In today’s fast-paced world, stress is practically unavoidable. From work deadlines to social obligations, our bodies are constantly navigating a sea of stressors. And behind the scenes? A hormone called cortisol is often steering the ship. Produced by your adrenal glands, cortisol plays a crucial role in the “fight-or-flight” response. While helpful in acute situations, chronically high cortisol levels can lead to weight gain, sleep problems, anxiety, and even cardiovascular issues.
But here’s the good news: You can influence your cortisol levels naturally, and one of the simplest ways to do that is through what you drink. Yes, your daily beverages can either fuel the fire or help put it out. In this post, we dive deep into five evidence-backed drinks that help lower cortisol, support mental clarity, and bring your body back to balance.
What is Cortisol?
Cortisol is your body’s main stress hormone, produced by the adrenal glands. It helps regulate blood sugar, metabolism, blood pressure, and your “fight-or-flight” response. But when cortisol levels remain high for too long, it can cause issues like weight gain (especially belly fat), anxiety, sleep problems, and hormonal imbalances. That’s why learning how to balance cortisol naturally is so important.
How to Lower Cortisol Naturally and Quickly
If you’re wondering how to lower cortisol levels naturally, here are simple science-backed strategies you can try today:
- ✅ Sip calming teas like green tea, chamomile, or lemon balm.
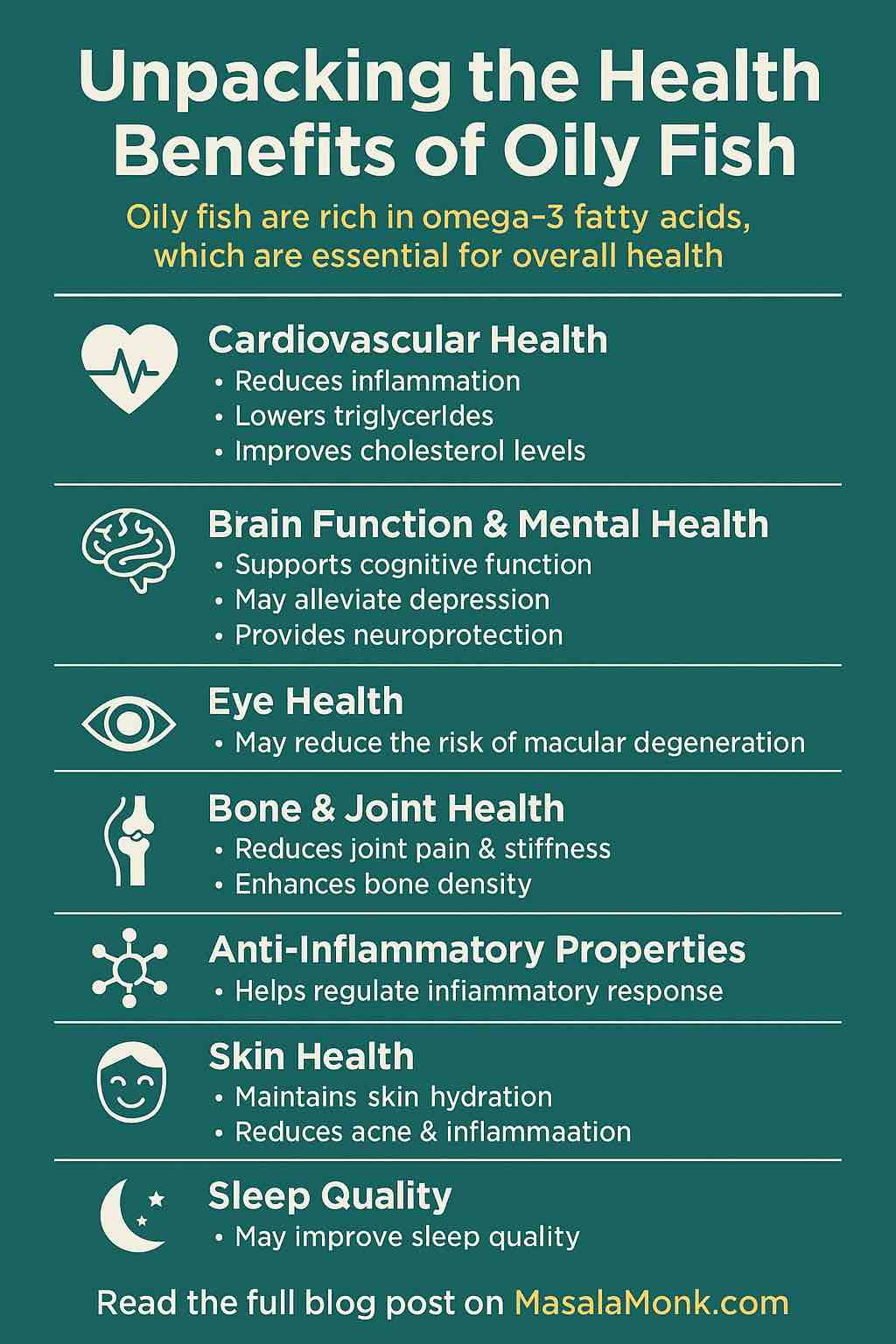
- ✅ Eat cortisol-lowering foods such as leafy greens, berries, and omega-3-rich fish.
- ✅ Avoid cortisol-triggering foods like sugar, alcohol, and processed snacks.
- ✅ Practice deep breathing or meditation for just 5 minutes a day.
- ✅ Stay hydrated, as even mild dehydration raises cortisol.
- ✅ Prioritize good sleep, since lack of rest is one of the biggest cortisol triggers.
👉 Consistency is key — small daily habits add up to lower stress and better hormonal balance.
Here you might want to read How to Naturally Lower Cortisol Levels?
Symptoms of High Cortisol in Women
