add a handful of frozen berries for antioxidants, and enough water or plant milk to blend smoothly.
- Blend until creamy. Taste and add a splash of lemon or a tiny pinch of ginger if you’re battling nausea.
Serving ideas:
Pour into a mason jar and keep it cool for on-the-go sipping. If you’re craving crunch, sprinkle a little granola or pumpkin seeds on top and eat it with a spoon.
Real-life tip:
This is a gentle way to “hide” greens if your stomach is sensitive—just add more banana if you want it sweeter or creamier.
4. Chia-Crusted Avocado Rainbow Salad
Why you’ll love it:
Sometimes you want a meal that looks as good as it tastes—this salad is a true mood-booster, bursting with color, crunch, and nourishing fats. Chia seeds add a unique texture, and the whole thing takes less than 10 minutes.
How to make it:
- Slice one ripe avocado, dip each slice lightly in lemon or lime juice.
- Roll the slices in chia seeds to lightly “crust” them.
- Arrange on a big bed of mixed greens (spinach, arugula, or whatever you love).
- Add colorful extras: shredded carrot, cherry tomatoes, cucumber, sweet corn, thin-sliced red onion, or roasted beets.
- Finish with a drizzle of olive oil and balsamic vinegar, and a sprinkle of sunflower or pumpkin seeds.
Real-life tip:
Salads can be tough when you’re sensitive to textures—chopping everything small makes it easier to eat. If raw veggies are a no-go, try roasted instead, or add warm grains (quinoa, brown rice) for extra comfort.
5. Southwest Avocado-Chia Nourish Bowl
Why you’ll love it:
This bowl is cozy and deeply satisfying—ideal when you need real substance but still want to eat clean. Every bite delivers plant protein, slow carbs, fiber, and healthy fats. It’s naturally gluten-free and totally customizable.
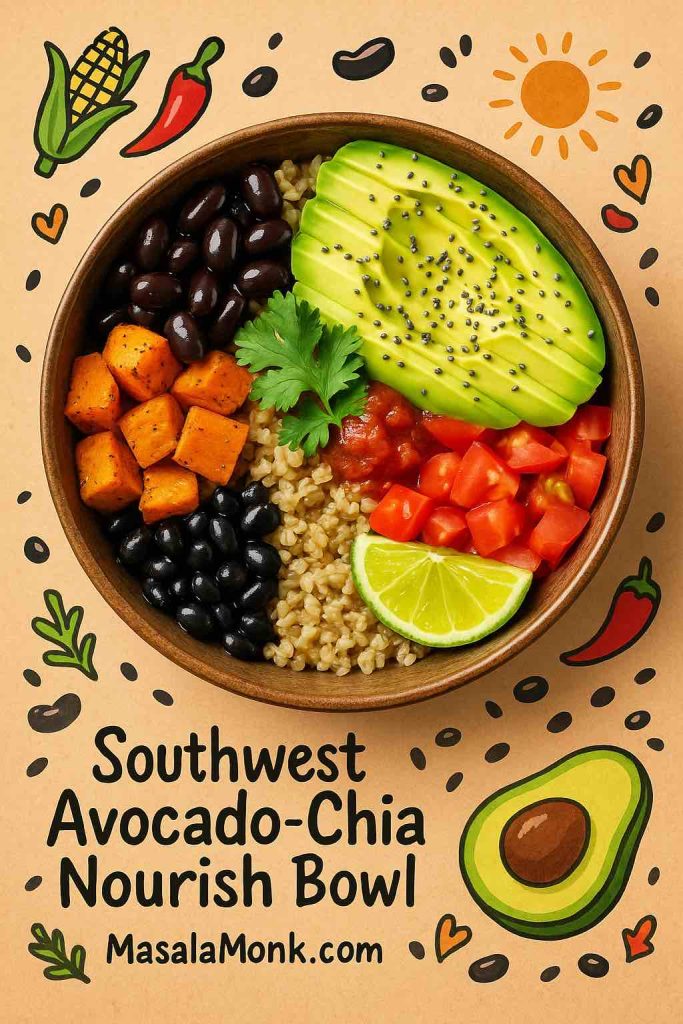
How to make it:
- Start with a base of cooked brown rice, quinoa, or even farro.
- Layer on: black beans (or pinto beans), roasted sweet potato cubes, diced tomatoes, sliced avocado, and a generous sprinkle of chia seeds.
- Add flavor: top with salsa, a dollop of Greek yogurt or vegan sour cream, fresh cilantro, and a squeeze of lime.
- For extra oomph, toss in corn, shredded lettuce, or diced bell peppers.
Real-life tip:
Bowls are perfect for meal-prep—just keep the avocado and chia separate until serving to keep everything fresh. Leftovers are great for lunch the next day (or midnight snacking).
