You want to donate—and you want that calm “you’re good to go” at screening. Food can’t rewrite biology overnight, but if you choose well and time things right, it can give you a steady tailwind. This guide breaks down iron rich foods for blood donation in the only way that matters on a busy week: plain servings with actual iron numbers, quick pairings that improve absorption, and a realistic answer to the question everyone asks—is food alone enough, or do I need a supplement?
When you’re ready to double-check day-of rules (hemoglobin cut-offs, plasma protein checks, cadence), hop to our plain-English explainer—Can You Donate Plasma if You’re Anemic or Have Low Iron?—then come back here to plan the meals that make that “yes” more likely.
⚠️ Educational Information Only
This article is for general education about iron, blood donation, and plasma eligibility. It is not medical advice and does not replace consultation with a qualified health professional. Donation rules, hemoglobin thresholds, and iron requirements differ by country and by program. Always check your local blood service’s guidelines and talk to your clinician before changing diet, taking supplements, or booking a donation.
Why Iron Matters Before You Give Blood (and What Clinics Actually Check)
As a quick refresher, iron is a core part of hemoglobin, the protein in red blood cells that carries oxygen. On donation day, most services measure hemoglobin; some plasma programs also check total protein before apheresis (typically acceptable 6.0–9.0 g/dL in the U.S.). That means you’re optimizing your day-of hemoglobin with the foods and habits below. Your deeper iron stores (often tracked as ferritin) change more slowly, which is why consistency over a few weeks beats one heroic salad.
