People love simple rituals. A tall glass of water. A splash of vinegar. A squeeze of lemon. The routine feels clean and doable, which is part of its charm. Still, it helps to be honest. Apple cider vinegar and lemon juice for weight loss can support better choices for some people, mostly because it makes water more appealing and may help a few folks feel fuller. Even so, it’s not a switch you flip to change your body overnight. Progress still leans on ordinary decisions repeated often: meals anchored by protein and plants, everyday movement, and decent sleep.
Rather than pitching another miracle, let’s slow down and explore the drink in a realistic way—what research actually says, how lemon genuinely helps, what safety looks like in real life, and the gentlest way to try the ritual if you’re curious. Along the way, you’ll find straightforward resources from trusted health publishers and several MasalaMonk reads to make the journey tastier and easier to keep.
Also Read: Lentil Pasta for Weight Loss: Nutrition, Best Brands & 5 Healthy Recipes.
What apple cider vinegar and lemon juice for weight loss can and can’t do
To begin with, expectations matter. The Mayo Clinic puts it plainly: vinegar alone is unlikely to drive significant weight loss, and the evidence just isn’t strong enough to promise big results. Their concise guidance on apple cider vinegar is a useful reset if you’re sorting through bold claims you’ve seen online (Mayo Clinic’s guidance on ACV for weight loss).
That said, there are reasons the habit keeps getting attention. Some small studies and reviews report that vinegar can blunt post-meal blood-sugar rises and slow gastric emptying. In plain language, digestion may take a touch longer, and energy swings may feel steadier. For some, that translates into modest appetite control. However—and this is important—the effect tends to be small, short-term, and heavily dependent on your overall pattern. For a measured, readable overview that balances interest with caution, Harvard Health’s discussion of the “ACV diet” is worth a skim (Harvard Health’s overview). Likewise, Health.com has a recent explainer that lands in the same place: there might be a small nudge when ACV is used alongside a calorie deficit, but robust proof is limited (Health.com’s explainer).
Stepping back, the pattern is consistent: apple cider vinegar and lemon juice for weight loss might be a possible nudge, not a cure-all. If you enjoy the taste and you use the drink to replace a sweetened beverage, it may tilt the day in your favor. If you dislike it or it bothers your stomach, you can safely skip it—plenty of people reach their goals without ever sipping vinegar.
Also Read: Chia Seed Water: Benefits, Recipes & Best Time to Drink for Weight Loss
Where lemon genuinely helps—and where it doesn’t
Lemon earns its place here for reasons that are refreshingly down-to-earth. It brightens water, adds a familiar aroma, and turns hydration into a habit you might actually look forward to. That alone can change a day. A squeeze of juice offers a little vitamin C and makes the ritual feel fresh. However, honest evidence that lemon juice directly drives fat loss in humans is thin. Consider it flavor and hydration support, not a fat-burning trigger.
If citrus rituals appeal to you, two simple MasalaMonk companions can help you fine-tune the vibe you enjoy: the cozy routine of warm lemon water in the morning and the crisp refreshment of cold lemon water. Pick the version you’ll actually repeat.
Safety first: protect teeth, throat, and stomach
Because vinegar is acidic, the biggest long-term concerns with sloppy use aren’t your waistline—they’re your teeth and comfort. Enamel erosion creeps up slowly; throat irritation can turn a once-pleasant ritual into something you avoid. In addition, vinegar slows stomach emptying. Some people like the lingering fullness; others, especially those with reflux or delayed gastric emptying, find it uncomfortable. For a clear consumer-level rundown of common pitfalls—enamel wear, low potassium with heavy long-term intakes, and potential interactions with medications—see Verywell Health’s side-effects summary (Verywell Health on ACV side effects). Harvard also underscores two evergreen rules: dilute thoroughly and prefer food-first uses over “shots” (Harvard Health’s overview).
Practical steps you can trust:
- Always dilute ACV in plenty of water.
- Sip through a straw, then rinse your mouth with plain water.
- Give enamel ~30 minutes before brushing.
- Pair the drink with food if you’re prone to heartburn or queasiness.
- Check with your clinician first if you live with diabetes and gastroparesis, significant reflux/ulcer symptoms, kidney disease, or if you take insulin, digoxin, or certain diuretics.
These guardrails keep a small habit from becoming a big problem.
