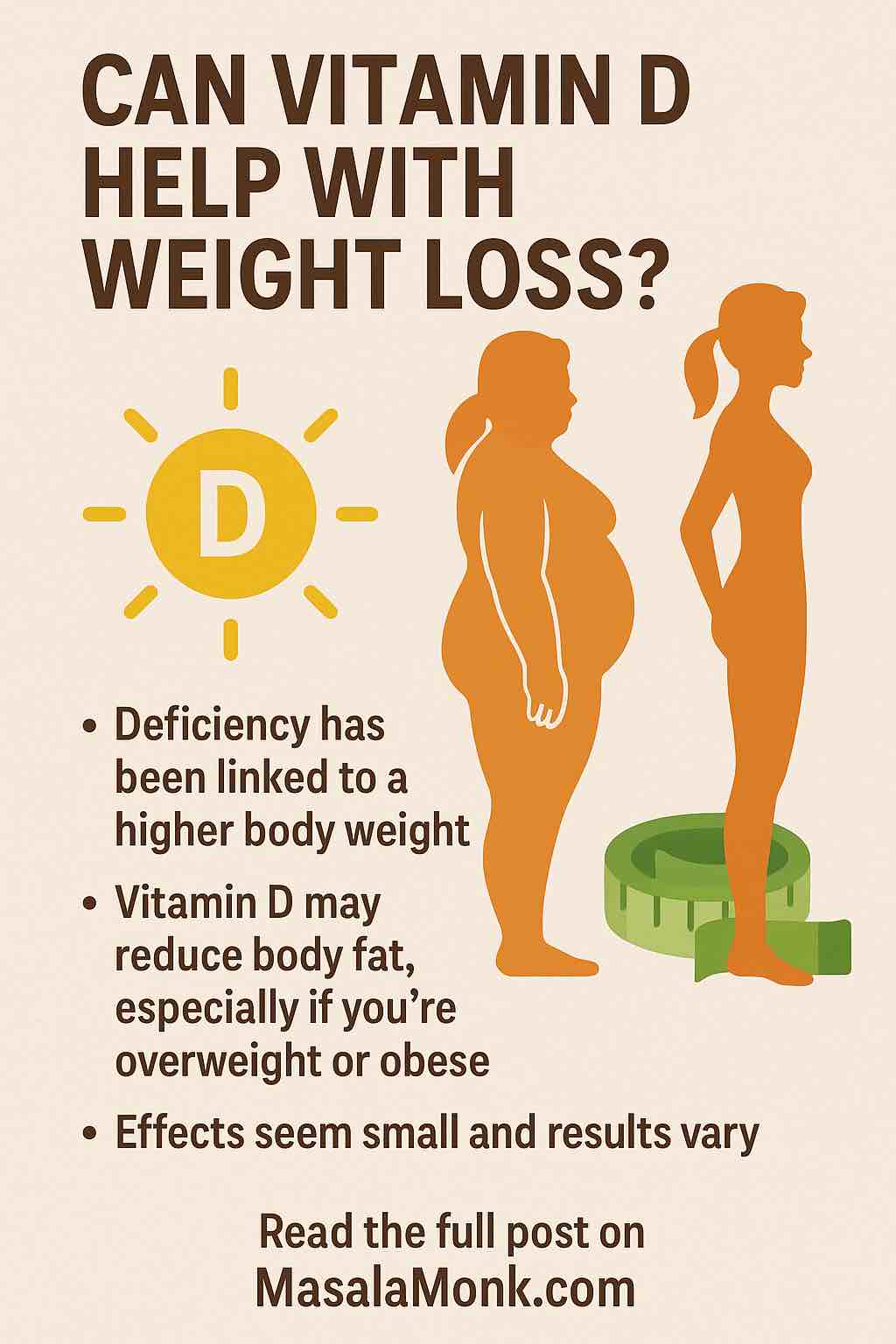
If you’ve ever searched for “easy weight loss tips,” you’ve probably seen vitamin D pop up on countless blogs and videos. Some say it melts belly fat, others claim it boosts metabolism, and a few warn it’s all hype. So what’s the truth? Is vitamin D the magic bullet for weight loss—or just another supplement myth?
In this article, we’ll take a deep dive into the real relationship between vitamin D and weight loss, sift through the latest science (with practical takeaways), and give you a step-by-step plan to use vitamin D as part of a holistic, healthy weight management strategy in 2025.
Vitamin D 101: The Basics
Vitamin D is called the “sunshine vitamin” because your skin makes it when exposed to sunlight. It’s vital for strong bones, immune health, mood, and (as newer research shows) a whole web of metabolic processes.
Key facts:
- Found in: fatty fish, egg yolks, fortified milk, supplements, and sunlight
- Measured as: 25-hydroxyvitamin D (25(OH)D) in blood tests
- Deficiency is common: especially in people who are overweight, have darker skin, live in northern latitudes, or spend most time indoors
What the Research Really Shows (as of 2025)
Let’s cut through the clickbait and see what the most recent and reliable studies tell us.
1. People with More Body Fat Tend to Have Less Vitamin D
- Fat tissue “hides away” vitamin D, making it less available in the bloodstream.
- This means overweight and obese individuals are more likely to be vitamin D deficient—even if they get some sun or eat fortified foods.
2. Losing Weight Increases Vitamin D Levels
- Why? As you lose fat, vitamin D stored in fat cells is released into the blood.
- Who benefits most? Recent research (2025) shows women, especially those with low vitamin D at the start, see the biggest boost. In fact, a 52-week study found that women who lost the most weight gained the most vitamin D—and those who started out low were more likely to keep the weight off.