If you’d like to see the difference between iron types, common inhibitors, and safety notes in one place, bookmark these readable, authoritative primers: the NIH’s Iron Fact Sheet for Consumers, American Red Cross blood donor iron guidance, and the WHO overview on iron deficiency.
(For a friendly overview on our website, see Iron-rich vegetables that boost hemoglobin.)
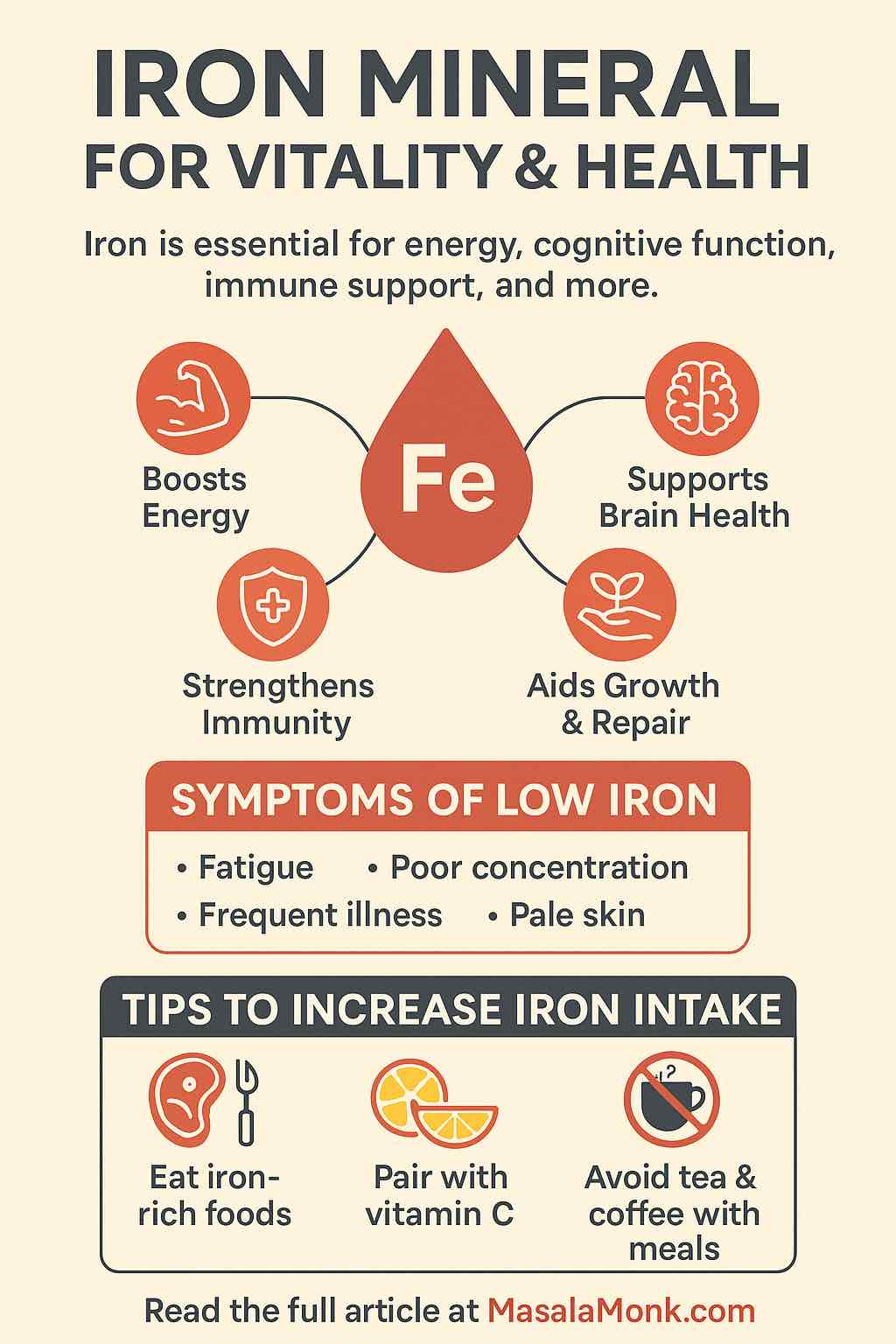
The Two Kinds of Iron—And the One Habit That Changes Everything
Dietary iron arrives in two forms:
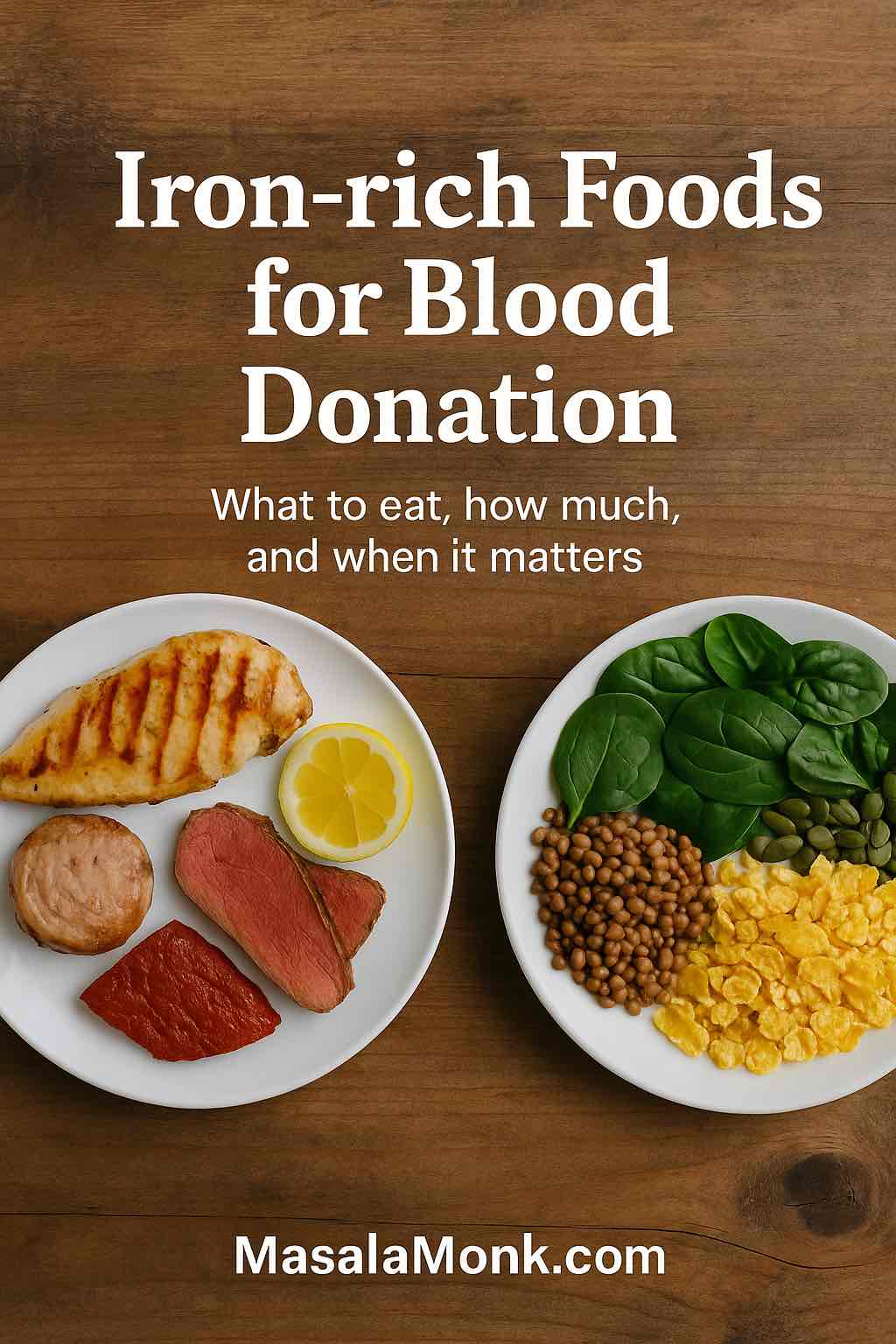
- Heme iron (animal sources): beef, chicken, turkey, tuna/salmon, liver. It’s absorbed more easily.
- Non-heme iron (plant & fortified foods): lentils, beans, chickpeas, tofu/tempeh, spinach, iron-fortified cereals and oats. It needs a little help.
That help is vitamin C. Pair plant iron with peppers, tomatoes, citrus, kiwi, berries, or amla in the same meal. Just as important, keep tea/coffee and big calcium servings away from the iron-focused plate; both can blunt absorption if they show up at the same time. If you want more depth on the why, the NIH sheet above is clear and practical.
Explore: Fight Anemia and Boost Hemoglobin: 10 High Iron Shakes & Smoothie Ideas
How Much Iron Is in Real Food? (Serving-by-Serving Numbers)
