Ever felt drained despite a full night’s sleep, or caught yourself craving chocolate for no obvious reason? Maybe your muscles twitch after exercise, or your stress levels run higher than usual. While we often blame sleep, caffeine, or stress itself, the underlying culprit could be something quieter: magnesium deficiency.
Magnesium is essential for over 300 biochemical reactions in the body, from keeping your heart steady to fueling muscle contractions and regulating blood sugar (NIH Fact Sheet). Yet, it’s one of the most overlooked nutrients in modern diets. Studies estimate that nearly half of U.S. adults don’t meet the daily requirement, and around 60% fall short of recommended intake (PMC). In Canada, up to 21.8% of adolescents show low serum magnesium levels (MDPI). And globally, similar patterns emerge—from Germany to South Korea, deficiency is widespread.
The consequences go beyond fatigue. Low magnesium is linked to hypertension, insulin resistance, osteoporosis, cardiovascular disease, and even mental health issues like depression (PMC; Frontiers). One recent study even found that low magnesium correlates with elevated homocysteine levels, a marker of DNA damage that increases risk for Alzheimer’s and Parkinson’s (Verywell Health).
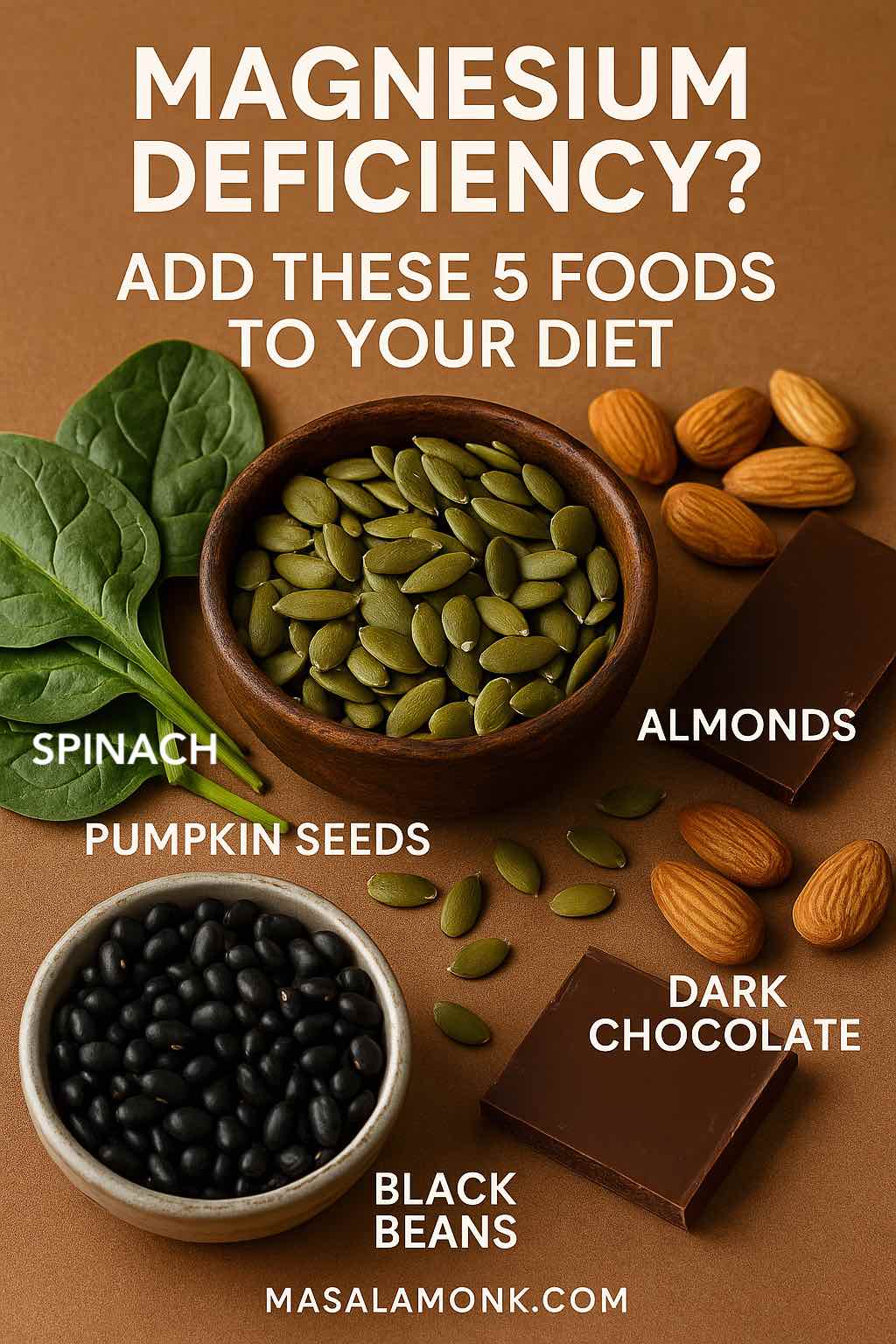
Here’s the good news: magnesium deficiency doesn’t demand exotic supplements or expensive treatments. The most effective solutions are already in your kitchen—in seeds, beans, greens, and even a square of dark chocolate. Let’s dive into the best magnesium deficiency foods and how to make them part of your daily diet.