Also Read: Apple Cider Vinegar for Arthritis & Joint Pain: Myths vs Facts
How to make apple cider vinegar and lemon juice for weight loss (gentle method)
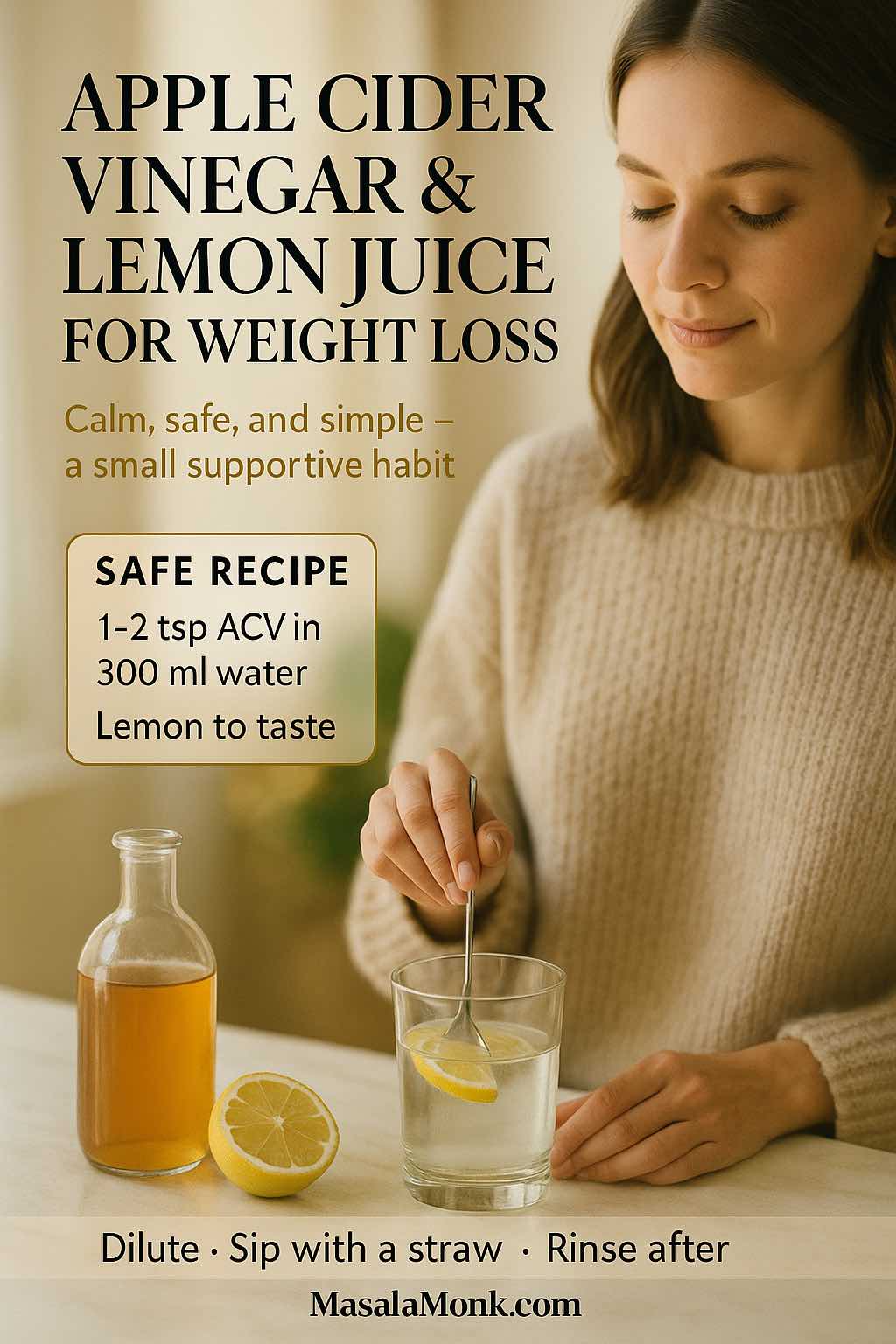
Let’s keep the method simple, the taste pleasant, and the dose sensible.
One-glass method (1 serving):
- Apple cider vinegar: start with 1–2 teaspoons; only increase if you feel fine. Most people don’t need more than 1 tablespoon per serving.
- Water: 250–300 ml (room temperature or warm).
- Lemon juice: 1–2 teaspoons (optional).
- Optional flavor: a slice of fresh ginger, or ½ teaspoon honey (remember honey adds calories).
How to:
Stir the vinegar into the water, add lemon, sip through a straw, then rinse with plain water.
When to drink:
With a meal or just before your most carbohydrate-heavy meal. There’s no proven “best time,” so choose a moment you’ll remember. The Mayo guidance emphasizes dilution and moderation above timing or brand (Mayo Clinic on ACV basics).