Let’s talk grams and cups, not vibes. Use these as building blocks while you assemble iron rich foods for blood donation across your week.
Top movers (one of these can anchor a day):
- Fortified breakfast cereal (100% Daily Value): ~18 mg per labeled serving. Check the back of the box; many mainstream cereals still hit 18 mg.
- White beans, canned, 1 cup: ~8 mg.
- Oysters, cooked, 3 oz: ~8 mg.
- Beef liver, cooked, 3 oz: ~5 mg.
Everyday staples (stack two or three):
- Lentils, cooked, 1 cup: ~6.6 mg.
- Spinach, cooked, 1 cup: ~6 mg (pair with vitamin C for better uptake).
- Tofu, firm, 1 cup: ~6 mg.
- Kidney/black beans, 1 cup: ~4 mg.
- Canned tuna, 3 oz: ~1–1.4 mg.
- Pumpkin seeds, 1 oz (28 g): ~2–2.5 mg.
Quiet helpers:
- Cast-iron cookware: tomato-rich dishes (chili, dal, sauces) can pick up extra iron during cooking. It’s not a miracle, but over months it nudges the needle.
- Citrus/peppers/tomatoes/berries: these are your vitamin-C “keys” that unlock non-heme iron absorption. Pair plant iron with ~75–100 mg vitamin C in the same meal (½ bell pepper, a kiwi, or a small orange does it); keep tea/coffee and big calcium servings 90+ minutes away.

For quick label lookups and recipe planning, USDA FoodData Central is gold; it’s searchable, detailed, and free.
Sources: NIH Table 2 + USDA FoodData Central.
Two Honest Paths to “Ready to Donate”
Because readers ask this bluntly, let’s answer it the same way.
Path A — You were close to the threshold
- Goal: Build days that deliver ~18–25 mg iron on paper, protect absorption, and keep caffeine/calcium away from the iron meal.