High cortisol affects women differently than men. Common symptoms of elevated cortisol in females include:
- Irregular or missed periods
- Weight gain, especially belly fat (“cortisol belly”)
- Fatigue, even after sleeping
- Mood swings, anxiety, or irritability
- Thinning hair or increased facial hair
- Acne or skin problems
- Poor sleep quality or insomnia
If you notice several of these signs, it may be worth checking your cortisol levels with a healthcare provider.
For deeper insights into this, please refer to 10 Symptoms of High Cortisol Levels in Females
Foods That Trigger Cortisol (to Avoid!)
Some foods make cortisol spike, adding more stress to your system. To naturally lower cortisol, limit or avoid:
- ❌ Sugary drinks & desserts
- ❌ Refined carbs like white bread and pastries
- ❌ Too much caffeine (especially on an empty stomach)
- ❌ Alcohol
- ❌ Fried or processed fast foods
- ❌ Energy drinks
👉 Instead, swap in cortisol-friendly foods: whole grains, fatty fish, probiotic yogurt, herbal teas, and plenty of fruits and veggies.
Read More about 5 Foods That Increase Cortisol
Best Drinks to Lower Cortisol
Now coming to the main point of this post, if you’re searching for the best drinks that lower cortisol, here are top picks:
- 🍵 Green tea (L-theanine calms while antioxidants fight stress)
- 🌿 Chamomile or lemon balm tea (soothes the nervous system)
- 🥥 Adrenal cocktail (orange juice + coconut water + sea salt)
- 🧉 Probiotic drinks (kefir, kombucha, yogurt drinks)
- 🌱 Adaptogen elixirs (ashwagandha, rhodiola teas or lattes)
👉 These drinks don’t just hydrate — they actively support your body’s stress response and help balance cortisol levels naturally. Lets dig deeper into each one of them below.
1. 🍵 Green Tea: Calm in a Cup
Green tea isn’t just a morning ritual; it’s a scientifically supported stress soother. It contains two star compounds:
- L-theanine: An amino acid that promotes relaxation without sedation. It balances the stimulating effect of caffeine and may reduce cortisol responses in stressful situations.
- EGCG (Epigallocatechin gallate): A potent antioxidant known to reduce inflammation and modulate hormone balance.