Do Read: Magnesium Glycinate, Citrate, and Oxide – How are they different?
Magnesium Deficiency Foods: Top 5 Sources
Pumpkin Seeds: The Mineral Powerhouse
If there’s a single food that deserves the crown in the magnesium world, it’s pumpkin seeds. Just one ounce contains ~150 mg of magnesium, nearly 37% of the recommended daily allowance (Cleveland Clinic).
Pumpkin seeds—also called pepitas—have long been treasured across cultures. In Mexico, they’re ground into sauces like mole; in India, they’re blended into chutneys and trail mixes. Their earthy, nutty crunch makes them easy to sprinkle on oatmeal, salads, or yogurt bowls.
What makes pumpkin seeds particularly valuable is their nutrient synergy. Alongside magnesium, they offer zinc, iron, plant-based protein, and healthy fats. But there’s a catch: like many seeds, they contain phytates, which can block mineral absorption. The good news? Light roasting or soaking can reduce phytates and boost bioavailability (ScienceDirect).
Try this: Blend pumpkin seeds into a smoothie with spinach, banana, and coconut water for a magnesium-rich energy drink that doubles as a post-workout recovery booster.
In Mexico… pumpkin seeds—also called pepitas—have long been treasured across cultures. Need recipe ideas? You can also try Masala Monk’s nutrient-rich pumpkin-seed smoothies for a creative twist.
Spinach and Leafy Greens: More Than Iron
Spinach has long been associated with iron (thank you, Popeye), but it’s also a quiet magnesium hero. Half a cup of cooked spinach contains ~78 mg magnesium, or about 19% of daily needs (Cleveland Clinic).
Leafy greens also come with oxalates, compounds that bind to minerals and reduce absorption. Here’s the trick: cooking reduces oxalates significantly—by up to 66% in spinach—making the magnesium far more available (ACS Journal of Agricultural and Food Chemistry). That means sautéed spinach, palak paneer, or Mediterranean-style greens drizzled with olive oil aren’t just delicious, they’re smarter choices than raw salads when it comes to magnesium intake.

Other leafy greens worth mentioning include Swiss chard, kale, and collard greens—all packed with magnesium and calcium.
Try this: Toss cooked spinach with garlic, olive oil, and a squeeze of lemon. The vitamin C enhances mineral absorption while balancing the flavor.
Sautéed spinach, garlicky and bright, isn’t just a smart magnesium source—it also appears in unexpected places like a Hung-curd spinach sandwich on Masala Monk.
Legumes and Spinach pair beautifully—check out Masala Monk’s lentil-and-spinach snacks, which are both iron-rich and magnesium-forward.
Almonds and Nuts: Snackable Strength
Almonds are more than a healthy snack—they’re one of the best foods high in magnesium, offering ~80 mg per ounce. Cashews, peanuts, and Brazil nuts also contribute meaningful amounts.
Nuts fit seamlessly into daily routines: a handful on the go, almond butter on toast, or almond milk in coffee. Beyond magnesium, they supply vitamin E, protein, and heart-healthy fats. Read more about Almonds Nutrition Facts 100g & Glycemic Index Impact.
Nut-based cuisines highlight their versatility. Indian sweets often use almonds, Middle Eastern dishes use tahini (sesame paste), and Mediterranean diets feature nut-based sauces.
Keep in mind portion size: nuts are calorie-dense. Pair them with fruit or whole grains for balanced snacks that deliver both energy and minerals.
Try this: Make an almond-date energy ball with rolled oats and cacao powder for a magnesium-packed afternoon pick-me-up.
Almonds are easy to snack on—or blend into one of Masala Monk’s nut-infused smoothie recipes to boost both flavor and minerals. Pairing almonds with chia seeds makes a magnesium-rich breakfast; try one of Masala Monk’s almond-and-chia smoothies for a tasty twist.