- Timeline: Over 2–4 weeks, many borderline donors see hemoglobin drift up modestly—enough to clear day-of checks, especially if starting with plasma.
- Why it works: Repetition. You eat two default meals daily that are iron-forward, vitamin-C paired, and timing-smart. You’re stacking small wins.
Path B — You were clearly below the line
- Goal: Discuss a short course of low-dose elemental iron with your clinician (frequent-donor guidance often falls around 18–38 mg/day for a defined window), plus the same food pattern as Path A.
- Timeline: With oral iron therapy, a ~1 g/dL hemoglobin rise in ~4 weeks is a common response; ~2 g/dL in 3–4 weeks is an optimal textbook rise.
- Why it works: The supplement does the heavy lifting; food makes the result stick so you don’t slide back between donations.
If you’re weighing plasma vs whole blood for your return, remember: plasma returns your red cells (smaller iron hit), though some programs also check total protein and enforce spacing. For U.S. readers, you can confirm spacing and protein ranges on the eCFR for Source Plasma and donor protein requirement pages.
Whenever eligibility—rather than food—is your main question, use the canonical in-house reference: Can You Donate Plasma if You’re Anemic or Have Low Iron?
Iron-Rich Foods for Giving Blood (Omnivore Day Plan That Actually Fits in a Workweek)
Think practical, not perfect. Here’s a single day you can repeat (and rotate ingredients) to keep momentum. It’s deliberately simple and designed around iron rich foods for blood donation.
Breakfast
- Fortified cereal (100% DV): ~18 mg + berries or orange segments for vitamin C.
- Coffee/tea: hold for 90 minutes; enjoy it mid-morning.
Lunch
- Lentil bowl, 1 cup: ~6.6 mg, with tomatoes and peppers, olive oil, herbs, and a lemon squeeze.
- Side of citrus or kiwi.
Dinner
- Chicken thighs or tuna (3–4 oz: ~1–1.4 mg) over greens; add sautéed spinach (1 cup cooked: ~6 mg).
- Bright finish: lemon, salsa, or peppers.
Evening snack (optional)
- Pumpkin seeds, 1 oz: ~2–2.5 mg or hummus with chopped peppers.
On paper: ~29–33 mg. With mixed-diet absorption, that might net 4–6 mg—steady enough for maintenance and a slow rise.
⚠️ Educational Information Only
This article is for general education about iron, blood donation, and plasma eligibility. It is not medical advice and does not replace consultation with a qualified health professional. Donation rules, hemoglobin thresholds, and iron requirements differ by country and by program. Always check your local blood service’s guidelines and talk to your clinician before changing diet, taking supplements, or booking a donation.
Iron-Rich Foods for Blood Donation (Plant-Forward Day That Still Hits the Numbers)
You don’t need meat to donate comfortably. You need plant iron + vitamin C + timing.
Breakfast
- Fortified oats/cereal (check label; many provide 8–18 mg).
- Add strawberries/kiwi for vitamin C.
Lunch
- Chana masala (1 cup: ~4–5 mg) + peppers and tomatoes; finish with lemon.
- Roasted chickpeas on the side.
Dinner
- Tofu, 1 cup: ~6 mg, and spinach, 1 cup cooked: ~6 mg, in a tomato-rich curry.
- Rice, quinoa, or millet for comfort.
Snack
- Pumpkin seeds, 1 oz: ~2–2.5 mg.
Caffeine & calcium
- Keep both away from iron plates; enjoy coffee/tea between meals, and schedule calcium tablets for another part of the day.
On paper: 22–28 mg; with diligent vitamin-C pairings and clean timing, you raise the odds of absorbing enough to climb—slowly but surely.
Read More: Iron Deficiency Symptoms & Top 10 Vegan Iron Rich Foods That Can Help
A Week-Out Planner (So the Night Before Isn’t a Scramble)
Because the calendar matters, here’s a Saturday-morning donor template. Shift days as needed.
Mon–Wed (foundation)
- Breakfast: fortified cereal + berries; pumpkin seed sprinkle.