Studies show that drinking several cups of green tea per day can significantly reduce cortisol levels and improve mood. One trial even observed a reduction in ACTH and corticosterone (both stress markers) after 6 weeks of daily green tea consumption.
How to enjoy it: Aim for 2–4 cups daily. Opt for decaf green tea in the evening to maintain cortisol-lowering benefits without interfering with sleep.
2. 🌿 Herbal Teas: Nature’s Tranquilizers
When it comes to non-caffeinated, stress-reducing beverages, herbal teas shine. Popular options include:
- Chamomile: Rich in apigenin, a flavonoid with calming effects.
- Lemon balm: Supports sleep and reduces nervousness.
- Passionflower: Traditionally used for anxiety and insomnia.
While herbal teas may not directly lower cortisol in all cases, they contribute to overall nervous system calm, indirectly reducing cortisol levels by improving sleep and lowering anxiety.
How to enjoy it: Brew a strong cup (or two) in the evening. Sip slowly and make it a mindful ritual.
3. 🥥 Adrenal Cocktail: A Trend Worth Trying
Popular on wellness blogs, the “Adrenal Cocktail” isn’t a medical treatment but a nutrient-packed drink designed to support adrenal function and energy regulation.
Typical ingredients:
- 1/2 cup fresh orange juice (vitamin C)
- 1/2 cup coconut water (potassium and electrolytes)
- A pinch of sea salt (sodium for adrenal support)
Vitamin C is crucial for adrenal gland function and helps regulate cortisol output. Electrolytes help maintain hydration, a key factor in stress resilience.