3. Vitamin D Supplements Alone Don’t Melt Pounds—But They Help in Other Ways
- A mega-review (2022–2025) looked at over 15,000 participants: vitamin D slightly reduced waist circumference and BMI, but had no significant effect on overall weight or body fat when used alone.
- However: Supplements do seem to improve some markers like inflammation, insulin sensitivity, and metabolic health—making your weight-loss journey healthier and possibly easier.
4. Exercise and Diet Are Key—Vitamin D Supports the Process
- Regular exercise itself helps your body maintain active forms of vitamin D (even without losing weight).
- Combining calorie restriction, exercise, and vitamin D supplementation (especially if you start deficient) can produce better fat loss, lower inflammation, and a healthier metabolism.
5. High-Dose Vitamin D Has Some Effect—But Is Not for Everyone
- Some short-term studies with higher doses (>5,000 IU/day) show a little more BMI drop, but this is best done under medical supervision. There’s no substitute for the basics: food, movement, and lifestyle.
Practical Takeaways: What Should You Actually Do?
Here’s how to put the science into action.
Step 1: Test Your Levels
- Get a blood test for 25(OH)D, especially if you’re overweight, live far from the equator, rarely go outside, or have darker skin.
- Optimal range: 30–50 ng/mL (75–125 nmol/L) for most people.
- If you’re low, you’re not alone!
Step 2: If You’re Deficient, Supplement Smartly
- For most adults: 1,000–2,000 IU/day is safe. Some may need more (up to 4,000 IU/day) short term, but always check with your healthcare provider.
- Pair with calcium if your diet is low in dairy or greens.
Step 3: Focus on Diet and Movement
- Aim for a moderate calorie deficit (cutting 300–500 calories/day is a sustainable start).
- Exercise most days: both cardio and resistance training work. New research shows exercise alone (even without weight loss) keeps your vitamin D metabolism humming!
- Eat vitamin D-rich foods: Salmon, sardines, egg yolks, fortified milks/yogurt, and mushrooms (exposed to sunlight).
Step 4: Combine for Best Results
- If you’re already on a weight-loss journey, adding vitamin D (if you’re deficient) can help with inflammation, metabolism, and even your mood.
- For women, correcting low vitamin D may help keep weight off long term.
- Remember, vitamin D is a supporter, not a soloist.
Step 5: Monitor, Adjust, Re-test
- After 3–6 months, re-check your vitamin D levels and weight-loss progress.
- Adjust dose as needed (it’s possible to get too much of a good thing!).
FAQs
1. What is the ideal vitamin D level for weight loss and overall health?
The optimal blood level is generally 30–50 ng/mL (75–125 nmol/L). Levels below 20 ng/mL are considered deficient. While higher levels can support metabolic health, more isn’t always better—extremely high levels (>100 ng/mL) can be harmful.
2. Can taking vitamin D supplements alone help me lose weight?
Vitamin D supplements by themselves won’t cause significant weight loss. They may slightly reduce waist circumference and BMI, but meaningful weight loss requires a healthy diet and regular exercise. Supplements work best as part of an overall wellness plan, especially if you’re deficient.
3. How does weight loss affect my vitamin D status?
When you lose body fat, vitamin D stored in fat tissue is released into your bloodstream, often improving your blood levels. This means your vitamin D status usually gets better as you lose weight, particularly in women.
4. Who is most likely to be vitamin D deficient?
People who are overweight or obese, have darker skin, live in northern climates, rarely spend time outdoors, are older, or who don’t eat vitamin D-rich foods are at the highest risk for deficiency.
5. What are the best natural food sources of vitamin D?
Salmon, sardines, mackerel, cod liver oil, egg yolks, UV-exposed mushrooms, and fortified foods (like milk, orange juice, and cereals) are good dietary sources.
6. How much vitamin D should I take if I’m deficient?
Typical supplementation is 1,000–2,000 IU/day for maintenance, or 2,000–4,000 IU/day for those who are deficient—always check with your healthcare provider and monitor your blood levels.
7. Does vitamin D improve belly fat or target fat loss in specific areas?
Vitamin D is not a targeted fat-burner. Some studies show a modest reduction in waist circumference, but overall body fat distribution is mostly determined by genetics, hormones, and lifestyle factors.
8. Can I get too much vitamin D? What are the risks?
Yes. Excessive intake (over 4,000 IU/day long-term) can cause toxicity, leading to high blood calcium, kidney stones, or organ damage. Always follow dosage recommendations and check your blood levels periodically.
9. Should I combine vitamin D supplements with calcium?
If your diet is low in calcium, combining both (as in dairy or green vegetables) may further support weight loss and bone health. However, excess supplemental calcium is not necessary for everyone and should be personalized.
10. Does exercise help my body use vitamin D more effectively?
Yes! Recent research shows regular exercise helps maintain active vitamin D levels, even without weight loss, and supports better metabolism overall. It’s a win-win for both fitness and vitamin D health.
Final Thoughts: Vitamin D as Your Wellness Ally
Vitamin D won’t magically melt away the pounds—but it plays a real, science-backed role in supporting your weight-loss journey, especially if you start out low or are carrying extra weight.
Think of vitamin D as a silent partner: it won’t steal the show, but it can make everything run more smoothly—better metabolism, less inflammation, a happier mood, and (in women) maybe even an easier time keeping the weight off for good.
Ready to get started?
- Check your vitamin D.
- Move more.
- Eat well.
- Supplement if you need it.
- Reap the benefits—not just for weight, but for lifelong health.
Have more questions about vitamin D, supplements, or building a sustainable weight-loss plan? Drop them in the comments or get in touch!
This post draws on clinical trials, meta-analyses, and research published through 2025.