- Lunch: lentil or bean bowls with peppers/tomatoes; lemon-tahini.
- Dinner: rotate dal with spinach, tofu-pepper stir-fry, and tuna + tomato salsa.
- Snacks: hummus + veg; citrus; roasted chickpeas.
- Habit: coffee mid-morning; put yogurt/cheese away from iron meals.
Thu–Fri (tighten up)
- Keep the pattern; if you eat meat/fish, add one heme dinner (chicken thighs or salmon).
- If plant-based, double down on spinach + legumes + citrus.
- Hydrate; don’t oversalt dinner the night before.
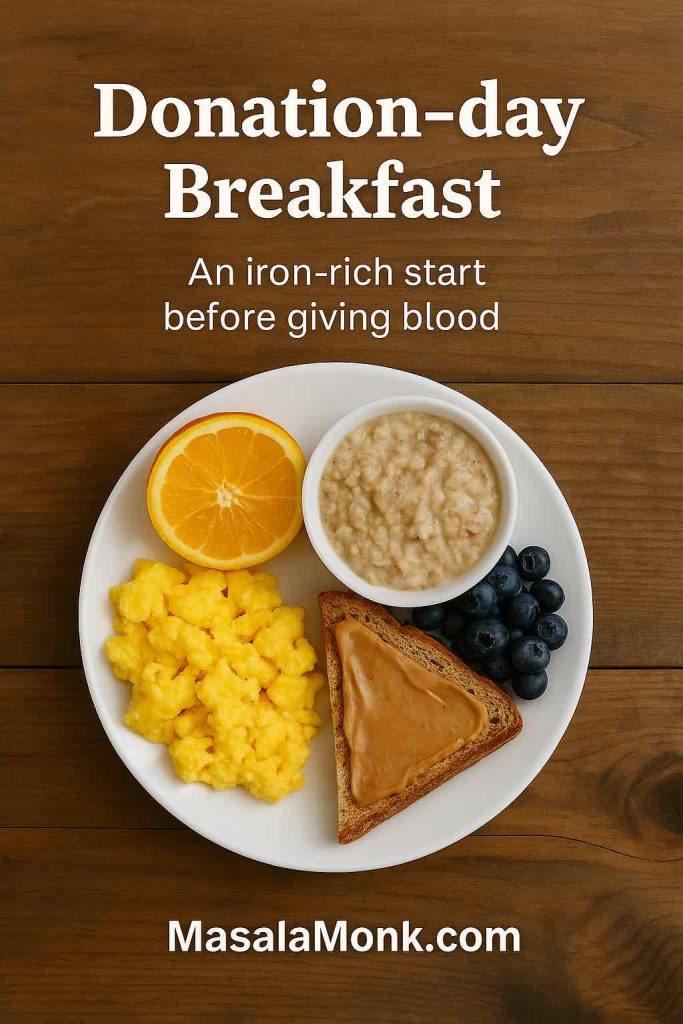
Sat (donation day)
- Light breakfast you trust: fortified cereal + berries, or chickpea-pepper salad, or eggs/tofu + tomatoes.
- Coffee after, not with.
- Pack a steady snack for later (banana, trail mix with pumpkin seeds).
Sat night–Sun (recovery)
- Keep meals iron-positive: soups, beans, greens, fish/chicken or tofu/tempeh, with citrus and peppers.
- Sleep well; note how your body responds.
Explore More: Iron Deficiency Anemia Symptoms: 15 Signs You Are Iron Deficient
Can Food Alone Raise Hemoglobin Enough to Pass Screening?
If you were borderline, yes—very often—if you give it 2–4 weeks and protect absorption. That means getting ~18–25 mg daily on paper, pairing plant iron with vitamin C, and kicking caffeine and big calcium servings to another time. Many donors clear the line this way, especially if they start back with plasma.
If you were clearly low, food alone is usually too slow. In that case, combining short, low-dose elemental iron (per clinician guidance) with the same food pattern is the predictable path back. The supplement corrects; your meals keep you there. For a simple, country-by-country sense check before you book your return, open our eligibility guide.