How to enjoy it: Drink mid-morning or mid-afternoon when cortisol naturally dips. It can also be a great post-workout replenisher.
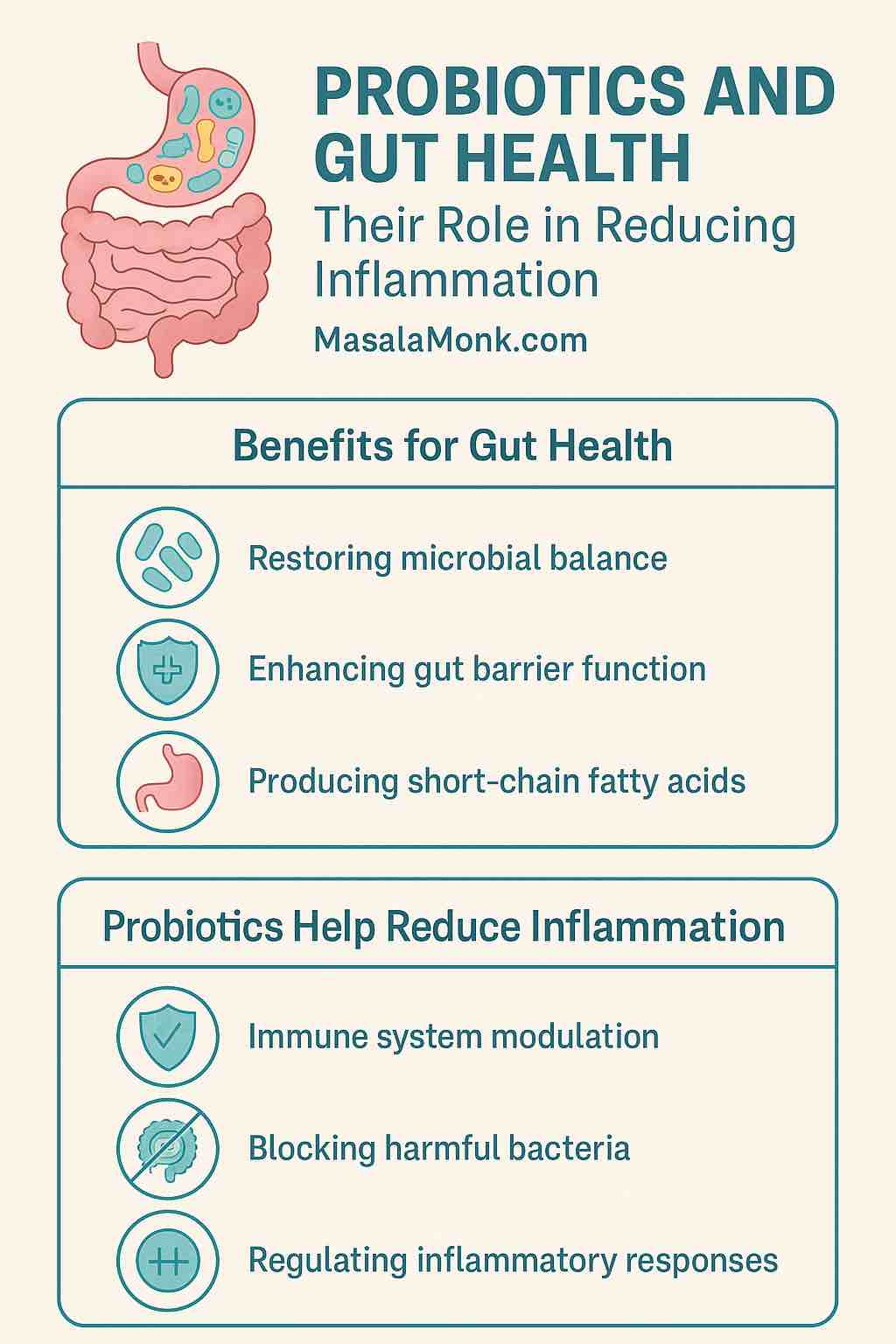
4. 🫲 Probiotic Drinks: Gut-Driven Stress Relief
The gut-brain axis is a major player in stress regulation, and your gut microbiome directly affects cortisol levels. Enter probiotic-rich drinks like:
- Kefir
- Probiotic yogurt drinks
- Kombucha (low sugar, non-caffeinated varieties)
A 12-week study among students showed that daily intake of probiotic beverages significantly lowered cortisol and improved stress perception.
How to enjoy it: Include one probiotic drink in your daily routine, ideally with meals. Choose high-quality products with live cultures and low added sugar.
5. 🌿 Adaptogenic Elixirs: Ancient Herbs, Modern Calm
Adaptogens are natural substances that help the body adapt to stress and normalize physiological functions. Popular adaptogenic herbs used in drinks include:
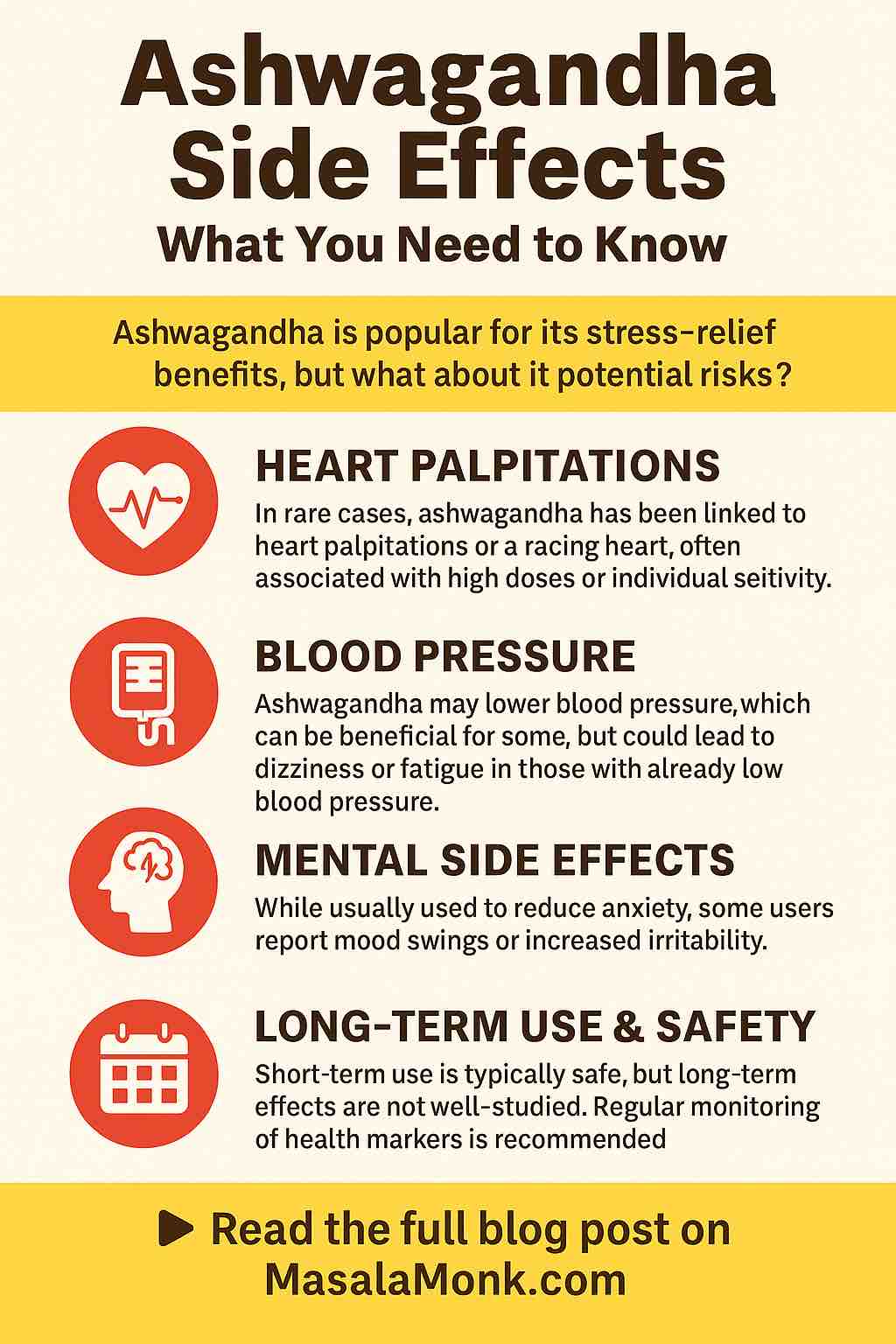
- Ashwagandha: Shown in multiple studies to lower cortisol and improve sleep and mood.
- Rhodiola Rosea: Enhances stress resilience and reduces fatigue.
- Panax Ginseng: Balances the HPA axis and reduces anxiety.
You can find these herbs in ready-made adaptogenic drinks or add powders/tinctures to smoothies, lattes, or herbal teas.
How to enjoy it: Start with one adaptogenic drink per day. Use under supervision if you’re pregnant, breastfeeding, or taking medication.