Bonus: Make It Yours
All of these meals are endlessly adaptable. If you’re plant-based, swap dairy for coconut yogurt or almond milk. If you want more protein, add eggs, tofu, or a sprinkle of hemp seeds. Pregnant and short on time? Keep pre-sliced avocado and soaked chia in the fridge so you can throw meals together in minutes.
Making It Practical: Real Tips From Real Moms
- Batch it:
Prep chia pudding in jars at the start of the week—add different fruits or spices each day to keep things interesting. - Portable snacks:
Carry a small container of soaked chia and a ripe avocado in your bag for a quick, satisfying snack on the go. - Listen to your cravings:
Some days you’ll want all the avocado, other days chia smoothies are easier to get down. Trust your body’s signals; pregnancy hunger changes all the time. - Gentle hydration:
Chia seeds absorb water, so they’re a natural way to boost hydration—especially helpful if you’re prone to headaches or swelling. - Eat the rainbow:
Use chia and avocado as the base, then add whatever colorful produce you have—berries, tomatoes, spinach, or even roasted veggies. - Pair with protein:
For longer-lasting fullness, add nuts, eggs, cheese, or a plant protein source to any chia-avocado meal.
Love Avocado and Chia? Discover More Pregnancy Superfoods
Craving more variety? Pregnancy is the perfect time to explore nutrient-dense foods that are gentle, filling, and delicious. Here are some more reads you might enjoy:
1. Try New Ways to Eat Omega-3s
See how other moms are working chia and flax into their pregnancy diets with 5 Omega-3 Rich Vegan Snack Ideas for Pregnant Women: Chia and Flaxseed Mixes. These ideas are a lifesaver for anyone with cravings or a busy schedule.
2. Understand Chia Safety First
Still have questions? Dive into Is it safe to eat Chia seeds during Pregnancy? for the latest research and practical advice straight from nutritionists and real moms.
3. For More on Pregnancy Nutrition
If you’re curious about the broader benefits of a plant-rich pregnancy diet, explore Nutrition for Pregnancy: 5 Omega-Rich Chia and Avocado Meals for more meal ideas, research, and practical eating tips.
The Emotional Side: Food as Comfort and Connection
Pregnancy can be a lonely road, and food is about more than just nutrients. Preparing a beautiful chia pudding the night before, or sharing avocado toast with a partner on a slow morning, can be a small act of self-kindness and connection.
Many women describe the relief of finding one or two go-to foods that always “work” for their body—even when morning sickness makes everything else a gamble. Chia and avocado often become those trusted foods, helping moms-to-be feel both nourished and normal.
Bringing It All Together: Your Pregnancy, Your Nourishment
No single food is a magic fix—but small, powerful choices add up. Chia and avocado are not only practical, affordable, and easy to prepare; they’re foods that meet you where you are—on the best days and the hardest.
They’re gentle on the stomach, full of what you and your baby need, and endlessly adaptable. Whether you’re just starting your pregnancy journey, in the thick of the third trimester, or already holding your little one, these meals are a gift you can give yourself every day.
So try a new recipe, experiment with flavors, or just add a spoonful of chia or a slice of avocado to what you’re already eating. Trust your intuition, celebrate the small wins, and remember: nourishment isn’t just about food—it’s about honoring yourself as you bring new life into the world.
If you have a favorite chia or avocado recipe, or a tip that’s helped you, please share it in the comments below. Your story could be the encouragement someone else needs today.
Frequently Asked Questions (FAQs)
1. Are chia seeds safe to eat during pregnancy?
Yes, chia seeds are safe for most pregnant women when eaten in moderation (1–2 tablespoons per day). Always soak them before eating to prevent digestive discomfort and help your body absorb the nutrients.
2. How much avocado can I eat each day while pregnant?
½ to 1 whole avocado daily is a great, nutritious portion for most people. Avocados are packed with folate, potassium, and healthy fats, but also contain calories, so enjoy in balance with other foods.
3. Can I get enough omega-3 for my baby from chia seeds alone?
Chia seeds are a great source of plant-based omega-3 (ALA), but your body only converts a small amount to DHA and EPA (the most important types for baby’s brain development). Consider adding low-mercury fish or an algae-based DHA supplement for full coverage.