Iron Level to Donate Blood vs Iron Level to Donate Plasma (Plain English Only)
People often seek “iron level to donate blood” or “iron level to donate plasma,” but the decision on the day is almost always about hemoglobin—your oxygen-carrying capacity right now. For whole blood, many services also have sex-specific cut-offs. For plasma, red cells are returned, though some programs check total protein and enforce spacing between sessions. If you like to verify details straight from the source, these pages are tidy and current:
- American Red Cross: hemoglobin minimums and frequent-donor iron guidance (start at their donor iron page and eligibility sections).
- Canadian Blood Services: practical explainers on hemoglobin & iron for donors.
- NHS Blood and Transplant (UK): clear thresholds and haemoglobin and iron guidance.
- Australian Red Cross Lifeblood: accessible pieces on plasma and iron-aware donation.
- U.S. plasma spacing/protein: eCFR rules for spacing and donor protein checks.
When you just want the bottom line without clicking around, lean on our in-house explainer—Can You Donate Plasma if You’re Anemic or Have Low Iron?—and then return to this page to keep your meals humming.
⚠️ Educational Information Only
This article is for general education about iron, blood donation, and plasma eligibility. It is not medical advice and does not replace consultation with a qualified health professional. Donation rules, hemoglobin thresholds, and iron requirements differ by country and by program. Always check your local blood service’s guidelines and talk to your clinician before changing diet, taking supplements, or booking a donation.
Iron-Rich Foods for Blood Donation: Cultural Plates You Already Love
Because food sticks when it tastes like home, here are familiar patterns that quietly deliver iron rich foods for blood donation:
- Indian: chana masala with tomatoes; rajma; palak dal; lemon on grilled fish; poha with peas and a squeeze of lime; amla on the side.
- Mediterranean: chickpea-pepper salads; lentil-tomato soups; sardines or tuna on toast with lemon; tomato-pepper shakshuka.
- East/Southeast Asian-leaning: tofu/bok choy stir-fries; tempeh with sambal and lime; salmon with ginger, scallion, and citrus.
- Latin-inspired: black beans with peppers and pico de gallo; beef-and-bean picadillo with tomato; lime-forward salsas over everything.
Different cuisines, same pattern: iron + vitamin C + timing.
Do Read: Revitalizing Recipes for Iron Deficiency: Nourish Your Body Naturally
Cooking Moves That Help Without Thinking About Them
- Cook tomato-forward dishes in cast iron. You’ll likely get a small iron lift meal after meal—no extra effort.
- Finish with acidity. Lemon, lime, salsa, or a tomato-pepper relish at the table are easy vitamin-C boosts.
- Batch and freeze. Chili, dal, and bean soups mean your plan survives the Wednesday evening you’d otherwise phone in.
“How Much Should I Eat to Reach the Target?”
Here’s an easy equivalence for a typical 18–25 mg day (on paper). You can pick one from the top row and two from the middle row, then add whatever protein and vitamin-C sides you like.
Pick one (anchor):
- Fortified cereal (100% DV) → 18 mg
- White beans 1 cup → 8 mg
- Oysters 3 oz → 8 mg
Pick two (supporting):
- Lentils 1 cup → 6.6 mg
- Spinach 1 cup cooked → ~6 mg
- Tofu 1 cup → ~6 mg
- Kidney/black beans 1 cup → ~4 mg
Add protein/boosters:
- Chicken/turkey 3–4 oz → ~1 mg (plus a modest “meat factor” that improves plant-iron uptake)
- Tuna 3 oz → ~1–1.4 mg
- Pumpkin seeds 1 oz → ~2–2.5 mg
- Vitamin-C side (peppers, tomatoes, citrus, berries) → better absorption
Now, because we’re aiming for iron rich foods for blood donation and absorption, remember the automatics: move coffee/tea between meals, and park big dairy servings and calcium tablets elsewhere in the day.
For a smart crunch, see our post on pumpkin seed benefits.