Black Beans and Legumes: Comforting Protein + Minerals
Legumes may not get the same spotlight as trendy seeds, but they’re a cornerstone of a diet for magnesium deficiency. Half a cup of cooked black beans contains ~60 mg magnesium (Cleveland Clinic). Lentils, chickpeas, and soybeans (edamame) also rank high.
Globally, legumes are cultural staples—whether it’s Indian dals, Latin American bean stews, or Middle Eastern hummus. They bring not just magnesium but also plant-based protein and fiber, making them ideal for energy and digestion.
Absorption can be tricky because beans are rich in phytates. The traditional wisdom of soaking, sprouting, and slow cooking proves its worth—research shows these methods reduce phytates and enhance mineral bioavailability (ResearchGate).
Try this: A black bean chili topped with avocado and pumpkin seeds delivers a magnesium trifecta in one hearty bowl.
Dark Chocolate and Cacao: Sweet Stress Relief
Yes, your late-night chocolate craving may be your body’s cry for magnesium. A single ounce of 70–85% dark chocolate contains ~64 mg magnesium, about 16% of daily needs. Cocoa powder adds ~26 mg per tablespoon.
Dark chocolate is also rich in flavonoids, antioxidants that support heart health and stress resilience. Research suggests that cacao’s compounds may help lower cortisol, making it both a comfort food and a functional stress reliever.
Pairing matters: melted into mole sauce, blended into a cacao-banana smoothie, or savored as a simple square with nuts—dark chocolate is one of the tastiest foods to eat for low magnesium.
Try this: A warm cacao drink with almond milk before bed makes for the ultimate magnesium bedtime drink—relaxing and restorative.
Looking for a richer way to enjoy dark chocolate’s benefits? Consider Masala Monk’s chocolate-vanilla pudding—a treat that still nods to magnesium.
Beyond the Top 5: More Foods Good for Magnesium Deficiency
To diversify your diet for magnesium deficiency, add these everyday items:
- Chia seeds (111 mg per ounce)
- Quinoa (118 mg per cooked cup)
- Avocado (58 mg per medium fruit)
- Tofu (37 mg per half cup)
- Banana (32 mg per medium fruit)
These foods are versatile and easy to incorporate into daily meals—from breakfast bowls to dinner sides.
Chia seeds also carry magnesium— have a look at 10 Creative Chia Pudding Recipes for Every Taste from Masala Monk for a breakfast worth waking up for.
Drinks High in Magnesium and Potassium
Magnesium doesn’t just hide in foods—it also shows up in nourishing drinks.
- Cacao Hot Chocolate: A tablespoon of cocoa (~26 mg magnesium) stirred into milk with a teaspoon of blackstrap molasses (+50 mg) creates a rich, mineral-packed tonic.
- Green Electrolyte Smoothie: Blend coconut water (~60 mg magnesium per cup), spinach, banana, and chia seeds for a natural sports drink.
- Blackstrap Lemonade: Old-fashioned but effective, molasses adds not just magnesium but also iron and potassium.
Supplement powders also exist. Clinical studies show that oral magnesium supplementation reduced deficiency prevalence from 26% to just 2% (Epidemiology & Health Journal). While they can be useful, especially for people with low intake, food-first remains the most sustainable approach.
Want refreshing ways to boost both magnesium and energy? Masala Monk’s matcha-spinach green powers are nutrient-rich and vibrant.
Foods High in Magnesium Chart
| Food (serving) | Magnesium (mg) | % Daily Value |
|---|---|---|
| Pumpkin seeds (1 oz) | 150 mg | 37% |
| Chia seeds (1 oz) | 111 mg | 28% |
| Almonds (1 oz) | 80 mg | 20% |
| Spinach (½ cup cooked) | 78 mg | 19% |
| Black beans (½ cup) | 60 mg | 15% |
| Dark chocolate (1 oz) | 64 mg | 16% |
| Avocado (1 medium) | 58 mg | 15% |
| Quinoa (1 cup cooked) | 118 mg | 30% |
| Tofu (½ cup) | 37 mg | 9% |
| Banana (1 medium) | 32 mg | 8% |
(Source: Cleveland Clinic)
Foods for Magnesium Deficiency: A 1-Day Meal Plan
Here’s how to build a diet for magnesium deficiency with simple meals:
- Breakfast: Cacao-banana smoothie with almond butter (~180 mg).
- Lunch: Quinoa salad with black beans, spinach, avocado, and pumpkin seeds (~250 mg).