Quick Tips for Cortisol-Calming Drinks
- Consistency matters: Benefits build over time.
- Watch the sugar: High sugar can spike cortisol.
- Stay hydrated: Even mild dehydration increases cortisol.
- Avoid late-night caffeine: Choose calming herbal blends instead.
Do Read 5 Herbal Teas & Brews That Help Lower Cortisol Naturally
Cortisol Detox: Reset Your Stress Hormones Naturally
You don’t need a harsh cleanse — a simple “cortisol detox” means resetting your lifestyle with stress-lowering choices:
- Drink plenty of water (add electrolytes if needed).
- Focus on anti-inflammatory foods like turmeric, ginger, and omega-3s.
- Try adaptogens like ashwagandha or rhodiola for stress resilience.
- Reduce alcohol, caffeine, and processed foods.
- Prioritize rest and recovery with 7–8 hours of sleep.
💡 Cortisol Belly Explained: Chronic high cortisol pushes your body to store fat in the abdominal area, even if the rest of your body is lean. Managing stress, diet, and sleep can help reverse this effect.
You might like to read: Fasting and Cortisol: Is Intermittent Fasting Stressing Your Hormones?
Final Sip: Nourish to Flourish
Stress may be unavoidable, but being chronically overwhelmed doesn’t have to be your normal. Choosing beverages that support your body’s stress response is a small, daily act of self-care that adds up. Whether it’s a warm mug of green tea, a fizzy probiotic shot, or a soothing cup of chamomile before bed, your drink choices can help you lower cortisol and lift your mood.