If You Were Deferred: A Calm, Doable Reset
First, find out what was low—hemoglobin, protein (for some plasma programs), or something else. Then pick Path A or Path B from above. Finally, hard-wire two dinners and one breakfast you can repeat with your eyes closed. Put a lemon next to your salt; it’ll remind you to finish plates with a squeeze. If you’re often on the go, keep a jar of roasted peppers or a quick tomato relish in the fridge; it turns any bean, lentil, tofu, or tuna dish into a vitamin-C-paired meal in seconds.
If you’re unsure whether to try plasma or whole blood first on your return, use our step-by-step eligibility guide and start with the gentler option your clinic confirms you qualify for today.
Iron-Rich Foods for Blood Donation: Your Takeaway
At this point you’ve got everything you need: actual serving amounts, the pairings that make iron count, the timing that stops good meals from going to waste, and a clear sense of what’s possible on food alone. More importantly, you’ve seen how to turn iron rich foods for blood donation into a pattern you hardly have to think about: two defaults a day, a couple of bright finishes, caffeine between meals, and—if needed—a short, clinician-guided supplement to get over the hump.
So choose your anchors, set your week, and book your screening when you feel steady. And when you want the exact cut-offs and donation rhythm for your country, keep this at hand: Can You Donate Plasma if You’re Anemic or Have Low Iron?.
That way, you focus on cooking and consistency—because that’s what gets you to “yes.”
Notes & disclaimers (reader-first)
This article is for general education. It doesn’t replace medical advice, diagnosis, or your local service’s rules. If you donate frequently or were deferred by a wide margin, talk to your clinician about a short, low-dose elemental iron plan and re-check rather than taking iron indefinitely.
FAQs on Iron Rich Foods for Blood Donation
1) What are the best iron rich foods for blood donation?
Lean heme sources like beef, chicken thighs, turkey, tuna, or salmon absorb easily; meanwhile, plant favorites—lentils, chickpeas, beans, tofu, tempeh, spinach, pumpkin seeds, and iron-fortified cereals—deliver steady non-heme iron. Pair them, moreover, with vitamin C foods (peppers, tomatoes, citrus, berries) so the iron actually absorbs.
2) How to increase iron levels for blood donation quickly yet safely?
First, repeat two iron-forward meals every day for 2–4 weeks; then, add vitamin C in the same plate; finally, keep tea/coffee and large calcium servings away from those meals. This simple rhythm usually nudges hemoglobin upward without drama.
3) What does your hemoglobin have to be to donate blood?
Because thresholds vary by service, use this rule of thumb: you must meet your local minimum hemoglobin for blood donation on the day. Practically, aim to sit a little above the cut-off so you’re not living on the edge at every visit.
4) What does your hemoglobin have to be to donate plasma?
Although plasma returns red cells, you still need to meet your center’s iron level to donate plasma, which is usually checked as same-day hemoglobin. Therefore, target a comfortable margin, not just the bare minimum.
5) Can you donate plasma with low iron?
Generally, not today. If your hemoglobin tests below the cut-off, you’ll be deferred; however, once it’s back in range—and you feel well—you can usually donate plasma again.
6) Can you donate plasma if you’re anemic?
If you’re actively anemic or trending low, most centers will say “not today.” Nevertheless, after a period of recovery—think iron-forward meals, rest, and, if recommended, a short, low-dose supplement—you can reassess eligibility.
7) What happens if you donate blood with low iron?
You risk feeling faint, recovering slowly, and sliding deeper into deficiency. Consequently, clinics defer donors with low hemoglobin to protect health first, donation second.
8) How much does hemoglobin drop after blood donation?
Typically, you’ll see a modest dip for a short period; then, with sensible spacing, iron rich foods for blood donation, and adequate sleep and hydration, most people return to baseline.
9) Iron rich foods for giving blood: what should I eat the day before?
Go for an iron-dense dinner—say, chicken thighs with peppers and tomatoes or lentil dal with spinach and lemon. Additionally, finish with a vitamin-C squeeze to boost non-heme absorption.
10) Same-day meals: what should I eat before giving blood?
Choose something light but iron-aware: fortified cereal with berries, chickpea-pepper salad with lemon, or tuna on wholegrain with tomatoes. Then, enjoy coffee or tea between meals, not alongside them.