Daily ceiling:
Without medical advice, keep total intake around 15–30 ml (1–2 tablespoons) per day, always well diluted.
Brand note:
Choose a pasteurized vinegar you like and can find easily. There’s nothing magical about a label; dilution and habits matter more than logos.
Also Read: Best Nuts and Seeds for Weight Loss (Chia, Flax, Almonds & More)
Prefer not to sip? Put vinegar in food and smile
You do not have to drink acid to get the flavor benefits. In fact, using vinegar in meals may be the smarter path for your teeth and your tastebuds. A simple vinaigrette over crisp greens gives you the same acetic-acid experience while bundling it with fiber, protein, and healthy fats. If you’d like enamel-friendlier ideas that still feel indulgent, browse MasalaMonk’s safe apple cider vinegar salad dressing and a set of ACV dressing recipes. Use those approaches broadly—not only during pregnancy.
As you experiment, lean into texture and contrast: peppery greens, toasted seeds, juicy tomatoes, and a vinaigrette that makes you crave the next bite. When a salad becomes the part of lunch you anticipate, you’ve shifted the whole day in your favor without feeling deprived.
Morning or empty stomach: is it necessary?
Plenty of people adore a morning ritual; it feels like a reset. Nevertheless, there isn’t convincing evidence that sunrise timing or an empty stomach makes vinegar more effective for fat loss. If an empty stomach leaves you queasy, place the drink with breakfast. If you prefer an even gentler start, consider warm lemon water on its own and then use ACV later in the day inside food. For tuning your routine to your taste, the MasalaMonk guide to warm lemon water in the morning is a friendly read.
Variations of apple cider vinegar and lemon juice for weight loss
Because taste keeps habits alive, it’s worth exploring small tweaks.
- Honey: A drizzle rounds off sharp edges and makes the ritual feel softer. Just remember that sweetness brings energy; a half teaspoon adds roughly 20–25 calories. That’s easy to fit into your day when you plan for it.
- Ginger: Grated ginger adds warmth without much energy cost and can make the drink feel cozier. For more zesty, hydrating ideas, MasalaMonk’s cucumber, lemon, and ginger water has crisp combinations you can borrow.
- Spices: A pinch of black pepper brings a gentle kick. If you enjoy playful seasonings that don’t sneak in calories, lemon and black pepper offers easy variations.
Finally, some readers ask whether one famous ACV brand matters. It doesn’t, assuming you choose a pasteurized product and keep the dose modest. The basics—dilution, consistency, and an overall balanced plate—do the heavy lifting.
Tiny habit upgrades that compound over time
Instead of asking, “Will this drink make me lose weight?”, consider, “How can this ritual help me show up for myself the rest of the day?” A single glass won’t change your life. A small cascade of better choices might.
- Pair it with protein. Aiming for ~25–35 g of protein at meals steadies appetite and protects lean mass as you lose fat.
- Swap, don’t stack. Let the drink replace a sweetened beverage rather than adding on top of your usual routine.
- Front-load plants. Start lunch or dinner with a generous salad dressed in a light ACV vinaigrette.
- Walk after meals. Even a short stroll can steady post-meal blood sugar and clear your head.
- Guard your bedtime. Hunger and cravings improve when sleep is consistent.
If you like myth-free fundamentals, the Mayo Clinic’s weight-loss basics is calm and useful (weight-loss basics). And for perspective from dietitians who see the ACV trend often, EatingWell recently summarized their take: interesting, but far from magical (dietitians’ view at EatingWell).
Also Read: How Does a High Protein, High Fiber Diet Support Weight Loss?
A seven-day starter plan using apple cider vinegar and lemon juice for weight loss
Trying something new is easier with a script. Use this as a soft landing and adjust freely.
Days 1–2
Stir 1 teaspoon ACV into 300 ml water. Add a little lemon. Drink with lunch. Rinse your mouth after.
Days 3–4
Increase to 2 teaspoons if you feel fine. Keep the same dilution. Stay with meals so your stomach has company.
Days 5–7
Try 1 tablespoon once per day, or split across two smaller servings. Keep your daily total within 1–2 tablespoons. If you notice throat irritation, reflux, or tooth sensitivity, switch to food-first uses and reassess later.
Alongside the drink, build a plate you enjoy: a protein you actually like, plenty of vegetables, and a starch that suits the day. If you need citrus refreshers between meals, cold lemon water is a bright companion to keep you sipping without added sugar (cold lemon water ideas).
What results feel like with apple cider vinegar and lemon juice for weight loss
Outcomes vary—and that’s completely normal. One person feels fewer afternoon cravings. Another feels no change. Someone else decides the drink isn’t for them and keeps vinegar strictly in dressings. None of these experiences are wrong; they simply reflect biology and preference.