🌟 Want more practical tips, research-backed strategies, and delicious recipes to support your well-being?
Read the full guide on cortisol-lowering nutrition here: masalamonk.com/diet-strategies-to-lower-cortisol-levels
🔗 Related Reads on Cortisol, Stress Management, and Hormonal Health
Explore more in-depth insights on how cortisol impacts your stress levels, metabolism, mood, and overall well-being:
- How Coffee Affects Cortisol, Stress, and Weight Management
Learn how caffeine and timing of your daily coffee can influence cortisol levels and body weight. - Can Drinking Tea Help Reduce Cortisol Naturally?
Discover the calming effects of herbal and green teas on stress hormone regulation. - Top 5 Cortisol-Lowering Drinks to Reduce Stress and Anxiety
Sip your way to serenity with these science-backed calming beverages. - Best Diet Strategies to Lower Cortisol Levels Naturally
A nutritionist-informed guide to eating in a way that supports balanced cortisol and mental well-being. - Omega-3 and Cortisol: How Fish Oil Supports Stress Hormone Balance
Understand how essential fatty acids like EPA and DHA help manage stress responses. - 5 Common Foods That Spike Cortisol and Increase Stress
Avoid these dietary culprits that may elevate your cortisol and disrupt hormonal balance. - 10 Warning Signs of High Cortisol in Women
A detailed look at symptoms and hormonal patterns specific to females with elevated cortisol. - 5 Foods That Naturally Help Lower Cortisol and Promote Calm
Add these anti-stress superfoods to your diet for better mood and lower cortisol levels.
✅ Frequently Asked Questions (FAQs)
1. What is cortisol, and why should I be concerned about it?
Cortisol is the body’s primary stress hormone, released by the adrenal glands. While it’s vital for managing acute stress and energy, chronically high cortisol levels can contribute to weight gain, poor sleep, anxiety, high blood sugar, and immune dysfunction.
2. Can drinks really help lower cortisol levels naturally?
Yes. Certain beverages—especially those rich in antioxidants, adaptogens, L-theanine, and other calming compounds—can support cortisol regulation by reducing inflammation, improving mood, and promoting relaxation.
3. How often should I drink these cortisol-lowering beverages?
Incorporating 1–2 of these drinks into your daily routine can be beneficial. For best results, pair them with a healthy diet, stress-management techniques, and good sleep hygiene.
4. Is green tea better than coffee for managing cortisol?
Yes. While coffee can spike cortisol (especially in large amounts or when consumed on an empty stomach), green tea contains L-theanine, which has calming effects and may help blunt cortisol release—even with its small caffeine content.
5. Can I drink these beverages at any time of the day?
Most of these drinks can be consumed throughout the day, but herbal teas (like chamomile or ashwagandha) are best taken in the evening to promote relaxation and better sleep.
6. Are there any side effects to these natural drinks?
Generally, no. However, some adaptogens like ashwagandha may interact with medications or hormonal conditions, and green tea contains caffeine, which may not suit everyone. Always consult a healthcare professional if unsure.
7. What foods should I avoid if I’m trying to lower cortisol?
Avoid or limit sugary drinks, refined carbs, energy drinks, alcohol, and processed or deep-fried foods. These can spike cortisol or disrupt blood sugar, worsening stress responses.
8. Are store-bought “stress relief” drinks effective?
Some may help if they contain science-backed ingredients like L-theanine, magnesium, or herbal adaptogens. But always read labels carefully—many are high in sugar or contain stimulants that do the opposite of what you want.
9. Can I mix ingredients like ashwagandha or turmeric into my regular drinks?
Absolutely. You can add powdered ashwagandha to smoothies or golden milk, or use turmeric with black pepper and a healthy fat in warm plant-based milk for enhanced absorption and anti-inflammatory effects.
10. Is hydration important for managing cortisol?
Yes. Even mild dehydration increases cortisol levels. Alongside these cortisol-lowering drinks, make sure you’re drinking enough plain water throughout the day to support optimal hormonal balance.