11) Do tea and coffee really block iron?
Yes—especially for plant iron. Therefore, sip your tea or coffee at least an hour or so after your iron-focused meal; that way, you keep the benefits while avoiding the absorption hit.
12) Does calcium affect iron absorption?
Large calcium doses can blunt iron uptake when taken with the meal. So, place big dairy servings or calcium tablets away from iron plates to keep absorption on track.
13) Iron supplements for blood donors: when do they make sense?
If you donate often or were clearly below the threshold, a short, clinician-guided low-dose elemental iron course can help. Meanwhile, keep the food pattern going; diet maintains the gains once you’re back in range.
14) Is it possible to pass screening with food alone?
Sometimes—particularly if you were borderline. With two to four weeks of consistent meals, vitamin-C pairings, and smart timing, many donors clear same-day checks. However, if you were well below the cut-off, diet alone is usually too slow; supplementation may be needed.
15) Iron levels for plasma donation vs whole blood: what’s the difference?
Whole blood removes red cells, so the iron hit is larger; plasma returns red cells, so the iron hit is smaller. Even so, both look at same-day hemoglobin; some plasma programs also check total protein and enforce spacing.
16) Minimum hemoglobin for blood donation: should I aim for the exact number?
Technically you can, but practically, it’s kinder to aim above the line. Thus, you stop playing roulette at the clinic and donation day feels routine rather than risky.
17) How to increase iron levels to give blood if I’m vegetarian or vegan?
Stack plant iron (lentils, beans, chickpeas, tofu/tempeh, spinach, iron-fortified cereals) and, crucially, add vitamin C in the same bowl—peppers, tomatoes, citrus, berries. Then, separate tea/coffee and large calcium servings from those meals. Consistency, not novelty, does the work.
18) What about cast-iron cookware—does it help at all?
Yes, sometimes. Tomato-forward dishes, stews, and chilis cooked in cast iron can pick up extra iron. It’s not a miracle; yet, across months, the small boost adds up alongside your regular iron rich foods for blood donation plan.
19) Can donating blood cause anemia?
Not by itself—provided you space donations sensibly and replenish iron. However, frequent donations without recovery time can nudge stores downward. Hence the emphasis on meal patterns and, when appropriate, a short supplement.
20) Giving blood to reduce iron levels: is that a thing?
Therapeutic phlebotomy exists for iron overload conditions, but it’s medically directed and not the same as routine community donation. If you suspect high iron, you’ll need clinical evaluation rather than self-treatment.
21) How long should I follow an iron-forward plan before re-screening?
As a reasonable benchmark, give it 2–4 weeks. During that time, repeat two iron-forward meals daily, pair with vitamin C, and move caffeine and big calcium servings away from those plates. Afterward, re-check and adjust.
22) Iron level to give blood vs ferritin: which one matters for screening?
For the day-of decision, hemoglobin is the usual gatekeeper. Ferritin (your iron stores) changes more slowly; nevertheless, a steady food pattern helps both over time.
23) Can I donate blood with high ferritin or hemochromatosis?
Policies differ and usually involve medical oversight. As a donor-health rule of thumb, follow clinical guidance first; then, once cleared, consider how your situation fits the local donation framework.
24) If I was deferred, should I try plasma first next time?
Often, yes. Because plasma returns red cells, it’s a gentler step back once your same-day hemoglobin is in range. Still, pace yourself, maintain the meals, and keep an eye on how you feel after each session.
25) Bottom line—how do I get to “yes” and donate confidently?
First, identify what was low; next, run a two-to-four-week plan centered on iron rich foods for blood donation with vitamin-C pairings and smart timing; then, if needed, layer in a short, clinician-guided supplement. Finally, re-screen when you feel steady and aim to sit slightly above the minimum.
⚠️ Educational Information Only
This article is for general education about iron, blood donation, and plasma eligibility. It is not medical advice and does not replace consultation with a qualified health professional. Donation rules, hemoglobin thresholds, and iron requirements differ by country and by program. Always check your local blood service’s guidelines and talk to your clinician before changing diet, taking supplements, or booking a donation.