If you enjoy the ritual and it helps you replace a sugary beverage, you may notice slow, steady benefits. If you dislike it, you won’t miss anything by skipping. A bright salad often delivers the same nudge with fewer dental worries. For a realistic, dietitian-led take, EatingWell sums it up neatly: evidence is limited; any help is likely small; food-first habits do the heavy lifting (dietitians’ view). Meanwhile, Health.com’s recent explainer lands in the same place, with a simple reminder to dilute and keep expectations modest (Health.com explainer).
Also Read: Guide to Body Fat Percentage
A kind closing thought on apple cider vinegar and lemon juice for weight loss
Choose the version of this habit that fits your life. If you enjoy the taste, keep it well diluted and pair it with meals. If you prefer food-first, whisk a quick vinaigrette and enjoy a generous salad. Both paths can support a calmer appetite and better choices—the quiet way real change happens. If questions about safety linger, the Verywell Health side-effects overview is clear and practical, and the Harvard Health pieces add helpful context without sensationalism (Verywell Health side-effects; Harvard Health overview).
Finally, a quick note to keep you safe: because vinegar can interact with certain conditions and medications, and because tolerance varies, it’s wise to speak with your clinician if you have diabetes (especially with gastroparesis), kidney disease, or chronic reflux, or if you take insulin, digoxin, or particular diuretics. A short conversation now is worth more than a long detour later.
FAQs
1. Can I mix lemon juice with apple cider vinegar?
First, yes—you can mix them. Apple cider vinegar and lemon juice for weight loss is mostly about taste and a simple ritual; the combo can make water more appealing while you aim for balanced meals and steady movement.
2. Does apple cider vinegar and lemon juice in the morning work better?
Next, timing isn’t magic. Morning feels motivating for many, yet the gentle benefits are similar whether you drink it with breakfast, lunch, or another meal you’ll remember.
3. Should I drink it on an empty stomach?
Also, not everyone tolerates acid well on an empty stomach. Pairing the drink with food often feels easier on the throat and may reduce reflux or queasiness.
4. How much should I drink daily?
Meanwhile, start small—1–2 teaspoons of apple cider vinegar in 250–300 ml water—with a squeeze of lemon if you like; if it sits well, you can work up to 1 tablespoon per serving and keep your daily total near 1–2 tablespoons.
5. Is apple cider vinegar and lemon juice good for weight loss?
Still, consider expectations. Apple cider vinegar and lemon juice for weight loss may help you feel a little fuller and swap out sugary drinks, yet the real progress comes from your overall eating pattern, steps, and sleep.
6. What are the benefits and risks?
That said, potential upsides include a more satisfying beverage habit and, for some, steadier appetite; possible downsides include enamel wear, throat irritation, delayed stomach emptying, and interactions if you have certain conditions or take specific medications.
7. Is there a simple recipe I can follow?
However, keep it basic: 1–2 teaspoons ACV + 250–300 ml water + 1–2 teaspoons lemon juice; sip through a straw and rinse your mouth with plain water afterward; adjust tartness to taste.
8. Can I add honey or ginger?
Moreover, tiny tweaks help adherence—½ teaspoon honey softens sharpness (remember the calories), while a slice of fresh ginger adds warmth without much energy.
9. Is warm water better than cold?
Additionally, temperature is personal. Warm water can feel soothing, cold water can feel refreshing; choose whichever helps you repeat the habit comfortably.
10. Is apple cider vinegar better than lemon juice alone?
On balance, vinegar has the stronger tradition of modest effects; lemon mainly brightens flavor and supports hydration, which can indirectly help you stick to your plan.
11. How long before I notice changes?
Practically speaking, give any routine a few weeks while you also stack fundamentals—protein-forward meals, vegetables, walking—so any small nudge from the drink has room to matter.
12. Who should avoid this drink?
Generally, skip or speak with your clinician first if you have diabetes with gastroparesis, chronic reflux or ulcers, kidney issues, low potassium history, or if you take insulin, digoxin, or certain diuretics.
13. Can I use apple cider vinegar and lemon juice for weight loss at night?
Typically, evenings are fine if you tolerate acid well; if nighttime triggers reflux, place the drink earlier in the day or use vinegar in a salad dressing instead.
14. Does it target belly fat?
Ultimately, no single drink targets fat from one area. Apple cider vinegar and lemon juice for weight loss may support better choices, but body fat reduces overall when your daily pattern creates a gentle calorie deficit.