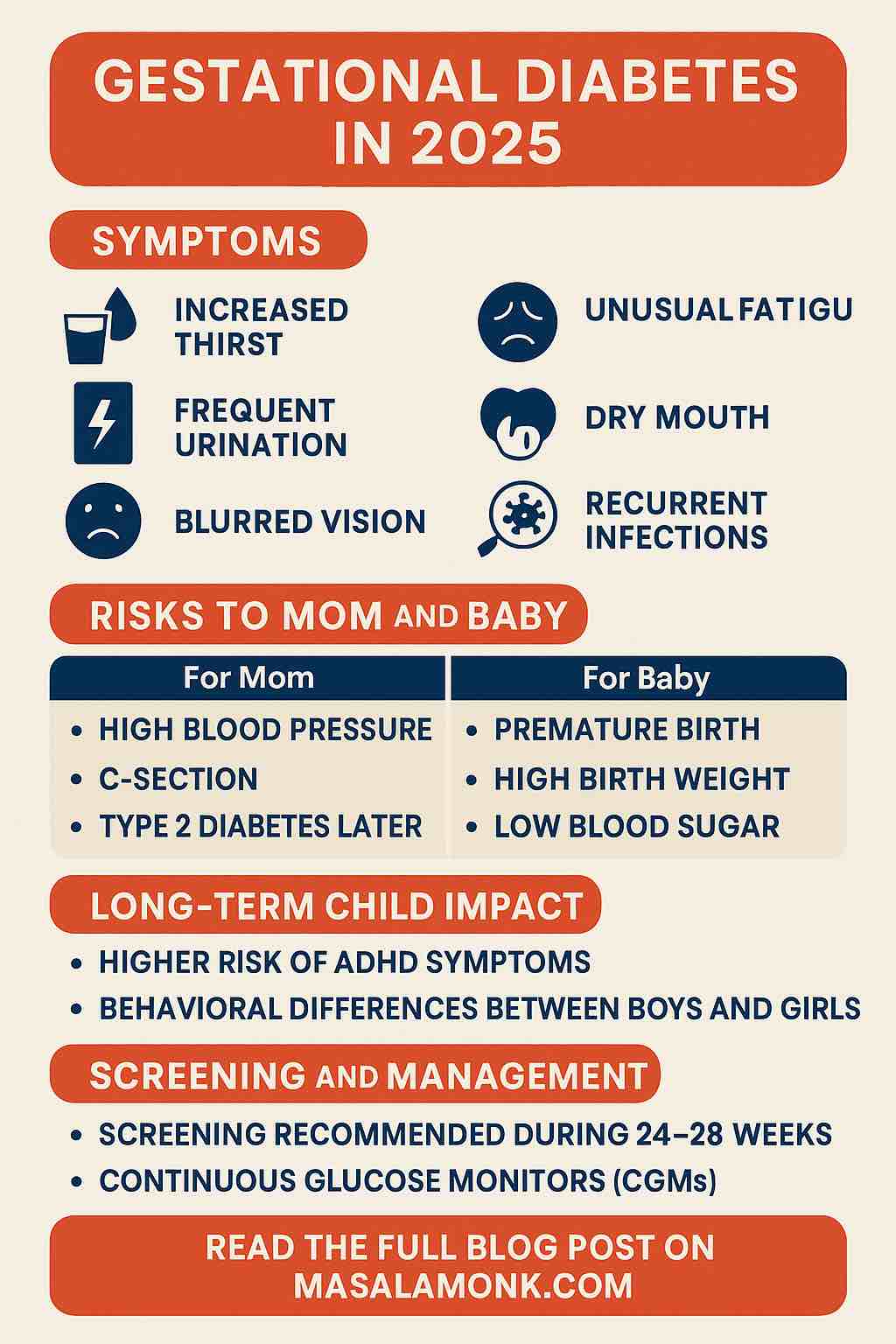
4. Are these meals suitable for gestational diabetes?
Yes! Both chia seeds and avocado are low in carbs and high in fiber and healthy fats, which help balance blood sugar. Always check with your healthcare provider for personal recommendations.
5. Will eating avocado really reduce my baby’s risk of allergies?
New research suggests regular avocado intake in pregnancy may lower the risk of food allergies in babies, possibly due to its folate and healthy fat content. While it’s not a guarantee, it’s a delicious and nourishing choice!
6. Can I prepare these meals ahead of time?
Absolutely. Chia pudding can be made the night before, and salad ingredients or smoothie packs can be prepped in advance. Keep avocado slices wrapped or in a little lemon juice to prevent browning.
7. What if I’m vegan or vegetarian?
All meals in this post are plant-based or easily adapted. For omega-3, pair chia with walnuts, flaxseed, and a DHA-rich algae supplement for the best nutrient coverage.
8. Are there any risks to eating too many chia seeds?
Large amounts (over 2–3 tablespoons at once) can cause bloating or digestive upset, especially if not well-soaked. Start with small portions and drink plenty of water.
9. How can I add protein to these meals?
Top with eggs, cottage cheese, Greek yogurt, nuts, seeds, beans, or lentils for extra protein. For vegan options, try tofu, tempeh, or protein-rich plant yogurt.
10. Will my kids or partner enjoy these recipes too?
Definitely! The flavors are family-friendly, and you can let everyone customize their toppings or bowls. Many parents find these meals are a great way to encourage healthy eating for the whole family.