- Snack: Almond-date energy balls with dark chocolate (~120 mg).
- Dinner: Lentil dal with sautéed greens and whole wheat roti (~200 mg).
- Evening Drink: Warm cacao with molasses (~75 mg).
Total: ~825 mg magnesium—well above the daily requirement (400–420 mg for men, 310–320 mg for women).
How to Increase Your Magnesium Intake Naturally
- Cook smart: Boiling spinach and beans reduces oxalates and phytates by up to 77%, unlocking minerals (ResearchGate).
- Soak and sprout: Traditional practices improve absorption (ScienceDirect).
- Pair foods wisely: Vitamin C-rich foods (like lemon or tomatoes) enhance mineral uptake.
- Spread intake: Instead of one giant serving, eat magnesium-rich foods throughout the day.
Also Read: What is Magnesium and Why is it Important?
Magnesium Beyond the Plate: Flakes and Butters
Bath soaks with magnesium flakes and topical butters are popular for relaxation. While research shows limited evidence of absorption through the skin, many people find them calming (Ancient Minerals). They can be part of a bedtime ritual, but they’re not substitutes for food.
Conclusion: From Deficiency to Vitality
Magnesium deficiency is far from rare—it’s a silent epidemic with wide-ranging effects, from energy and mood to long-term disease risk. But the fix doesn’t require fancy pills or expensive powders. It starts with food: a handful of seeds, a bowl of beans, a plate of greens, a square of chocolate.
By focusing on these magnesium deficiency foods—and complementing them with nourishing drinks—you can restore balance, energy, and resilience. It’s not just about avoiding deficiency; it’s about thriving.
Your next step? Sprinkle pumpkin seeds on your breakfast, sauté spinach for dinner, sip cacao at night. Small daily choices add up to a mineral-rich life.
Frequently Asked Questions About Magnesium Deficiency Foods
1. What are the first signs of low magnesium?
To begin with, symptoms can be subtle. You might notice muscle twitches, restless sleep, headaches, or fatigue creeping in. Over time, low magnesium may also show up as anxiety, poor concentration, or chocolate cravings—yes, that sweet tooth may be your body’s way of asking for minerals.
2. Which foods are best for magnesium deficiency?
In short, the most powerful magnesium deficiency foods are pumpkin seeds, spinach, almonds, black beans, and dark chocolate. They’re nutrient-dense and easy to add to daily meals. What’s more, you can round out your diet with quinoa, chia seeds, avocado, tofu, and bananas. Together, they provide a natural, balanced approach to restoring your levels.
3. What fruits are high in magnesium?
Although fruits aren’t the richest sources, some still help. Avocados top the list with ~58 mg per medium fruit. Bananas contribute ~32 mg, while figs and raspberries also contain modest amounts. So, while fruits alone won’t cover your needs, they play a supportive role—especially when paired with nuts or seeds.
4. Can drinks really boost my magnesium intake?
Absolutely. For example, a cacao hot chocolate with molasses can give you 70–80 mg in a single cup. Likewise, a coconut water green smoothie blends hydration with magnesium and potassium for an electrolyte lift. And here’s the good news: these drinks don’t just add minerals, they also make your daily routine feel comforting and enjoyable.
5. How can I increase magnesium absorption from foods?
Here’s where small changes matter. Cooking greens like spinach lowers oxalates, which block absorption. Soaking or sprouting beans and seeds makes minerals more available. And spreading your intake throughout the day works better than eating one large magnesium-rich meal. In other words, it’s not just what you eat—it’s how you prepare and enjoy it.
6. Do magnesium flakes or body butters help with deficiency?
To put it simply, they’re relaxing but not a reliable cure. Research shows limited evidence for magnesium being absorbed through the skin. Still, a warm bath with magnesium flakes or a calming magnesium butter massage can reduce stress and prepare your body for sleep. Think of them as complementary rituals—not replacements for food.
7. Who is most at risk of magnesium deficiency?
In fact, certain groups need to be extra mindful. Older adults, people with diabetes, heavy drinkers, and those following restrictive diets (like strict keto) often run low. Pregnant women also require higher amounts. For these groups especially, focusing on foods to eat for low magnesium can make a big difference.
8. What’s the easiest way to start getting more magnesium today?
Start simple. Add a handful of pumpkin seeds to your breakfast, sauté spinach with your dinner, and swap one evening dessert for a square of dark chocolate. As a bonus, try a magnesium bedtime drink like warm cacao with almond milk. These small steps add up, turning your daily meals into a steady source of calm and energy.